Fundamentals
You may feel it as a subtle shift in your stamina, a change in how your body responds to exertion, or perhaps you’ve noted clinical markers like blood pressure beginning to trend in a new direction. These experiences are valid and often point toward deeper physiological processes.
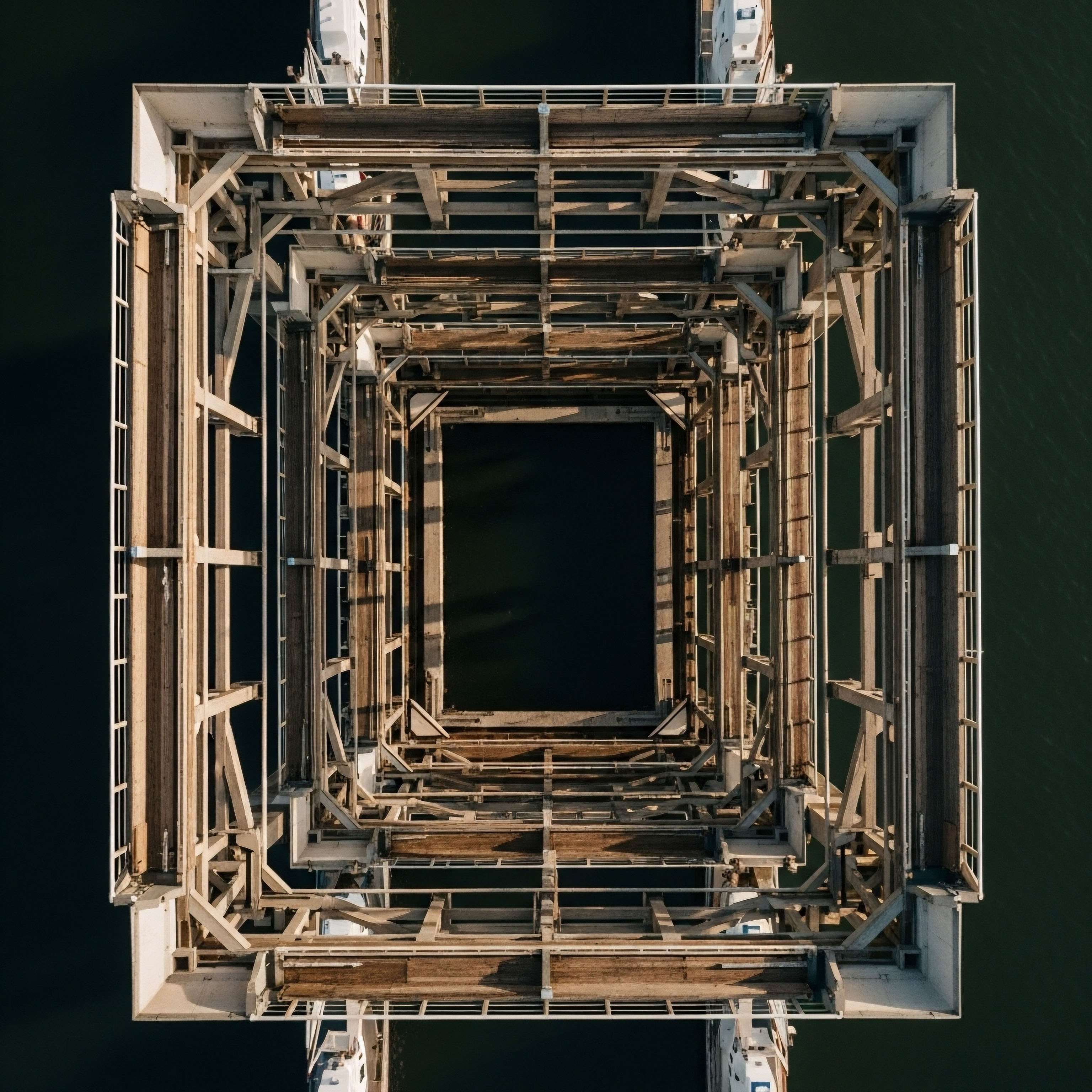
One of the most central of these is vascular remodeling, the body’s continuous process of altering the structure of your blood vessels. This is your circulatory system’s innate method for adapting to long-term changes in pressure, flow, and the complex hormonal signals that govern your internal environment. It is a biological response mechanism designed to maintain stability. The architecture of your arteries and veins is dynamic, constantly being rebuilt in response to the demands placed upon it.
Think of your vascular system as an intelligent network of roadways. When traffic patterns change consistently ∞ perhaps due to increased demand in one area ∞ the system must adapt by widening lanes or building new routes. Similarly, your blood vessels undergo structural changes to manage fluctuations in blood flow and pressure.
This remodeling involves the cells that make up the vessel walls, particularly the vascular smooth muscle cells Micronized progesterone interacts with nuclear, membrane, and mitochondrial receptors in vascular cells to regulate gene expression and rapid signaling. (VSMCs) and the endothelial cells that form the inner lining. These cells respond to both mechanical forces, like the shear stress of blood flow, and a vast array of biochemical messengers, including the hormones that orchestrate so much of your body’s function.
The process can be adaptive, helping your body cope, or it can become maladaptive, contributing to the very symptoms you may be experiencing.
Vascular remodeling is the active, structural adaptation of blood vessels in response to sustained changes in mechanical and biochemical signals.
The primary drivers of this remodeling process are multifaceted, involving an intricate interplay between physical forces and your body’s internal chemistry. Hypertension, or elevated blood pressure, is a powerful mechanical stimulus that forces the vessel wall to thicken to withstand the increased force. This is a form of hypertrophic remodeling, where the vessel wall gains mass.
Conversely, other stimuli might cause different adaptations. The health of the endothelium, the single layer of cells lining your blood vessels, is paramount. A healthy endothelium produces nitric oxide (NO), a molecule that signals smooth muscle cells Sex hormones directly instruct heart muscle cells on energy production, structural integrity, and contractile force via specific receptors. to relax, promoting healthy blood flow and preventing excessive cellular growth. When endothelial function Meaning ∞ Endothelial function refers to the physiological performance of the endothelium, the thin cellular layer lining blood vessels. is compromised, this delicate balance is disturbed, setting the stage for structural changes that can affect your entire system.

The Cellular Architects of Your Arteries
At the heart of vascular remodeling Meaning ∞ Vascular remodeling describes the structural and functional changes occurring in blood vessel walls. are the vascular smooth muscle Testosterone modulates vascular reactivity by directly influencing blood vessel smooth muscle and supporting nitric oxide production, vital for cardiovascular health. cells. In a healthy vessel, these cells are in a “contractile” state, primarily responsible for managing vessel tone ∞ the degree of constriction or dilation. In response to certain signals, such as injury, inflammation, or specific hormonal cues, these VSMCs can undergo a profound transformation.
They shift to a “synthetic” phenotype, where their primary job changes from contraction to proliferation and migration. These transformed cells move from the middle layer of the artery (the media) into the inner layer (the intima), contributing to wall thickening and the formation of plaques, a hallmark of atherosclerosis. This cellular behavior is a core mechanism in nearly all forms of vascular remodeling.
The extracellular matrix Meaning ∞ The Extracellular Matrix, often abbreviated as ECM, represents the non-cellular component present within all tissues and organs, providing essential physical scaffolding for cellular constituents and initiating crucial biochemical and biomechanical signals. (ECM), the protein scaffold that gives the vessel wall its structure and elasticity, is also a key player. It is composed of proteins like collagen and elastin. During remodeling, the balance between the production and degradation of these proteins changes dramatically.
An increase in collagen deposition leads to stiffening of the arteries, a condition that is a major contributor to cardiovascular disease and mortality. The breakdown of elastin fibers, which provide flexibility, further compromises the vessel’s ability to expand and contract with each heartbeat. This loss of elasticity means the heart must work harder to pump blood through a more rigid system, creating a feedback loop that can perpetuate the remodeling process.


Intermediate
Understanding that vascular remodeling occurs is the first step. The next is to appreciate how your endocrine system ∞ the intricate web of hormones that acts as your body’s master regulator ∞ directly orchestrates these structural changes. Your hormonal status is a powerful determinant of your vascular health.
Sex hormones, in particular, exert profound and direct effects on the cells of the vessel wall, influencing everything from smooth muscle cell proliferation to endothelial function. These are not secondary effects; they are direct, receptor-mediated actions that can either protect your vascular system or accelerate maladaptive remodeling, depending on the context of your overall health and hormonal balance.
Hormonal optimization protocols are designed with this deep connection in mind. When we address hormonal deficiencies, we are concurrently influencing the biological environment of the vascular wall. For men, testosterone plays a complex role. It can modulate vascular tone and has been shown to influence the migration of vascular smooth muscle cells.
Low testosterone levels are often associated with endothelial dysfunction, a state where the vessel lining fails to produce adequate nitric oxide. Restoring testosterone to a healthy physiological range can improve this crucial function. The hormone interacts with androgen receptors present on both endothelial and smooth muscle cells, triggering signaling cascades that affect cell growth and function.

How Do Hormones Directly Influence Vascular Structure?
The mechanisms by which hormones direct vascular remodeling are specific and increasingly well-understood. They operate through both genomic and non-genomic pathways. Genomic pathways involve the hormone binding to a receptor inside the cell, which then travels to the nucleus to alter gene expression ∞ a slower, more sustained effect. Non-genomic pathways are rapid, occurring at the cell membrane and triggering immediate changes in intracellular signaling.
Estrogen, for instance, has well-documented vasoprotective effects, primarily through its interaction with estrogen receptors (ERα and ERβ) found abundantly in vascular tissue. Activation of these receptors enhances the production of nitric oxide, inhibits VSMC proliferation and migration, and reduces inflammation within the vessel wall.
Progesterone also has a role, often working in concert with estrogen to maintain vascular health. The decline of these hormones during perimenopause and menopause removes this protective shield, contributing to the increased cardiovascular risk seen in postmenopausal women. For women receiving low-dose testosterone therapy, the goal is to restore a healthy androgen-to-estrogen balance, which can improve libido and energy while supporting vascular function, often in conjunction with progesterone to ensure endometrial safety and overall hormonal synergy.
Hormones like testosterone and estrogen directly bind to receptors on vascular cells, modulating gene expression and signaling pathways that control vessel growth, repair, and tone.
The following table outlines the primary vascular effects of key sex hormones, illustrating their direct influence on the cellular components of the vessel wall.
| Hormone | Effect on Endothelial Cells | Effect on Vascular Smooth Muscle Cells (VSMCs) | Overall Impact on Remodeling |
|---|---|---|---|
| Testosterone |
Modulates nitric oxide (NO) production; activation of androgen receptors can increase NO synthase activity. |
Influences VSMC migration and proliferation, potentially via NADPH oxidase-derived reactive oxygen species. |
Complex role; protective at physiological levels by improving endothelial function, but can contribute to maladaptive remodeling in certain contexts. |
| Estrogen (Estradiol) |
Strongly promotes NO production, leading to vasodilation; reduces expression of adhesion molecules. |
Inhibits VSMC proliferation and migration, a key protective mechanism against intimal thickening. |
Primarily protective; helps maintain a healthy vascular structure and prevents maladaptive changes associated with injury or inflammation. |

The Role of Peptides and Growth Factors
Beyond the primary sex hormones, other signaling molecules are critical to vascular health Meaning ∞ Vascular health signifies the optimal physiological state and structural integrity of the circulatory network, including arteries, veins, and capillaries, ensuring efficient blood flow. and are often a focus of advanced wellness protocols. Growth hormone (GH) and the peptides that stimulate its release, such as Sermorelin and Ipamorelin, also have significant vascular effects.
GH receptors are present on endothelial cells, and GH can directly stimulate the production of nitric oxide. It also promotes the mobilization of endothelial progenitor cells, which are crucial for repairing damage to the vessel lining. This makes GH peptide therapy a valuable tool not just for body composition and recovery, but for maintaining the integrity of the vascular system itself.
Other specialized peptides can also play a role in tissue repair that extends to the vascular system. For instance, BPC-157 is known to modulate the activity of vascular endothelial growth factor (VEGF), a key signaling protein that drives the formation of new blood vessels (angiogenesis).
By enhancing growth factor signaling and improving local circulation through nitric oxide Meaning ∞ Nitric Oxide, often abbreviated as NO, is a short-lived gaseous signaling molecule produced naturally within the human body. pathways, such peptides can support the healing of damaged tissues, including the vessel walls themselves. This highlights a systems-based approach where restoring foundational signaling pathways can have broad, beneficial effects on your body’s ability to maintain and repair its critical infrastructure.


Academic
A sophisticated analysis of vascular remodeling moves beyond cataloging stimuli and responses to examine the central role of cellular phenotype switching, particularly within the vascular smooth muscle cell Meaning ∞ Vascular Smooth Muscle Cells are specialized contractile cells forming the muscular layer within the walls of arteries, veins, and lymphatic vessels, primarily responsible for regulating vessel diameter and, consequently, blood flow and systemic blood pressure. (VSMC) population. This process is the nexus where mechanical forces, hormonal signals, and inflammatory mediators converge to dictate vessel architecture.
The transition of a VSMC from a quiescent, contractile state to a proliferative, synthetic phenotype is the defining event in the pathogenesis of intimal hyperplasia, the anatomical basis for both atherosclerosis Meaning ∞ Atherosclerosis is a chronic inflammatory condition characterized by the progressive accumulation of lipid and fibrous material within the arterial walls, forming plaques that stiffen and narrow blood vessels. and restenosis following vascular intervention. This phenotypic plasticity is not a random occurrence; it is a highly regulated, multi-step process governed by specific transcription factors, microRNAs, and complex intracellular signaling cascades.
The hormonal regulation Meaning ∞ Hormonal regulation refers to the precise physiological processes controlling hormone synthesis, release, action, and degradation. of this phenotypic switch is a critical area of investigation. Androgens and estrogens exert direct, often opposing, effects on the molecular machinery controlling VSMC behavior. Testosterone, for example, has been shown in vitro to stimulate VSMC migration through pathways involving reactive oxygen species (ROS) generated by NADPH oxidase.
This process is dependent on both genomic and non-genomic actions, activating kinases like c-Src that are integral to cell motility. This suggests that in certain pro-inflammatory or high-stress environments, androgen signaling could potentially facilitate the migration of VSMCs into the intima, contributing to lesion formation. This provides a molecular rationale for why hormonal balance, rather than just the absolute level of a single hormone, is paramount for vascular health.

What Is the Molecular Crosstalk between Hormones and Vsmc Phenotype?
The molecular dialogue between hormonal signals and VSMC function is intricate. Estrogen, acting through ERα, is a powerful inhibitor of VSMC proliferation. It achieves this by interfering with key cell cycle progression pathways. For instance, estradiol can suppress the mitogenic effects of growth factors Meaning ∞ Growth factors are a diverse group of signaling proteins or peptides that regulate cellular processes within the body. like platelet-derived growth factor (PDGF) by inhibiting the phosphorylation of mitogen-activated protein kinases (MAPKs) such as ERK1/2 and p38.
This effectively blocks the signal for the cell to divide. Furthermore, estrogen has been shown to downregulate the expression of Sirtuin 1 (SIRT1) in VSMCs, a protein involved in cell survival, which leads to increased apoptosis (programmed cell death) of these cells and reduced proliferation and migration. This provides a powerful braking mechanism on the development of intimal thickening.
This contrasts with some of the signaling initiated by other factors. Angiotensin II, a potent vasoconstrictor, is a major driver of VSMC proliferation and hypertrophy and is a key molecule in hypertensive remodeling. The interplay between these systems is crucial. For example, healthy estrogen levels can blunt the proliferative response to angiotensin II, providing another layer of vascular protection.
The loss of this estrogenic check-and-balance system after menopause can unmask the potent remodeling effects of the renin-angiotensin system, contributing to accelerated vascular aging.
The phenotypic state of the vascular smooth muscle cell is the ultimate determinant of structural remodeling, a state directly governed by the complex interplay of hormonal and mechanical signaling pathways.
The following table details some of the key molecular players involved in the hormonal regulation of VSMC function, providing insight into the specific pathways targeted by therapeutic interventions.
| Signaling Pathway | Regulator | Effect on VSMC Phenotype | Therapeutic Relevance |
|---|---|---|---|
| MAPK (ERK1/2, p38) |
Estrogen (via ERα) |
Inhibits phosphorylation, thus blocking proliferation and migration signals from growth factors like PDGF. |
Explains the protective effect of estrogen against neointima formation. Loss of this inhibition contributes to postmenopausal vascular risk. |
| NADPH Oxidase / ROS |
Testosterone |
Stimulates ROS production, which can promote VSMC migration through redox-sensitive pathways. |
Highlights the importance of managing oxidative stress alongside hormone optimization. Anastrozole, used in TRT, mitigates estrogenic side effects but managing the androgen-driven redox state is also key. |
| SIRT1 Downregulation |
Estrogen |
Decreases SIRT1 expression, leading to increased apoptosis and reduced proliferation of VSMCs. |
Demonstrates a mechanism by which estrogen helps clear excess smooth muscle cells, preventing pathological accumulation in the vessel wall. |
| Nitric Oxide Synthase (eNOS) |
Estrogen, Testosterone, GH |
Increases NO production in the endothelium, which in turn inhibits VSMC growth and promotes relaxation. |
A common pathway for multiple hormones that supports vascular health. Protocols that enhance endothelial function are fundamentally supporting this anti-remodeling mechanism. |

Systemic Inflammation and the Adventitial Contribution
The academic view of vascular remodeling now extends beyond the intima and media to recognize the critical role of the adventitia, the outermost layer of the blood vessel. This layer is a reservoir of inflammatory cells, fibroblasts, and progenitor cells. In response to injury or chronic stress like hypertension, the adventitia becomes a hotbed of inflammation.
Macrophages and T-lymphocytes are recruited to the area, releasing a flood of cytokines and growth factors that permeate the vessel wall, profoundly influencing the behavior of VSMCs in the media. This “outside-in” signaling is a major driver of maladaptive remodeling.
Hormones are potent modulators of this inflammatory response. Estrogen generally exerts anti-inflammatory effects, reducing the expression of cytokines and adhesion molecules that attract immune cells. Growth hormone Meaning ∞ Growth hormone, or somatotropin, is a peptide hormone synthesized by the anterior pituitary gland, essential for stimulating cellular reproduction, regeneration, and somatic growth. also influences the immune system, and its impact on vascular inflammation is an area of active research, with evidence suggesting it can reduce markers like C-reactive protein in deficient individuals.
Therefore, a comprehensive understanding of vascular remodeling must be viewed through a systems-biology lens, integrating endocrinology with immunology and cellular mechanics. Therapeutic protocols that only target one aspect of this complex system may be less effective than those that address the foundational hormonal and inflammatory environment of the entire vessel.
- Vascular Smooth Muscle Cells (VSMCs) ∞ These cells are central to remodeling, capable of switching from a contractile to a synthetic, proliferative state.
- Endothelial Cells ∞ This inner lining of the vessel is a critical sensor and transducer of hemodynamic and biochemical signals, primarily through nitric oxide production.
- Extracellular Matrix (ECM) ∞ The balance of collagen and elastin deposition and degradation determines the stiffness and compliance of the vessel wall.
- Inflammatory Cells ∞ Macrophages and lymphocytes, particularly in the adventitia, release cytokines that drive VSMC proliferation and migration.

References
- Humphrey, J. D. & Dufresne, E. R. (2021). Mechanisms of Vascular Remodeling in Hypertension. American Journal of Hypertension, 34(5), 459 ∞ 467.
- van Varik, B. J. Rennenberg, R. J. Reutelingsperger, C. P. Kroon, A. A. de Leeuw, P. W. & Schurgers, L. J. (2012). Mechanisms of arterial remodeling. Frontiers in Bioscience, 17(1), 1492-1507.
- Spyridopoulos, I. Llevadot, J. & Losordo, D. W. (2001). Estrogen Regulation of Endothelial and Smooth Muscle Cell Migration and Proliferation. Arteriosclerosis, Thrombosis, and Vascular Biology, 21(11), 1747 ∞ 1752.
- Yanes, L. L. & Reckelhoff, J. F. (2011). VASCULAR ACTIONS OF ESTROGENS ∞ FUNCTIONAL IMPLICATIONS. Physiology, 26(4), 232 ∞ 244.
- Tosta, C. E. & de Moura, P. J. (2013). Testosterone and the Cardiovascular System ∞ A Comprehensive Review of the Basic Science Literature. Journal of the American Heart Association, 2(4), e000271.
- Liao, W. Wang, J. Xu, D. & Fang, C. (2018). Estrogen modulates vascular smooth muscle cell function through downregulation of SIRT1. Experimental and Therapeutic Medicine, 16(5), 4447 ∞ 4453.
- Carnevale, R. & Cammisotto, V. (2016). Growth Hormone (GH) and Cardiovascular System. Current Pharmaceutical Design, 22(34), 5276-5283.
- Goglia, F. Silvestri, E. & Lanni, A. (2010). Testosterone and Vascular Function in Aging. Frontiers in Physiology, 1, 19.
- Khalil, R. A. (2013). Estrogen, Vascular Estrogen Receptor and Hormone Therapy in Postmenopausal Vascular Disease. Biochemical Pharmacology, 2(3), 1000121.
- George, A. & Raper, A. (2009). Estrogen and Mechanisms of Vascular Protection. Arteriosclerosis, Thrombosis, and Vascular Biology, 29(3), 286-292.

Reflection
The information presented here provides a map of the complex biological territory known as vascular remodeling. It connects the symptoms you may feel to the cellular and molecular events occurring within your arteries. This knowledge is the foundational step.
Seeing how your internal hormonal symphony conducts the behavior of your vascular cells reframes the conversation from one of passive symptoms to one of active systems. Your body is a network of interconnected signals, and understanding the language of these signals is the beginning of a more proactive and informed approach to your own health.
The path forward involves considering how your unique biochemistry aligns with these fundamental processes and what personalized strategies can best support the lifelong integrity of your vascular system.