

Fundamentals
The decision to explore hormonal recalibration when you are also managing an existing cardiac condition brings you to a unique intersection of your personal health narrative. It is a space where the desire to alleviate the disruptive symptoms of menopause meets the critical need to protect your cardiovascular system.
Your experience is valid, and the questions you are asking are born from a place of deep wisdom about your own body. This is a journey of profound self-awareness, where understanding the intricate biological dialogue between your hormones and your heart becomes the first step toward reclaiming vitality with confidence and precision.
To begin this exploration, we must first appreciate the foundational role that estrogen plays in a woman’s cardiovascular wellness throughout her reproductive years. Estrogen is a powerful signaling molecule that interacts with nearly every tissue in the body, including the heart and blood vessels.
It supports the flexibility of arterial walls, allowing them to expand and contract with each heartbeat, which helps regulate blood pressure. This hormone also has a favorable influence on cholesterol profiles, assisting in the maintenance of higher levels of high-density lipoprotein (HDL), the “good” cholesterol, and lower levels of low-density lipoprotein (LDL), the “bad” cholesterol. In essence, your natural hormonal state provides a baseline of cardiovascular resilience.
The menopausal transition fundamentally alters the body’s internal environment, removing a key modulator of cardiovascular health.
The onset of menopause signifies a significant shift in this protective hormonal milieu. As ovarian production of estrogen declines, the body’s systems must adapt to its relative absence. For the cardiovascular system, this change can manifest in several ways. Blood vessels may become stiffer, and the body’s ability to manage cholesterol and inflammation may be altered.
For a woman with a completely healthy heart, these changes are a natural part of the aging process that the body gradually accommodates. When an existing cardiac condition is part of the equation, the decline in endogenous estrogen removes a layer of physiological support from a system that is already under strain. This is the central challenge we must address.

The Central Question of Intervention
When we consider hormonal recalibration, such as menopausal hormone therapy, we are proposing to reintroduce specific hormones into this new biological context. The core safety consideration is understanding how these external hormones will interact with a cardiovascular system that has already undergone changes due to an underlying condition.
The environment within the blood vessels of a woman with established heart disease is different from that of a woman without it. There may be atherosclerotic plaque, a different inflammatory baseline, and altered endothelial function. Therefore, the introduction of hormone therapy requires a meticulously tailored approach, one that acknowledges the unique physiology of your body. The goal is to support your well-being without introducing new risks to your heart.

Why Individualized Assessment Is Paramount
The conversation about safety is entirely personal. It moves away from generalized statements and toward a detailed analysis of your specific health profile. This involves a comprehensive evaluation of several factors:
- The nature of your cardiac condition ∞ A history of coronary artery disease presents different considerations than a history of arrhythmia or heart failure.
- The time elapsed since menopause ∞ As we will explore, the timing of when hormone therapy is initiated appears to be a critical factor in its safety profile.
- Your overall metabolic health ∞ Factors like blood pressure, blood sugar levels, and body weight are integral to the decision-making process.
- Your personal and family history ∞ A history of blood clots or certain cancers will also inform the safest path forward.
Understanding these elements allows for a strategic, informed discussion with your healthcare provider. It transforms the question from a simple “yes or no” into a more sophisticated inquiry ∞ “What specific protocol, if any, is appropriate and safe for my unique biological system?” This is the foundation upon which all further, more detailed considerations are built.
It is a process of assembling a complete picture of your health to make decisions that honor both your immediate quality oflife and your long-term cardiovascular stability.


Intermediate
Advancing our understanding of hormonal recalibration in the context of cardiac health requires moving from foundational concepts to the clinical strategies that guide safe application. A central organizing principle in modern endocrinology and cardiology is the “timing hypothesis”.
This concept proposes that the cardiovascular effects of menopausal hormone therapy are critically dependent on when it is started relative to the onset of menopause. Initiating therapy in the early stages of postmenopause, typically within the first 10 years and before the age of 60, appears to interact with the body’s systems differently than initiation in the later postmenopausal years.
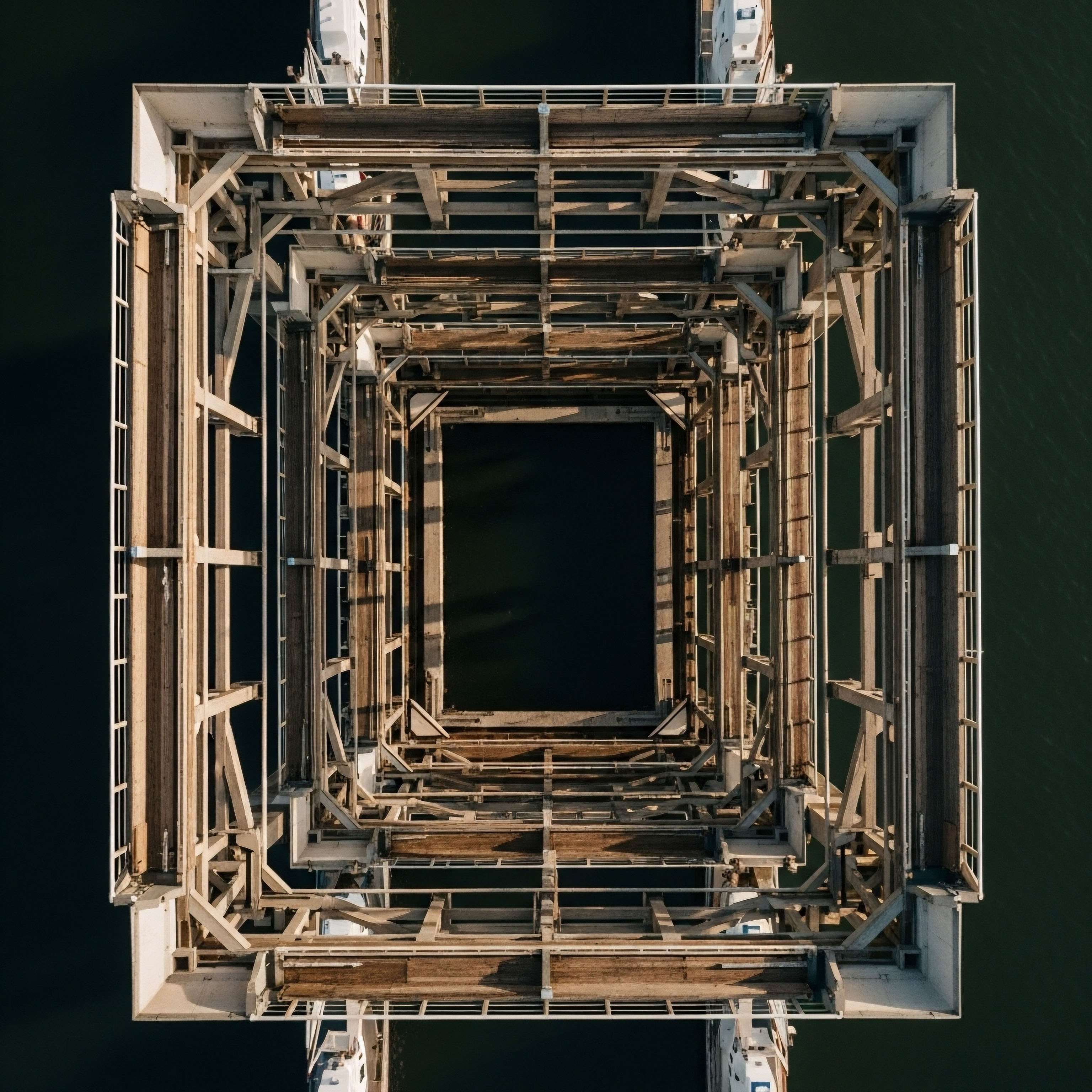
Think of the vascular system as a complex piece of biological architecture. In the years immediately following menopause, the structure is still relatively sound, even with the withdrawal of estrogen. Introducing hormone therapy at this stage can be likened to performing preventative maintenance on a fundamentally healthy building; it may help preserve the flexibility and function of the arterial walls.
Conversely, starting therapy more than a decade after menopause, particularly in a woman with established atherosclerosis, is like trying to remodel a structure that already has significant foundational weaknesses. In this scenario, the hormonal intervention may interact with existing plaque in unpredictable ways, potentially increasing inflammation and destabilizing it. This hypothesis helps explain the divergent results seen in various clinical studies and underscores why a one-size-fits-all approach is clinically inappropriate.

A Framework for Risk Stratification
Given the importance of individual context, clinicians use a risk-stratified approach to counsel women. This framework categorizes individuals based on their specific health profile to determine the appropriateness of hormone therapy. It is a systematic way to weigh the potential benefits for symptom relief against the potential cardiovascular risks. The American College of Cardiology provides guidance that helps delineate these categories.
A clear understanding of where one might fall within this framework is empowering. It provides a data-driven starting point for a conversation with your cardiologist and endocrinologist. The table below outlines the factors that contribute to this stratification, helping to clarify what an “intermediate-risk” profile might look like in a clinical setting.
| Risk Factor Category | Clinical Characteristics and Considerations |
|---|---|
| Low-Risk Profile |
This category generally includes women who are younger than 60 or within 10 years of menopause onset. They possess a 10-year atherosclerotic cardiovascular disease (ASCVD) risk score below 5%. Additional factors include having a normal body weight, well-controlled blood pressure, being physically active, and having a low personal risk for breast cancer. For these individuals, the benefits of symptom management often outweigh the potential risks. |
| Intermediate-Risk Profile |
A woman in this group may have one or more cardiovascular risk factors. These can include conditions like diabetes, hypertension, obesity, hyperlipidemia, or metabolic syndrome. A history of smoking or a sedentary lifestyle also places an individual in this category. Their 10-year ASCVD risk score typically falls between 5% and 10%. The decision-making process here is more complex, requiring a careful balancing of risks and benefits, with a strong preference for non-oral routes of administration. |
| High-Risk / Contraindicated Profile |
This group includes women for whom hormonal therapy is generally not recommended. This includes those with a history of coronary heart disease, particularly those who have had a myocardial infarction. A personal history of venous thromboembolism (VTE), such as deep vein thrombosis or pulmonary embolism, stroke, or spontaneous coronary artery dissection, are absolute contraindications for most forms of systemic hormone therapy. In these cases, the risks are considered to be unacceptably high, and non-hormonal treatment strategies are the standard of care. |

How Do Formulations and Delivery Routes Affect Safety?
The specific type of hormone and the method of delivery are critical variables in the safety equation. The blanket term “hormone replacement therapy” is imprecise because different formulations have distinct metabolic and vascular effects. The choice of estrogen and progestogen, as well as the route of administration, can significantly alter the risk profile, especially for women with cardiac considerations.
The method of hormone delivery directly influences its passage through the body and its impact on liver and clotting factors.
Oral estrogen preparations are processed by the liver before entering systemic circulation, an event known as “first-pass metabolism.” This process can increase the production of certain clotting factors, which in turn elevates the risk of venous thromboembolism (VTE). For a woman with pre-existing cardiovascular risk, this is a significant concern.
Transdermal delivery methods, such as patches, gels, or sprays, bypass this first-pass metabolism in the liver. The hormone is absorbed directly into the bloodstream, resulting in a more stable hormonal level and a lower impact on clotting factors. This makes transdermal routes a generally safer option from a cardiovascular standpoint.

The Role of Progestogen Selection
For women who have a uterus, a progestogen is included in the regimen to protect the uterine lining. The type of progestogen matters. Older, synthetic progestins have been associated in some studies with less favorable effects on blood pressure and lipid profiles compared to bioidentical or micronized progesterone.
Micronized progesterone is structurally identical to the hormone produced by the body and appears to have a more neutral effect on cardiovascular markers, making it a preferred choice in many modern protocols, especially for women with intermediate risk factors.
- Transdermal Estrogen ∞ Delivers estrogen directly to the bloodstream, minimizing the liver’s production of clotting factors and inflammatory proteins. This is often the preferred route for women with any underlying cardiovascular risk factors.
- Oral Estrogen ∞ Undergoes first-pass metabolism in the liver, which can increase the risk of VTE. Its use requires careful consideration and is generally reserved for women at very low cardiovascular risk.
- Micronized Progesterone ∞ A bioidentical hormone that appears to have a neutral or even potentially beneficial effect on the cardiovascular system compared to some synthetic progestins. It is often paired with transdermal estrogen.
- Synthetic Progestins ∞ Certain types, like medroxyprogesterone acetate (MPA) used in the large WHI study, may have less favorable effects on lipids and blood pressure. Their use is now more nuanced and selective.
The evolution in our understanding of these formulations allows for a more refined and personalized approach. By selecting specific hormones and delivery methods, clinicians can design a protocol that maximizes symptom relief while minimizing known cardiovascular risks. This level of precision is essential when navigating the complexities of hormonal health in the presence of a cardiac condition.


Academic
A sophisticated analysis of the safety considerations for hormonal recalibration in women with existing cardiac conditions requires a deep exploration of the molecular and cellular mechanisms at play within the vascular wall.
The apparent paradox observed between the cardiovascular benefits of endogenous estrogen and the potential risks of exogenous hormone therapy in certain populations can be understood through the lens of vascular biology and the pathophysiology of atherosclerosis. The decisive factor appears to be the health of the endothelium and the state of the underlying arterial substrate at the time of hormonal intervention.
In a healthy, pre-menopausal vascular environment, estrogen primarily exerts its protective effects through activation of estrogen receptor alpha (ERα) on endothelial cells. This activation stimulates the production of nitric oxide (NO), a potent vasodilator that promotes arterial relaxation, inhibits platelet aggregation, and reduces the expression of adhesion molecules that recruit inflammatory cells to the vessel wall. Estrogen also modulates a favorable lipid profile and exhibits antioxidant properties. This physiological state is one of active, hormone-driven vascular maintenance.

What Is the Mechanistic Basis of the Timing Hypothesis?
The “timing hypothesis” is more than a clinical observation; it is a reflection of a fundamental shift in the biological response of aging vascular tissue to estrogen. The transition from a protective to a potentially detrimental effect is rooted in the progression of atherosclerosis.
In the early stages of postmenopause, the vascular endothelium, while deprived of estrogen, may still retain much of its functional integrity. Introducing estrogen at this point can potentially restore some of the beneficial NO-mediated signaling and delay the progression of atherosclerosis. This aligns with findings from studies like the KEEPS trial, which showed no adverse cardiovascular effects when therapy was initiated in recently menopausal women.
However, in a woman with long-standing estrogen deficiency and established coronary artery disease, the vascular landscape is profoundly different. The endothelium is dysfunctional, and the vessel wall contains complex atherosclerotic plaques. These plaques are not inert; they are active, inflammatory sites populated by macrophages, foam cells, and smooth muscle cells.
In this altered milieu, the introduction of exogenous estrogen, particularly oral formulations, can trigger a cascade of events that promotes plaque instability. Oral estrogens are known to increase systemic levels of inflammatory markers like C-reactive protein (CRP) and matrix metalloproteinases (MMPs).
MMPs are enzymes that degrade the extracellular matrix, including the fibrous cap that sequesters the necrotic, lipid-rich core of an atherosclerotic plaque. By promoting the activity of these enzymes, estrogen can weaken the plaque’s structural integrity, making it more susceptible to rupture, which is the precipitating event for most myocardial infarctions.
This mechanism provides a compelling biological explanation for the early increase in coronary events observed in the Heart and Estrogen/progestin Replacement Study (HERS), which specifically enrolled women with pre-existing coronary heart disease.
In an already inflamed vascular environment, estrogen can paradoxically enhance the enzymatic processes that lead to atherosclerotic plaque rupture.

Thrombosis and Procoagulant Effects
The route of administration has profound implications for thrombotic risk, a critical consideration in patients with cardiac disease. Oral estrogen’s first-pass metabolism through the liver significantly increases the synthesis of procoagulant factors, including Factor VII, Factor VIII, and fibrinogen, while simultaneously decreasing levels of natural anticoagulants like antithrombin and Protein S.
This shifts the hemostatic balance toward a prothrombotic state. The Women’s Health Initiative (WHI) clearly demonstrated this effect, with a more than two-fold increased risk of venous thromboembolic events in the hormone therapy group.
Transdermal estrogen delivery circumvents this hepatic first-pass effect. By absorbing directly into the systemic circulation, it avoids the large bolus of estrogen reaching the liver, resulting in a far more neutral effect on the coagulation cascade. This distinction is paramount in clinical practice.
For a woman with any notable cardiovascular risk, the selection of a transdermal route is a primary strategy for risk mitigation. The table below details the differential effects of oral versus transdermal administration on key cardiovascular biomarkers, providing a clear rationale for this clinical preference.
| Biomarker / Pathway | Oral Estrogen Administration | Transdermal Estrogen Administration |
|---|---|---|
| Coagulation Factors |
Significantly increases procoagulant factors due to hepatic first-pass metabolism. This leads to a clinically relevant increased risk of VTE and stroke. |
Has a minimal to neutral effect on the synthesis of coagulation factors, as it bypasses the liver. This results in a substantially lower risk of thrombotic events. |
| C-Reactive Protein (CRP) |
Markedly increases levels of this key inflammatory marker, which is associated with vascular inflammation and plaque instability. |
Does not significantly increase CRP levels, suggesting a much lower pro-inflammatory effect on the vascular system. |
| Triglycerides |
Can significantly raise triglyceride levels, which is an independent risk factor for cardiovascular disease. |
Has a neutral or even slightly favorable effect on triglyceride levels. |
| Lipid Profile (HDL/LDL) |
Has a more potent effect, raising HDL cholesterol while also potentially increasing triglycerides. The net effect is complex. |
Has a less pronounced but still favorable effect on HDL and LDL cholesterol, without the negative impact on triglycerides. |

Why Was Early Observational Data so Different from Clinical Trials?
The discrepancy between early observational studies, which suggested a 35-50% reduction in coronary heart disease risk, and the results of randomized controlled trials like WHI and HERS, is a classic lesson in epidemiology.
The observational studies were subject to a “healthy user bias.” The women who opted to take hormone therapy in the 1980s and 1990s were often of higher socioeconomic status, more educated, and more proactive about their health in general. They were less likely to smoke, more likely to exercise, and had fewer underlying cardiovascular risk factors to begin with.
The hormone therapy itself was not the sole reason for their better outcomes; it was a marker for an overall healthier lifestyle.
Randomized controlled trials (RCTs) like the WHI were designed specifically to eliminate this bias. By randomly assigning healthy women to either receive hormone therapy or a placebo, the WHI provided a much clearer, unbiased assessment of the therapy’s direct effects.
The trial revealed that for the primary prevention of cardiovascular disease, the risks associated with the specific formulation used (oral conjugated equine estrogen plus medroxyprogesterone acetate) outweighed the benefits. This finding fundamentally reshaped clinical practice, moving it away from prescribing hormones for cardioprotection and toward a more focused use for the management of severe menopausal symptoms in carefully selected, low-risk women.

References
- Manson, J. E. et al. “Menopausal Hormone Therapy and Cardiovascular Disease ∞ 10 Lessons From the Women’s Health Initiative.” Circulation, vol. 127, no. 2, 2013, pp. 259-70.
- Lobo, Rogerio A. “Hormone-replacement therapy ∞ current thinking.” Nature Reviews Endocrinology, vol. 13, no. 4, 2017, pp. 220-231.
- Cho, Leslie, et al. “Menopausal Hormone Therapy and Cardiovascular Risk ∞ A Scientific Statement From the American Heart Association.” Circulation, vol. 142, no. 24, 2020, pp. e410-e427.
- Hulley, S. et al. “Randomized trial of estrogen plus progestin for secondary prevention of coronary heart disease in postmenopausal women. Heart and Estrogen/progestin Replacement Study (HERS) Research Group.” JAMA, vol. 280, no. 7, 1998, pp. 605-13.
- Rossouw, J. E. et al. “Risks and benefits of estrogen plus progestin in healthy postmenopausal women ∞ principal results From the Women’s Health Initiative randomized controlled trial.” JAMA, vol. 288, no. 3, 2002, pp. 321-33.
- Boardman, H. M. et al. “Hormone therapy for preventing cardiovascular disease in post-menopausal women.” Cochrane Database of Systematic Reviews, no. 3, 2015, CD002229.
- Hodis, H. N. & Mack, W. J. “The timing hypothesis for hormone replacement therapy ∞ a new era for menopausal medicine.” Journal of the American Geriatrics Society, vol. 62, no. 2, 2014, pp. 358-60.
- Canonico, M. et al. “Hormone therapy and venous thromboembolism among postmenopausal women ∞ impact of the route of estrogen administration and progestogens ∞ the E3N cohort study.” Circulation, vol. 115, no. 7, 2007, pp. 840-5.
Reflection
You have now journeyed through the complex biological landscape where hormonal health and cardiovascular integrity converge. You have seen how a single molecule, estrogen, can be both a guardian and a potential agitator, its effects profoundly shaped by the context of time and the underlying health of your own vascular system. This knowledge is not an endpoint. It is a toolkit for a more empowered, precise, and personalized conversation with the clinicians who partner with you on your health journey.
The information presented here is designed to illuminate the ‘why’ behind the clinical guidance you receive. It transforms abstract precautions into tangible biological reasoning. With this deeper perspective, how might your approach to your own health management evolve? What questions now seem most pressing?
Perhaps you are now thinking about the specific formulation of a hormone, the route of its delivery, or your own personal timeline since menopause began. This is the intended purpose of this exploration ∞ to shift the focus from a place of generalized concern to one of specific, informed inquiry.
Your body’s story is unique. The path forward is one of collaboration, blending your lived experience with the rigorous, data-driven insights of clinical science. The goal is to arrive at a strategy that honors the intricate wisdom of your physiology, allowing you to navigate this chapter of your life with clarity, confidence, and a renewed sense of well-being. The power lies in the precision of the questions you are now equipped to ask.

Glossary

hormonal recalibration

cardiovascular system

blood pressure

menopausal hormone therapy

atherosclerotic plaque

hormone therapy

timing hypothesis

cardiovascular disease

cardiovascular risk factors

coronary heart disease

venous thromboembolism

first-pass metabolism

cardiovascular risk

clotting factors

micronized progesterone

underlying cardiovascular risk factors

transdermal estrogen

heart disease




