
Fundamentals
You may feel a profound disconnect. On one hand, you encounter compelling stories about hormonal optimization, of reclaiming vitality through protocols involving growth hormone modulators. On the other, you face a clinical reality that appears cautious, restrictive, and slow to adopt these tools.
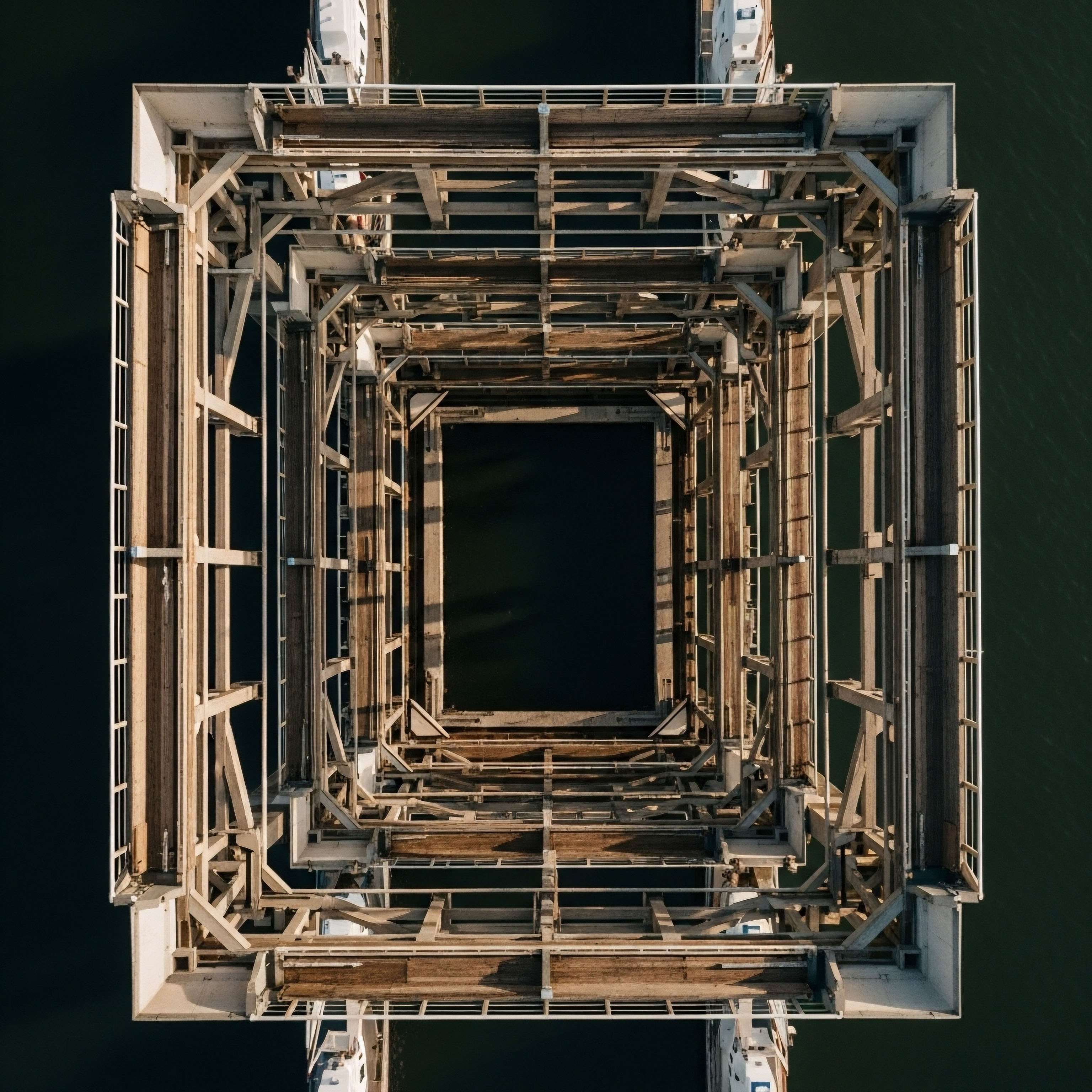
This gap between potential and practice is a direct consequence of a complex regulatory environment. Understanding this landscape begins with a foundational concept ∞ the human body’s endocrine system operates as a network of immense precision and interconnectedness. Introducing a powerful signaling molecule is an intervention that demands the highest standard of evidence.
The journey of a growth hormone modulator from a laboratory concept to a clinical tool is governed by a mandate to prove safety and specific utility. Regulatory bodies, principally the Food and Drug Administration (FDA) in the United States, function to validate that a therapeutic agent is what it claims to be, does what it claims to do, and does so without posing an unreasonable risk.
This process is intensive because the molecules in question are designed to interact with the very systems that regulate growth, metabolism, and cellular repair. An error in this system carries significant consequences.
The regulatory pathway for any therapeutic agent is a direct reflection of the biological complexity it seeks to influence.

The Body’s Internal Communication Network
Your endocrine system functions like a highly sophisticated communication network. The hypothalamic-pituitary-adrenal (HPA) and hypothalamic-pituitary-gonadal (HPG) axes are central command pathways. The hypothalamus sends signals to the pituitary gland, which in turn releases hormones that direct the function of other glands throughout the body, including the production of growth hormone (GH).
This entire process is governed by intricate feedback loops, much like a thermostat maintains a room’s temperature. A signal is sent, a hormone is released, a physiological change occurs, and that change signals back to the hypothalamus and pituitary to adjust the output.
Growth hormone modulators are substances that directly influence this delicate signaling cascade. They fall into several distinct categories, each with a unique mechanism and, consequently, a different regulatory status.
- Recombinant Human Growth Hormone (rhGH) ∞ This is a synthetic version of the growth hormone your pituitary gland produces. It is a powerful, direct-acting agent.
- Growth Hormone-Releasing Hormone (GHRH) Analogs ∞ These molecules, such as Sermorelin and Tesamorelin, mimic the body’s own GHRH. They stimulate the pituitary to produce and release its own growth hormone, working with the body’s natural pulsatile rhythm.
- Growth Hormone Secretagogues (GHS) ∞ This class includes peptides like Ipamorelin and small molecules like MK-677. They act on different receptors to stimulate the pituitary’s GH release, effectively amplifying the body’s own production signals.
- Related Peptides ∞ Other peptides, like BPC-157, are often discussed in the context of recovery and wellness. While their primary mechanism may differ, they exist within the same regulatory conversation due to their therapeutic potential and lack of formal approval.
The regulatory hurdles exist because each of these interventions represents a significant input into a finely tuned system. The core question from a regulatory standpoint is whether this input creates a predictable, beneficial, and safe outcome for a specific medical need. This validation process is what separates a scientifically proven medication from a promising but unverified compound.

Intermediate
The journey from a promising molecule to an approved clinical therapy is a structured, multi-year process defined by rigorous data collection. This pathway creates the primary distinction between growth hormone modulators available through a standard pharmacy and those sourced through other channels.
The hurdles are the sequential phases of clinical trials, each designed to answer specific questions about the drug’s behavior in the human body. Failure to clear any of these hurdles prevents a substance from being legally marketed as a drug for a specific condition.

The Gauntlet of Clinical Trials
For a growth hormone modulator to gain FDA approval, its manufacturer must sponsor a series of clinical trials. This is the most significant and costly hurdle. The process ensures that by the time a drug is available for prescription, it has a well-documented profile of its effects, side effects, and appropriate use.
A clear example is Tesamorelin (Egrifta), which was approved to treat a very specific condition ∞ excess abdominal fat in HIV-infected patients with lipodystrophy. The trials were designed to prove efficacy for that exact indication.
| Trial Phase | Primary Objective | Typical Number of Participants | Key Regulatory Question |
|---|---|---|---|
| Phase I | Safety and Dosage | 20-80 healthy volunteers | Is the molecule safe in humans at any dose? |
| Phase II | Efficacy and Side Effects | 100-300 patients with the condition | Does the molecule work for the intended condition and what are its common side effects? |
| Phase III | Large-Scale Efficacy and Safety | 1,000-3,000 patients with the condition | Is the molecule’s benefit greater than its risk in a large, diverse population? |
| Phase IV | Post-Marketing Surveillance | Thousands of patients | What are the long-term effects and are there any rare side effects? |
This structured process explains why some peptides are approved while others are not. Sermorelin and Tesamorelin successfully completed this process for specific medical conditions. In contrast, peptides like BPC-157 have not undergone this level of scrutiny in human trials, which is why the FDA has not approved them for any medical use. They remain classified as “research chemicals,” a designation that carries significant implications.

What Is the Difference between an Approved Drug and a Research Chemical?
The distinction between an FDA-approved drug and a substance sold as a “research chemical” is the central regulatory hurdle in practice. This classification dictates how a substance can be manufactured, sold, and used.
An approved drug has a verified identity and a validated purpose; a research chemical has neither in the eyes of regulators.
An FDA-approved peptide, like Tesamorelin, is manufactured in a facility compliant with Current Good Manufacturing Practices (cGMP). This ensures every batch has the same identity, purity, and strength. Its sale is tied to a specific, proven medical indication. Peptides like BPC-157 or various IGF-1 analogs are legally sold for laboratory research purposes only. Their use in humans falls outside any regulatory approval. This leads to two major hurdles for the individual seeking therapy:
- Quality and Purity Concerns ∞ The “research chemical” market is largely unregulated. The purity, concentration, and even the identity of the substance in the vial may not match the label. The FDA has noted that impurities and improper characterization of active ingredients are significant safety risks with these products.
- The Compounding Pharmacy Bridge ∞ Some physicians utilize compounding pharmacies to source peptides that are not commercially available as FDA-approved drugs. These pharmacies are regulated by state boards, not the FDA, and operate under different rules. They can, in some cases, legally create formulations for specific patients. This provides a potential avenue for access, yet the quality control can vary, and it remains a complex legal and medical area.
| Substance | Regulatory Status | Commonly Cited Hurdle | Athletic Status (WADA) |
|---|---|---|---|
| Tesamorelin (Egrifta) | FDA Approved | Approved only for HIV-associated lipodystrophy; off-label use is a clinical decision. | Prohibited |
| Sermorelin (Geref) | FDA Approved | Approved for specific diagnostic and therapeutic uses in growth hormone deficiency. | Prohibited |
| Ipamorelin / CJC-1295 | Not FDA Approved | Lack of large-scale human clinical trials; exists as a research chemical or compounded substance. | Prohibited |
| BPC-157 | Not FDA Approved | Classified as a research chemical; FDA has stated insufficient data to assess human safety. | Prohibited |
| IGF-1 LR3 | Not FDA Approved | Classified as a research chemical; not approved for human use outside of clinical trials. | Prohibited |
A final regulatory layer, particularly relevant for active adults and athletes, is the World Anti-Doping Agency (WADA). The WADA Prohibited List operates independently of the FDA. Nearly all growth hormone modulators, whether FDA-approved or not, are banned in competitive sports due to their performance-enhancing potential. This creates a distinct and absolute hurdle for any athlete subject to testing.


Academic
A sophisticated analysis of the regulatory barriers facing growth hormone modulators moves beyond the clinical trial pipeline and into two deeper, more challenging domains ∞ the molecular and the philosophical. The first is the immense technical challenge of Chemistry, Manufacturing, and Controls (CMC), which is about proving a molecule’s identity and purity. The second is the conceptual challenge of defining a treatable “disease,” particularly in the context of aging and wellness, which are processes rather than pathologies.

The Molecular Identity Hurdle Chemistry Manufacturing and Controls
For any drug to be approved, regulators demand an exhaustive CMC data package. This documentation provides an exact blueprint of the substance. It details the entire manufacturing process, stability data, and methods for identifying and quantifying the active peptide and any impurities. For complex molecules like peptides, this is a formidable hurdle. The FDA’s concern with compounded BPC-157, for instance, centers on potential impurities and the lack of data on how they might affect the human immune system.
The challenges are numerous and technically demanding:
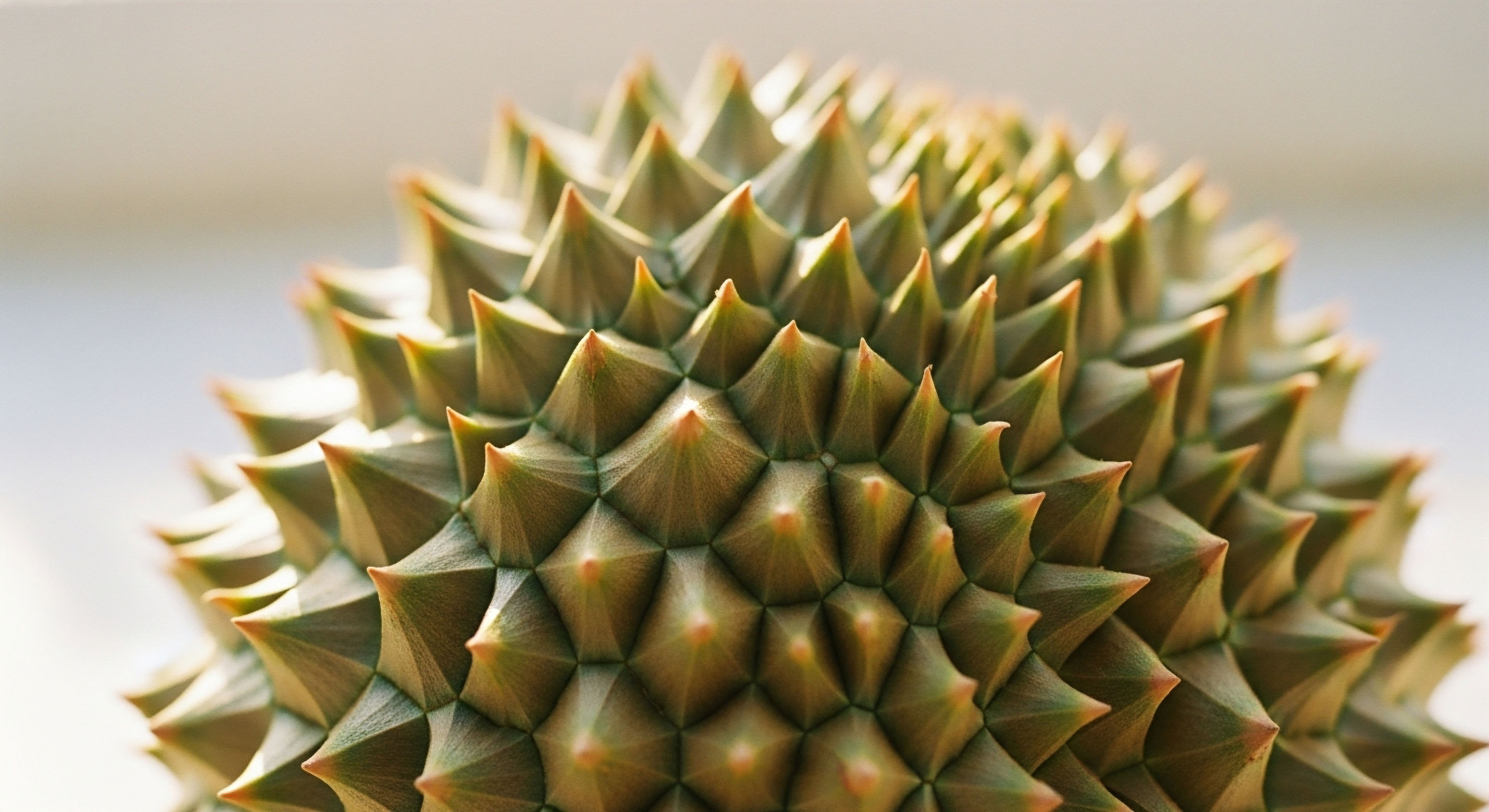
- Synthesis Byproducts ∞ Solid-phase peptide synthesis, the common method for producing these molecules, can result in deletion sequences (missing amino acids) or incomplete deprotection, creating a cocktail of closely related but functionally different peptides.
- Stereoisomers ∞ Amino acids (except glycine) are chiral. An error in synthesis can lead to the incorporation of a D-amino acid instead of the natural L-form, creating a diastereomer with a different three-dimensional shape and potentially altered biological activity or immunogenicity.
- Oxidation and Aggregation ∞ Peptides containing residues like methionine are prone to oxidation. Many peptides can also aggregate, forming dimers or larger structures that can be less effective or even trigger an immune response. Regulators require proof that the product is stable and remains in its intended monomeric form.
This obsession with molecular identity is rooted in biological reality. The specificity of a hormone or peptide’s action depends entirely on its precise structure, which dictates how it fits into its receptor. A minor structural variance can alter binding affinity, change downstream signaling, or be recognized as foreign by the immune system.
The unregulated market for research peptides bypasses this entire system of validation, presenting a material risk to the end-user. The hurdle is demonstrating to regulators, with picogram-level precision, that every single vial contains exactly what it is supposed to contain, and nothing else.
Regulatory validation of a peptide’s molecular structure is the foundation upon which all claims of safety and efficacy are built.

Why Does the FDA Distinguish between Disease Treatment and Wellness Enhancement?
The second profound hurdle is the very definition of a therapeutic indication. The FDA approves drugs to diagnose, cure, mitigate, treat, or prevent a disease. This framework is well-suited for conditions like cancer or diabetes. It is poorly suited for addressing the gradual functional decline associated with aging.
While symptoms of hormonal decline are real and measurable, “aging” itself is not classified as a disease. Therefore, a company cannot seek approval for a drug with the indication “to reverse aspects of aging.”
This creates a strategic challenge for developers of growth hormone modulators, whose most desired applications often fall into the categories of “longevity,” “enhanced recovery,” or “improved body composition.” To navigate this, manufacturers must identify a specific, recognized disease state where the peptide’s mechanism provides a clear benefit.
The approval of tesamorelin is the archetypal example. Its ability to modulate fat metabolism was applied to the distinct pathology of HIV-associated lipodystrophy, an abnormal fat distribution that is a recognized medical condition. The approval of somapacitan (Sogroya) was for Adult Growth Hormone Deficiency (AGHD), a diagnosed endocrine disorder, with the clinical endpoint being a reduction in truncal fat, a metabolic marker associated with the disease.
This “disease-centric” model forces a bifurcation. The on-label, approved use of these powerful molecules is restricted to narrow patient populations with specific diagnoses. Their application in broader wellness or age-management protocols falls into the domain of “off-label” prescribing.
While off-label use by a physician is legal and common in medicine, it places a higher burden of evidence and responsibility on the prescribing clinician. It also means that the rigorous data from Phase III trials may not directly apply to a healthier, aging population. This philosophical and structural barrier within the regulatory framework is perhaps the most significant hurdle to the widespread clinical integration of growth hormone modulators for personalized wellness and longevity protocols.

References
- Al Musaimi, Othman. “Exploring FDA-Approved Frontiers ∞ Insights into Natural and Engineered Peptide Analogues in the GLP-1, GIP, GHRH, CCK, ACTH, and α-MSH Realms.” Biomolecules, vol. 14, no. 3, 2024, p. 264. PubMed Central, doi:10.3390/biom14030264.
- “BPC 157 ∞ Science-Backed Uses, Benefits, Dosage, and Safety.” Rupa Health, 18 Feb. 2025.
- “IGF-1 LR3 vs IGF-1 DES ∞ Which Peptide Is Best for Muscle Growth and Recovery?” Swolverine, 18 Jul. 2025.
- “FDA-approved weekly subcutaneous human growth hormone debuts in US.” Pharmaceutical Technology, 1 Oct. 2020.
- U.S. Food and Drug Administration. “Substances in Compounding that May Present Significant Safety Risks.” FDA.gov.

Reflection
You now possess a clearer map of the landscape connecting the science of hormonal health to the reality of its clinical application. The hurdles you perceive are built upon a foundation of biological caution. They exist to ensure that interventions into the body’s most intricate signaling systems are both predictable and purposeful.
This knowledge itself is a form of empowerment. It moves the conversation from one of frustration with restrictions to one of understanding the questions that must be answered before a powerful tool can be used with confidence.
Your own health journey is unique. The symptoms you experience, the goals you hold, and your individual biology create a context that is entirely your own. The information presented here is a framework for understanding the broader system.
The next step is to apply this understanding to your personal context, recognizing that a path toward optimized function is one built on a partnership between your lived experience and validated clinical science. The most effective protocols are those that are both biologically sound and deeply personalized.



