

Fundamentals
You feel it before you can name it. A subtle shift in energy, a change in the way your body responds to exercise, or a fog that clouds your thoughts. These experiences are not abstract; they are the direct result of intricate biochemical conversations happening within your body. When we discuss personalized hormone replacement Personalized hormone protocols precisely calibrate your body’s unique endocrine needs, restoring balance beyond conventional, standardized approaches. therapy, we are talking about recalibrating this internal communication network.
The primary concern for anyone considering this path is, understandably, its long-term safety. This is a conversation about your future self, about ensuring that the vitality you reclaim today is sustained for a lifetime.
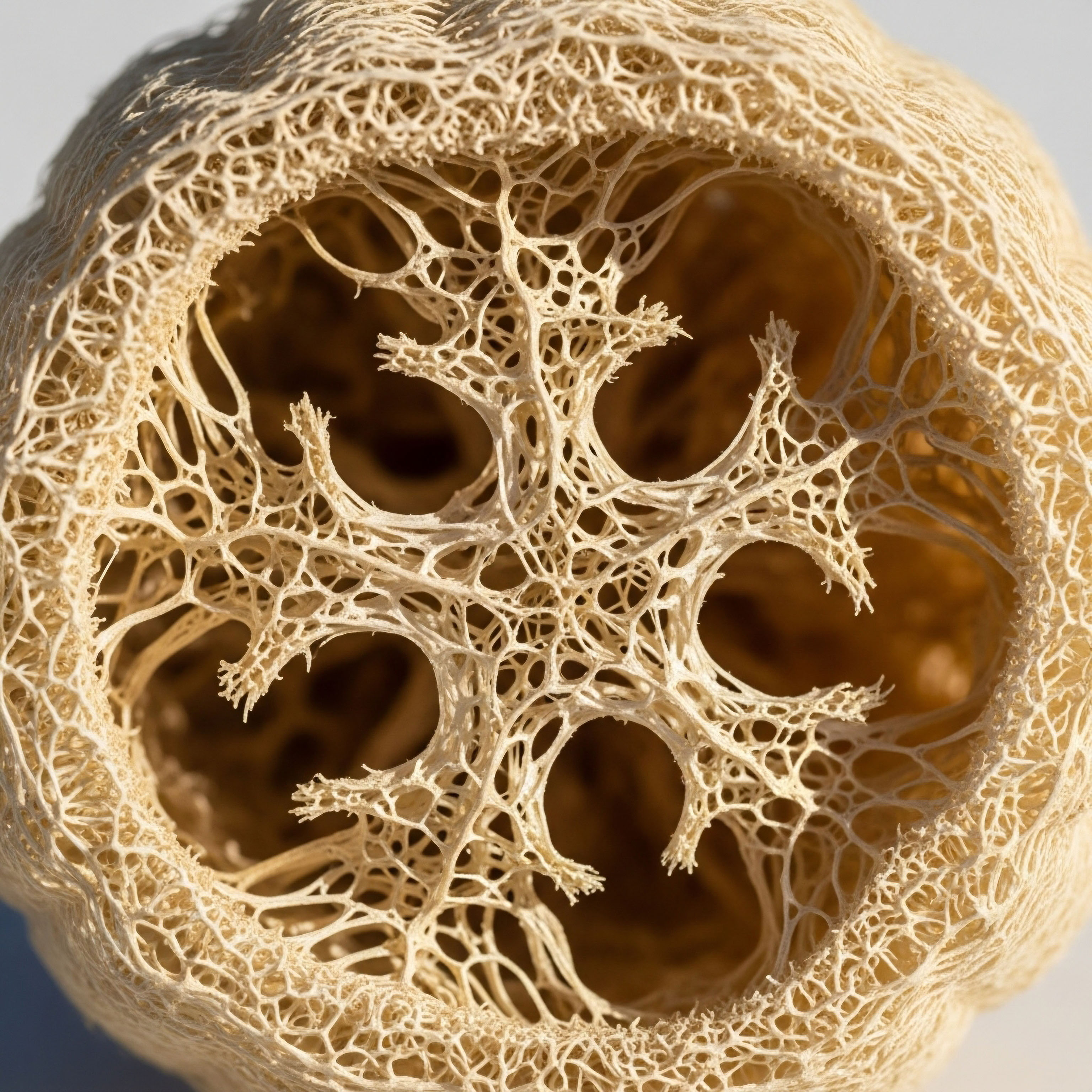
The human body is a system of systems, a complex interplay of feedback loops where hormones act as messengers. The endocrine system, which governs these hormones, is designed for resilience and adaptation. However, with age and environmental stressors, its efficiency can decline.
This can manifest as low testosterone in men, leading to fatigue and diminished drive, or the complex hormonal fluctuations of perimenopause and menopause Meaning ∞ Menopause signifies the permanent cessation of ovarian function, clinically defined by 12 consecutive months of amenorrhea. in women, which can disrupt everything from sleep to mood. The goal of personalized hormonal support is to gently guide these systems back to a state of optimal function, using the lowest effective doses of bioidentical hormones—molecules that are structurally identical to those your body naturally produces.
A foundational principle of personalized hormone therapy is to restore physiological balance, not to push the body beyond its natural limits.
Understanding the safety of these protocols begins with understanding the individual. A “one-size-fits-all” approach is antithetical to true wellness. Your unique biology, genetics, and lifestyle are the starting point for any therapeutic consideration. Before any intervention, a comprehensive diagnostic process, including detailed blood work, is essential.
This provides a baseline, a map of your internal hormonal landscape. This data-driven approach allows for precise, individualized protocols that are continuously monitored and adjusted over time. This is a partnership between you and your clinician, a shared journey toward sustainable health.

The Role of Bioidentical Hormones
The term “bioidentical” is significant. Unlike synthetic hormones, which have a different molecular structure, bioidentical hormones Meaning ∞ Bioidentical hormones are substances structurally identical to the hormones naturally produced by the human body. are recognized and metabolized by the body in the same way as its own. This is a key factor in their safety profile.
For men, this often involves testosterone cypionate, a form of testosterone that is slowly released into the bloodstream, mimicking the body’s natural rhythm. For women, it may involve a combination of estradiol, progesterone, and sometimes a small amount of testosterone, all tailored to their specific needs and phase of life.

Key Hormones and Their Function
- Testosterone ∞ In both men and women, testosterone is vital for maintaining muscle mass, bone density, cognitive function, and libido.
- Progesterone ∞ In women, progesterone plays a crucial role in regulating the menstrual cycle and pregnancy. In menopausal women, it is used to protect the uterine lining and has been shown to improve sleep and mood.
- Estradiol ∞ The primary female sex hormone, estradiol is essential for bone health, cardiovascular function, and cognitive well-being.
The safety of these therapies is further enhanced by the use of ancillary medications when necessary. For example, men on testosterone replacement therapy Meaning ∞ Testosterone Replacement Therapy (TRT) is a medical treatment for individuals with clinical hypogonadism. may also be prescribed anastrozole to manage estrogen levels or gonadorelin to maintain natural testicular function. These additions are not an afterthought; they are an integral part of a holistic protocol designed to maintain the delicate balance of the entire endocrine system.


Intermediate
Advancing beyond the foundational concepts of hormonal balance, an intermediate understanding requires a closer look at the specific clinical protocols and the long-term data that informs them. The safety of personalized hormone replacement therapy Personalized hormone protocols precisely calibrate your body’s unique endocrine needs, restoring balance beyond conventional, standardized approaches. is not a matter of opinion; it is a conclusion drawn from decades of clinical research and a deep understanding of endocrinology. Here, we will examine the evidence surrounding the most common protocols, moving from the theoretical to the practical application of this science.
For men, the primary concern with testosterone replacement Meaning ∞ Testosterone Replacement refers to a clinical intervention involving the controlled administration of exogenous testosterone to individuals with clinically diagnosed testosterone deficiency, aiming to restore physiological concentrations and alleviate associated symptoms. therapy (TRT) has historically been its potential impact on cardiovascular health and prostate cancer risk. Recent, large-scale studies have provided significant clarity on these issues. The TRAVERSE study, a landmark clinical trial, found that TRT in men with hypogonadism and a high risk of cardiovascular disease was not associated with an increased incidence of major adverse cardiac events. This finding has been reassuring for both clinicians and patients, suggesting that when properly managed, TRT does not appear to increase the risk of heart attack or stroke.
Ongoing monitoring and dose adjustments are critical components of a safe and effective long-term hormone optimization strategy.
Similarly, the concern that TRT could increase the risk of prostate cancer Meaning ∞ Prostate cancer represents a malignant cellular proliferation originating within the glandular tissue of the prostate gland. has been addressed by numerous studies. A large review of medical records in Sweden found that long-term use of TRT did not increase the overall risk of prostate cancer. In fact, the study suggested a potential reduction in the risk of aggressive prostate cancer in men who had been on therapy for more than a year. This data suggests that the historical fear of TRT and prostate cancer may have been overstated, and that with appropriate screening and monitoring, TRT can be a safe option for hypogonadal men.

Protocols for Men and Women
The specific protocols used in personalized hormone therapy are designed to mimic the body’s natural rhythms and maintain hormonal equilibrium. This is achieved through careful selection of hormones, delivery methods, and ancillary medications.
Male Hormone Optimization
A standard protocol for men with low testosterone often involves weekly intramuscular or subcutaneous injections of testosterone cypionate. This is frequently combined with other medications to create a comprehensive support system for the endocrine system.
- Testosterone Cypionate ∞ A long-acting ester of testosterone that provides a steady release of the hormone.
- Gonadorelin ∞ A peptide that stimulates the pituitary gland to produce luteinizing hormone (LH) and follicle-stimulating hormone (FSH), which in turn helps to maintain natural testosterone production and testicular size.
- Anastrozole ∞ An aromatase inhibitor that blocks the conversion of testosterone to estrogen, helping to prevent side effects such as gynecomastia and water retention.

Female Hormone Optimization
For women, protocols are highly individualized based on their menopausal status and specific symptoms. The goal is to restore hormonal balance and alleviate the symptoms of perimenopause and menopause.
| Hormone | Typical Application | Primary Benefit |
|---|---|---|
| Testosterone Cypionate | Low-dose weekly subcutaneous injections | Improved libido, energy, and cognitive function |
| Progesterone | Oral capsules or topical creams | Protects uterine lining, improves sleep, and balances mood |
| Estradiol | Transdermal patches or gels | Alleviates hot flashes, night sweats, and vaginal dryness |
For postmenopausal women, the combination of estrogen and progesterone is crucial for those who still have a uterus, as unopposed estrogen can increase the risk of endometrial cancer. The use of bioidentical progesterone, such as oral micronized progesterone, has been shown to be a safe and effective way to provide this protection while also offering additional benefits like improved sleep.
Academic
An academic exploration of the long-term safety Meaning ∞ Long-term safety signifies the sustained absence of significant adverse effects or unintended consequences from a medical intervention, therapeutic regimen, or substance exposure over an extended duration, typically months or years. of personalized hormone replacement therapy Peptide therapy may reduce HRT dosages by optimizing the body’s own hormonal signaling and enhancing cellular sensitivity. requires a granular analysis of the available clinical data and a nuanced understanding of the underlying physiological mechanisms. This deep dive moves beyond general reassurances to examine the specific risks and benefits of these therapies, as documented in peer-reviewed literature. The conversation here is one of statistical significance, risk ratios, and the complex interplay of hormonal pathways.
The TRAVERSE trial, published in the New England Journal of Medicine, represents a pivotal moment in our understanding of testosterone therapy’s cardiovascular safety. This large, randomized, placebo-controlled study demonstrated noninferiority for major adverse cardiac events Initiating TRT post-cardiac event is possible with careful timing, stabilization, and rigorous medical oversight to balance benefits and risks. in men with hypogonadism and cardiovascular risk factors. However, a closer look at the data reveals a more complex picture.
While the primary composite endpoint was not met, there was a higher incidence of atrial fibrillation, acute kidney injury, and pulmonary embolism in the testosterone group. This underscores the importance of careful patient selection and monitoring, particularly for men with pre-existing renal or cardiac conditions.
The long-term safety of any therapeutic intervention is best understood through a rigorous, evidence-based assessment of its effects on multiple physiological systems.
Regarding prostate safety, the data has been consistently reassuring. Multiple studies, including a large population-based study from Sweden and a meta-analysis of randomized controlled trials, have failed to show an association between TRT and an increased risk of high-grade prostate cancer. Some research even suggests a potential protective effect against aggressive disease with long-term use. The prevailing hypothesis is that there is a saturation point for testosterone’s effect on prostate tissue; once this is reached, further increases in testosterone levels do not appear to promote cancer growth.

Growth Hormone Peptides and Progesterone Safety
The use of growth hormone Meaning ∞ Growth hormone, or somatotropin, is a peptide hormone synthesized by the anterior pituitary gland, essential for stimulating cellular reproduction, regeneration, and somatic growth. secretagogues, such as Sermorelin and Ipamorelin, represents a more recent development in personalized wellness. These peptides stimulate the body’s own production of growth hormone, offering a more physiological approach than direct injection of recombinant human growth hormone (rhGH). While long-term safety data on these specific peptides is still emerging, they are generally considered to have a favorable safety profile due to their mechanism of action, which preserves the natural pulsatile release of GH and is subject to the body’s own negative feedback loops. Concerns about the long-term effects of elevated GH and IGF-1 levels, such as potential impacts on insulin sensitivity and cell proliferation, remain a subject of ongoing research.

What Are the Long-Term Safety Considerations for Progesterone Therapy in China?
In the context of China, where there is a growing interest in personalized wellness, the long-term safety of progesterone therapy Meaning ∞ Progesterone therapy involves the exogenous administration of the steroid hormone progesterone or synthetic progestins. for postmenopausal women is a particularly relevant topic. The cultural and genetic factors specific to the Chinese population may influence the risk-benefit profile of this therapy. While large-scale, long-term studies specifically in Chinese women are needed, the existing body of international research provides a strong foundation for clinical practice. The E3N cohort study in France, for example, found that the use of bioidentical progesterone in combination with transdermal estrogen was not associated with an increased risk of breast cancer.
This is in contrast to synthetic progestins, which have been linked to an increased risk. This distinction is critical for ensuring the long-term safety of hormone therapy for women.
| Therapy | Primary Safety Concern | Current Evidence |
|---|---|---|
| Testosterone Replacement Therapy (Men) | Cardiovascular Events & Prostate Cancer | No increased risk of MACE or high-grade prostate cancer in major studies. |
| Progesterone Therapy (Women) | Breast Cancer Risk | Bioidentical progesterone not associated with increased risk in some large studies. |
| Growth Hormone Peptides | Long-term effects of elevated IGF-1 | Generally well-tolerated, but long-term data is still being gathered. |
The long-term safety of personalized hormone replacement Meaning ∞ Hormone Replacement involves the exogenous administration of specific hormones to individuals whose endogenous production is insufficient or absent, aiming to restore physiological levels and alleviate symptoms associated with hormonal deficiency. therapy is not a static concept. It is an evolving field of medicine that is continually being refined by new research and clinical experience. The available evidence strongly suggests that when these therapies are administered by experienced clinicians, using bioidentical hormones and evidence-based protocols, they represent a safe and effective way to improve quality of life and promote long-term wellness.
References
- Lincoff, A. M. Bhasin, S. Flevaris, P. et al. “Cardiovascular Safety of Testosterone-Replacement Therapy.” New England Journal of Medicine, 2023.
- “Long-term Exposure to Testosterone Therapy and the Risk of High Grade Prostate Cancer.” The Journal of Urology, vol. 194, no. 5, 2015, pp. 1212-1217.
- Fournier, A. Berrino, F. & Clavel-Chapelon, F. “Unequal risks for breast cancer associated with different hormone replacement therapies ∞ results from the E3N cohort study.” Breast Cancer Research and Treatment, vol. 107, no. 1, 2008, pp. 103-111.
- Carel, J. C. Ecosse, E. Landier, F. et al. “Long-term mortality after recombinant growth hormone treatment for isolated growth hormone deficiency or childhood short stature ∞ preliminary report of the French SAGhE study.” The Journal of Clinical Endocrinology & Metabolism, vol. 97, no. 2, 2012, pp. 416-425.
- Loeb, S. et al. “Long-term use of testosterone replacement therapy does not appear to increase the risk of prostate cancer.” Presented at the American Urological Association Annual Meeting, 2016.
- Jerilynn C. Prior. “Progesterone Therapy for Menopause.” Centre for Menstrual Cycle and Ovulation Research, 2018.
- Teichmann, J. “Progesterone in Peri- and Postmenopause ∞ A Review.” Gynecological Endocrinology, vol. 34, no. sup1, 2018, pp. 5-9.
- Sigalos, J. T. & Zito, P. M. “Ipamorelin.” StatPearls, StatPearls Publishing, 2023.
- “Testosterone Replacement Therapy for Assessment of Long-term Vascular Events and Efficacy Response in Hypogonadal Men (TRAVERSE).” Cleveland Clinic, 2023.
- “Hormone Replacement Therapy (HRT) for Menopause.” Cleveland Clinic, 2022.
Reflection
The information presented here is a map, a detailed guide to the scientific landscape of hormonal health. It is designed to equip you with the knowledge to ask informed questions and to understand the intricate biological processes that shape your daily experience. Your personal health narrative, however, is uniquely your own. The sensations of renewed energy, the clarity of thought, the return of a sense of well-being—these are the destinations that the map can help you reach.
The journey itself is a collaborative one, a partnership between your lived experience and the clinical expertise of a trusted guide. This knowledge is the first step toward reclaiming your biological sovereignty, empowering you to make choices that will resonate through every aspect of your life for years to come.








