
Fundamentals
You have likely experienced those subtle, yet persistent shifts in your body’s rhythms ∞ the inexplicable fatigue, the stubborn weight that resists all efforts, or the emotional fluctuations that feel disconnected from daily events. These experiences are not merely subjective sensations; they represent your body’s intricate endocrine system signaling a departure from its optimal state.
Your internal environment operates through a complex orchestra of biochemical messengers, known as hormones, which orchestrate virtually every physiological process, from metabolism and mood to vitality and regenerative capacity.
The body’s inherent design establishes a foundational operating range for these hormonal systems, a biological blueprint that dictates potential and sets boundaries. Lifestyle interventions, encompassing nutrition, physical activity, sleep, and stress mitigation, serve as powerful modulators within this pre-defined biological framework. They function to optimize the expression of your genetic potential, supporting the body’s innate drive for balance, rather than fundamentally altering its core architecture. Understanding this distinction is the initial step toward reclaiming physiological equilibrium.
Hormonal shifts, often felt as subtle changes in energy or mood, are the body’s way of communicating imbalances within its intricate endocrine network.

The Endocrine System an Internal Communication Network
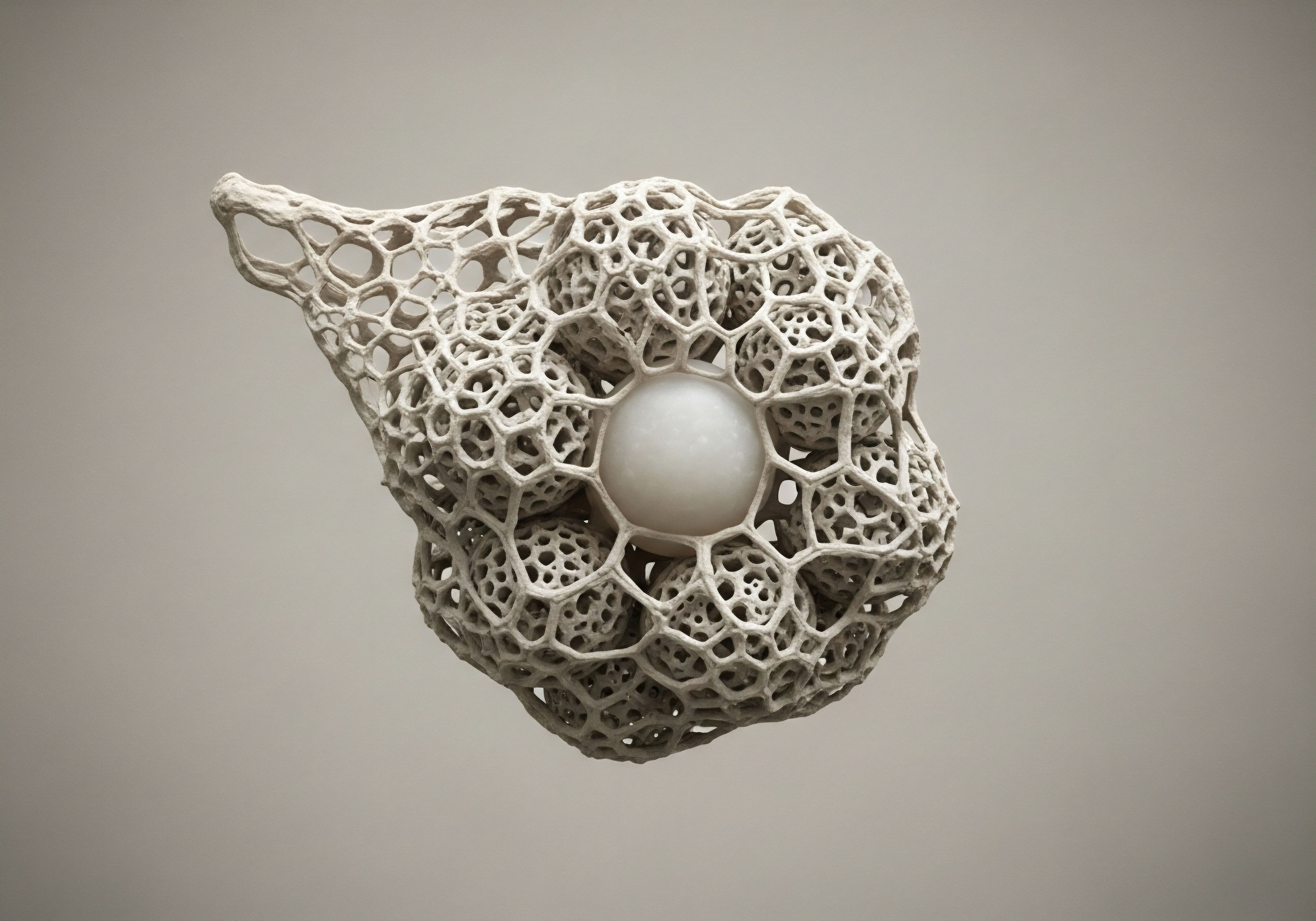
Consider the endocrine system as your body’s highly sophisticated internal communication network, where glands function as broadcasting stations and hormones serve as the vital messages. These chemical signals travel through the bloodstream, delivering precise instructions to target cells and tissues throughout your entire organism. This network maintains homeostasis, ensuring that all bodily functions remain within a tightly regulated spectrum. When lifestyle factors disrupt this delicate balance, the system responds with observable symptoms, indicating a need for recalibration.
The interconnectedness of these hormonal pathways means that an imbalance in one area frequently precipitates effects across other systems. For example, the hypothalamic-pituitary-adrenal (HPA) axis, responsible for stress response, directly influences the hypothalamic-pituitary-gonadal (HPG) axis, which governs reproductive and sexual health. This systemic interdependency means that supporting one aspect of your well-being, such as sleep quality, can positively impact numerous hormonal cascades simultaneously.


Intermediate
As we deepen our understanding of hormonal physiology, it becomes clear that lifestyle interventions represent the primary leverage points for optimizing endocrine function within your inherent biological capacity. These daily choices do not merely influence superficial well-being; they exert measurable effects on the synthesis, transport, receptor sensitivity, and degradation of hormones. Recognizing the specific mechanisms allows for a more targeted and effective approach to personal wellness.

How Lifestyle Shapes Hormonal Dynamics
Nutrition, as a cornerstone of metabolic health, provides the molecular building blocks and energetic currency for hormone production. Adequate protein intake, for example, supplies the essential amino acids necessary for peptide hormone synthesis, while healthy fats are indispensable for steroid hormone production.
Conversely, diets rich in processed foods and refined sugars can induce insulin resistance, a state where cells become less responsive to insulin, leading to elevated insulin levels and subsequent disruptions in other hormonal pathways, including those governing reproductive health.
Physical activity profoundly influences hormone receptor sensitivity, enhancing the efficiency with which cells receive and respond to hormonal signals. Regular exercise helps modulate stress hormones like cortisol, preventing chronic elevation that can suppress beneficial anabolic hormones. Sleep, often undervalued, acts as a crucial period for hormonal restoration and regulation. During deep sleep, the body releases growth hormone, vital for cellular repair and metabolic maintenance, while inadequate sleep elevates cortisol and disrupts appetite-regulating hormones such as leptin and ghrelin.
Lifestyle choices, including nutrition and physical activity, directly influence hormone production and cellular responsiveness, forming the primary tools for endocrine optimization.
Managing psychological stress also presents a direct influence on hormonal balance. Chronic stress activates the HPA axis, leading to sustained cortisol release, which can negatively affect thyroid function, sex hormone production, and metabolic processes. Techniques that promote relaxation, such as mindfulness or yoga, can attenuate this stress response, thereby supporting a more balanced hormonal milieu.

Identifying Lifestyle Intervention Limits
While lifestyle interventions offer substantial benefits, their physiological limits become apparent when underlying genetic predispositions, significant endocrine pathologies, or advanced age present more profound challenges. An individual with a strong genetic propensity for insulin resistance, for example, may find that even rigorous dietary and exercise protocols yield only partial improvements in glycemic control. Similarly, significant age-related declines in hormone production, such as those seen in andropause or menopause, often extend beyond the restorative capacity of lifestyle modifications alone.
In these circumstances, the body’s intrinsic capacity to self-regulate or restore optimal function through lifestyle alone may reach its ceiling. This threshold signifies a point where clinical interventions, precisely tailored to address specific hormonal deficiencies or dysfunctions, become a necessary consideration for restoring vitality and function.

Hormonal Impact of Lifestyle Factors
| Lifestyle Factor | Primary Hormonal Impact | Physiological Mechanism |
|---|---|---|
| Nutrition | Insulin sensitivity, sex hormone synthesis, peptide hormone production | Provides building blocks for hormones; regulates glucose metabolism and inflammation |
| Exercise | Insulin sensitivity, cortisol regulation, growth hormone release, sex hormone levels | Increases receptor sensitivity; modulates HPA axis activity; stimulates anabolic pathways |
| Sleep | Cortisol rhythm, growth hormone secretion, leptin/ghrelin balance | Restores HPA axis regulation; facilitates nocturnal GH pulses; regulates appetite signals |
| Stress Management | Cortisol levels, adrenal function, HPA axis stability | Reduces chronic sympathetic nervous system activation; supports neuroendocrine balance |


Academic
A deeper exploration into the physiological limits of lifestyle interventions requires a systems-biology perspective, acknowledging the complex interplay of genetic predispositions, receptor dynamics, and intricate feedback loops that govern endocrine function. Lifestyle choices, while potent, operate within the confines of an individual’s unique biochemical architecture, which can present inherent boundaries to optimal hormonal balance.

Genetic Predisposition and Hormonal Set Points
The concept of a “set point” for various physiological parameters, including body weight and hormonal levels, offers a lens through which to view these inherent limits. Genetic factors contribute significantly to establishing these set points, influencing everything from metabolic rate to the efficiency of hormone synthesis and receptor expression.
For example, variations in genes encoding hormone receptors can alter their binding affinity or signal transduction efficiency, meaning that even optimal hormone levels may elicit a suboptimal cellular response. This genetic blueprint dictates the maximum adaptive capacity of the endocrine system to lifestyle adjustments.
Hormonal resistance, such as insulin resistance or leptin resistance, exemplifies a critical physiological limit. While lifestyle factors like diet and exercise can improve insulin sensitivity, a persistent genetic component or prolonged exposure to obesogenic environments can lead to a recalibration of the body’s set point, making further lifestyle-driven improvements challenging. In such cases, the body actively defends a new, less optimal hormonal state, illustrating the profound influence of intrinsic biological mechanisms.
Genetic factors establish inherent set points for hormonal balance, defining the boundaries within which lifestyle interventions can effectively operate.

Advanced Clinical Interventions Addressing Physiological Limits
When lifestyle interventions reach their inherent physiological limits, targeted clinical protocols offer a precise means to recalibrate endocrine function. These interventions aim to either directly supplement deficient hormones or modulate the body’s endogenous production and responsiveness, moving beyond what lifestyle alone can achieve.

Testosterone Replacement Therapy Protocols
Testosterone Replacement Therapy (TRT) directly addresses states of clinical hypogonadism, where endogenous testosterone production falls below physiological requirements, often due to age-related decline or other medical conditions. TRT involves administering exogenous testosterone, which then binds to androgen receptors in target tissues, promoting anabolic effects, improving bone density, modulating libido, and enhancing overall vitality.
For men, standard protocols frequently involve weekly intramuscular injections of Testosterone Cypionate, a long-acting ester. Concurrently, Gonadorelin, a gonadotropin-releasing hormone (GnRH) agonist, may be administered to stimulate the pituitary’s release of luteinizing hormone (LH) and follicle-stimulating hormone (FSH), thereby maintaining testicular function and preserving fertility.
Anastrozole, an aromatase inhibitor, is often included to mitigate the conversion of exogenous testosterone into estradiol, preventing potential estrogenic side effects. For women, lower doses of Testosterone Cypionate, typically via subcutaneous injection, address symptoms such as low libido, mood fluctuations, and bone density concerns. Progesterone may also be prescribed, particularly for peri- or post-menopausal women, to ensure comprehensive hormonal balance.

Growth Hormone Peptide Therapy
Growth Hormone Peptide Therapy targets the somatotropic axis, stimulating the pituitary gland to produce and release more endogenous growth hormone (GH). This approach differs from direct GH administration, aiming to restore more physiological pulsatile release patterns. Peptides like Sermorelin, a synthetic analog of Growth Hormone-Releasing Hormone (GHRH), directly stimulate the pituitary.
Ipamorelin and CJC-1295 work synergistically, with Ipamorelin acting as a selective ghrelin receptor agonist and CJC-1295 extending the half-life of GHRH, resulting in sustained GH elevation. Tesamorelin specifically targets visceral fat reduction and metabolic optimization, while Hexarelin offers potent GH release for muscle gain and recovery.
Other specialized peptides address specific physiological needs. PT-141 (Bremelanotide) acts on melanocortin receptors in the brain to improve sexual function, distinct from hormonal pathways. Pentadeca Arginate (PDA) is utilized for its regenerative properties, supporting tissue repair, wound healing, and inflammation modulation, impacting cellular recovery and integrity. These peptide therapies represent advanced tools that operate at the level of neuroendocrine signaling and cellular regeneration, offering avenues for physiological optimization beyond the reach of foundational lifestyle adjustments.
- Hormone Replacement Therapy (HRT) for Men ∞
- Testosterone Cypionate ∞ Weekly intramuscular injections (e.g. 200mg/ml) to restore circulating testosterone levels.
- Gonadorelin ∞ Twice weekly subcutaneous injections to support endogenous testosterone production and fertility by stimulating LH and FSH.
- Anastrozole ∞ Twice weekly oral tablets to manage estrogen conversion, reducing potential side effects.
- Hormone Balance Protocols for Women ∞
- Testosterone Cypionate ∞ Low-dose weekly subcutaneous injections (e.g. 10-20 units) for libido, mood, and bone density.
- Progesterone ∞ Tailored dosing based on menopausal status for uterine health and hormonal balance.
- Pellet Therapy ∞ Long-acting subcutaneous testosterone pellets, with Anastrozole considered if appropriate for estrogen management.
- Growth Hormone Peptide Therapies ∞
- Sermorelin ∞ Mimics GHRH to stimulate natural GH release, supporting anti-aging, energy, and sleep.
- Ipamorelin / CJC-1295 ∞ Potent GH secretagogues for muscle growth, fat loss, and enhanced recovery.
- Tesamorelin ∞ Targets visceral fat reduction and metabolic health.

Clinical Interventions and Their Targets
| Intervention Type | Primary Target | Mechanism of Action |
|---|---|---|
| Testosterone Replacement Therapy | Androgen receptor activation, systemic testosterone levels | Exogenous hormone administration to compensate for insufficient endogenous production |
| Gonadorelin | Hypothalamic-Pituitary-Gonadal (HPG) axis | Stimulates pituitary gonadotropin release, preserving testicular function |
| Anastrozole | Aromatase enzyme | Inhibits conversion of androgens to estrogens, managing estrogenic side effects |
| Growth Hormone Peptides | Pituitary somatotrophs, ghrelin receptors | Stimulate pulsatile release of endogenous growth hormone |
| PT-141 | Melanocortin receptors in the central nervous system | Modulates neurochemical pathways related to sexual desire |
| Pentadeca Arginate (PDA) | Cellular repair pathways, inflammatory cascades | Supports tissue regeneration and modulates inflammatory responses |

References
- Fruhbeck, G. & Mendez-Gimenez, L. (2020). Set points, settling points and some alternative models ∞ theoretical options to understand how genes and environments combine to regulate body adiposity. Physiology & Behavior, 227, 113142.
- Gagliano-Jucá, T. & Basaria, S. (2019). Testosterone replacement therapy and cardiovascular risk. Therapeutic Advances in Endocrinology and Metabolism, 10, 204201881988118.
- Guyton, A. C. & Hall, J. E. (2015). Textbook of Medical Physiology (13th ed.). Elsevier.
- Hyman, M. (2020). The UltraMind Solution ∞ Fix Your Broken Brain by Healing Your Body First. Little, Brown and Company.
- Kalsbeek, A. Fliers, E. & Romijn, J. A. (2019). The hypothalamic-pituitary-adrenal axis and sleep. Endotext.
- Kelley, K. W. & Johnson, R. W. (2019). Stress and sleep ∞ Nutritional interventions for adrenal fatigue. Nutrients, 11(10), 2390.
- Leibel, R. L. Rosenbaum, M. & Hirsch, J. (1995). Changes in energy expenditure resulting from altered body weight. New England Journal of Medicine, 332(10), 621-628.
- Loche, S. Farello, G. & Cappa, M. (2018). Growth hormone-releasing peptides ∞ clinical and basic aspects. Journal of Pediatric Endocrinology and Metabolism, 31(1), 1-10.
- McEwen, B. S. (2007). Physiology and neurobiology of stress and adaptation ∞ central role of the brain. Physiological Reviews, 87(3), 873-904.
- Papadakis, M. A. & McPhee, S. J. (2020). Current Medical Diagnosis & Treatment 2020 (59th ed.). McGraw-Hill Education.
- Rebar, R. W. & Yen, S. S. C. (1973). The effect of an LH-RH analogue on the secretion of LH and FSH in women. Journal of Clinical Endocrinology & Metabolism, 37(6), 917-920.
- Speroff, L. & Fritz, M. A. (2019). Clinical Gynecologic Endocrinology and Infertility (9th ed.). Lippincott Williams & Wilkins.
- Tsigos, C. & Chrousos, G. P. (2002). Hypothalamic-pituitary-adrenal axis, neuroendocrine factors and stress. Journal of Psychosomatic Research, 53(4), 865-871.
- Veldhuis, J. D. & Dufau, M. L. (2018). Neuroendocrine mechanisms in the pulsatile secretion of growth hormone. Growth Hormone & IGF Research, 40, 1-11.
- Veldhuis, J. D. & Johnson, M. L. (2019). Modeling of endocrine systems. Methods in Enzymology, 539, 3-26.

Reflection
Understanding your body’s hormonal landscape, and the intrinsic limits within which lifestyle interventions operate, marks a significant step toward informed self-advocacy. This knowledge invites you to move beyond generalized advice, encouraging a deeper introspection into your unique biological systems.
Consider this information as a guide, prompting you to observe your body’s responses with heightened awareness and to recognize when the subtle language of symptoms signals a need for more precise, clinically informed support. Your journey toward optimal vitality is deeply personal, demanding a collaborative approach with your body’s inherent wisdom and, at times, with advanced scientific understanding.



