Fundamentals
You feel it before you can name it. A subtle shift in energy, a fog that settles over your thoughts, a change in the way your body responds to food, to exercise, to stress. This lived experience is the first and most important piece of data.
It is the signal that your internal communication network, the exquisitely sensitive endocrine system, is undergoing a profound change. When we consider hormonal therapy, we are considering a way to restore a conversation that has been disrupted. The long-term success of this intervention, however, is shaped by the environment in which these new messages are received.
Your daily choices regarding nutrition, movement, sleep, and stress are the environmental factors that determine whether this restored conversation is clear and effective or filled with static.
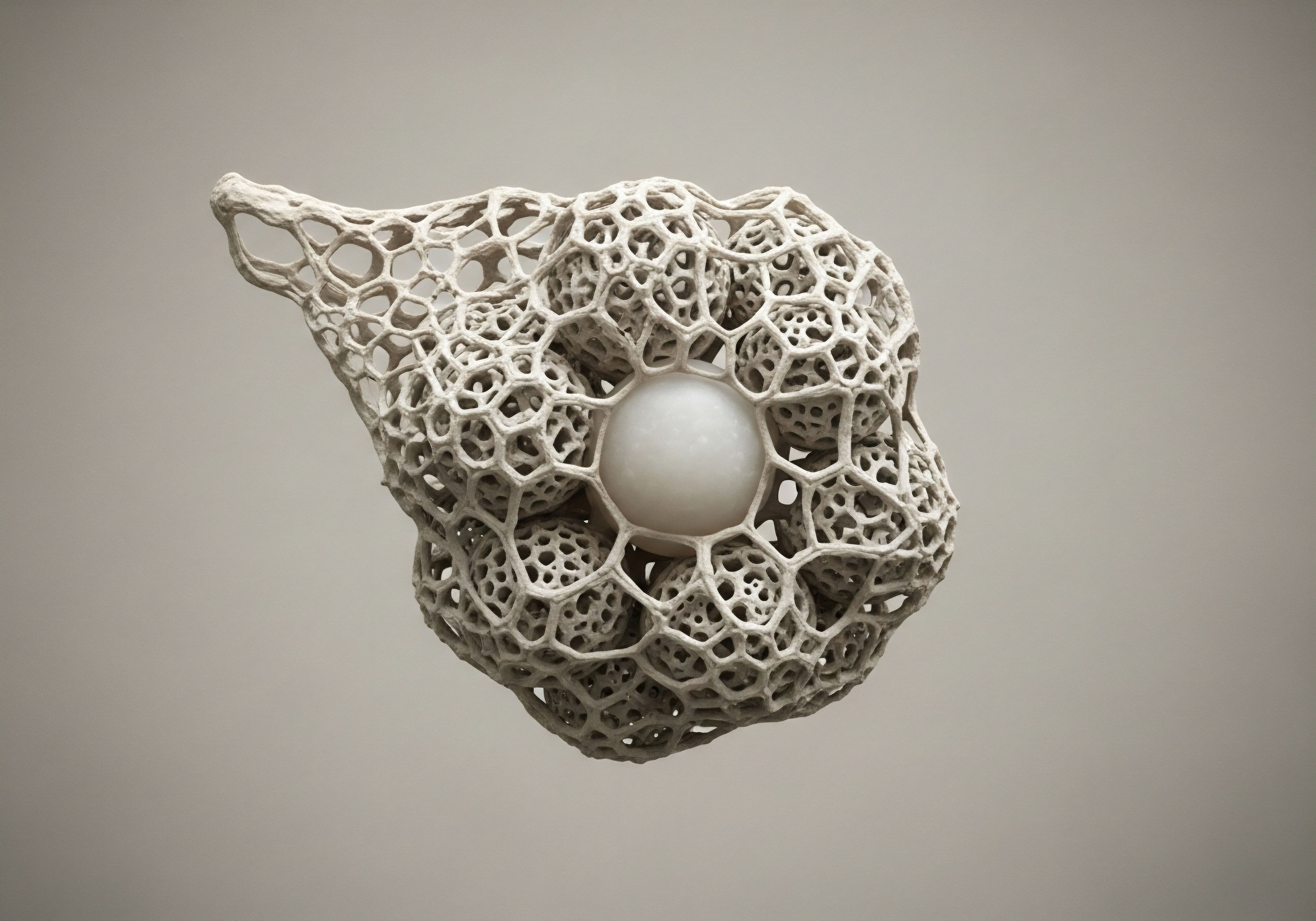
Think of your endocrine system as a vast, interconnected web of messengers and receivers. Hormones are the chemical messengers, traveling through the bloodstream to deliver specific instructions to target cells. These cells have receptors, which are like docking stations designed to receive a particular hormone.
When a hormone docks with its receptor, it triggers a cascade of events inside the cell, altering its function. This is how hormones regulate everything from your metabolic rate and mood to your immune response and libido. Lifestyle choices are the master regulators of this entire process. They influence how many messengers are sent, how sensitive the docking stations are, and how efficiently the cellular instructions are carried out.
Your body’s hormonal state is a direct reflection of the inputs it receives from your daily life.

The Cellular Environment Matters
Introducing therapeutic hormones into your system, such as testosterone or estrogen, is like sending a priority message through this network. The goal is to supplement a declining supply and ensure critical instructions are still being delivered. The environment of the cell receiving this message dictates the outcome.
A cell bathed in inflammatory molecules from a highly processed diet, or one that is resistant to insulin due to chronic sugar intake, will have compromised receptor sites. Its ability to hear and execute the hormonal command is diminished. Conversely, a cell supported by nutrient-dense foods, restorative sleep, and regular physical activity will have highly sensitive, functional receptors. It will respond to the therapeutic hormone with precision and efficiency.
This is the foundational principle for understanding the long-term implications of your choices. You are not merely a passive recipient of hormone therapy. You are the active curator of the biological environment in which it operates. Every meal, every workout, every hour of sleep is a decision that either amplifies or dampens the therapeutic signal.
This perspective shifts the focus from simply replacing a substance to holistically recalibrating an entire system. The therapy provides the tool; your lifestyle determines how skillfully that tool can be used to rebuild your physiological function and sense of well-being.

How Does Stress Disrupt Hormonal Balance?
Chronic stress provides a powerful example of this dynamic. The adrenal glands produce the hormone cortisol in response to perceived threats. In a healthy system, cortisol levels rise in the morning to promote wakefulness and fall at night to allow for sleep.
Chronic stress, be it from work deadlines, emotional turmoil, or poor sleep, keeps cortisol levels persistently elevated. This has significant consequences for hormonal health. The building blocks used to make cortisol are the same ones used to make sex hormones like testosterone and progesterone.
In a state of chronic stress, the body prioritizes survival by shunting these resources toward cortisol production, a phenomenon sometimes called “cortisol steal” or “pregnenolone steal.” This process actively depletes the very hormones you may be trying to supplement, creating a physiological headwind that can undermine the effectiveness of your therapy.


Intermediate
Understanding the foundational role of lifestyle allows us to examine the specific interactions between your daily habits and sophisticated hormonal protocols. These therapies are designed with precise biochemical objectives. Their long-term success hinges on a synergistic relationship with the choices you make, which can either facilitate or impede these objectives. Let’s explore the mechanics of how this plays out within common, targeted clinical protocols for both men and women.

Optimizing Male Endocrine System Support
A standard protocol for men experiencing the effects of low testosterone often involves weekly intramuscular injections of Testosterone Cypionate, supplemented with Gonadorelin and an aromatase inhibitor like Anastrozole. Each component has a distinct role, and each is influenced by lifestyle factors.
- Testosterone Cypionate This is the primary therapeutic agent, a bioidentical form of testosterone designed to restore levels to a healthy, functional range. Its effectiveness is measured by how well it alleviates symptoms like fatigue, low libido, and cognitive fog.
- Gonadorelin This peptide stimulates the pituitary gland to release Luteinizing Hormone (LH) and Follicle-Stimulating Hormone (FSH). This is critical for maintaining testicular function and preserving the body’s own capacity to produce testosterone, preventing the shutdown of the natural signaling pathway (the Hypothalamic-Pituitary-Gonadal axis).
- Anastrozole This is an aromatase inhibitor. The aromatase enzyme converts testosterone into estrogen. While some estrogen is necessary for male health, excess levels can lead to side effects like water retention, moodiness, and gynecomastia. Anastrozole blocks this conversion, helping to maintain a healthy testosterone-to-estrogen ratio.
Lifestyle choices directly impact the efficiency of this entire system. For instance, body fat is a primary site of aromatase activity. A man with a higher body fat percentage will naturally convert more testosterone to estrogen. This may necessitate a higher dose of Anastrozole to manage side effects. A nutritional plan that promotes fat loss and a consistent resistance training program can reduce overall aromatase activity, making the protocol more efficient and potentially reducing the need for ancillary medications.
The synergy between hormone therapy and lifestyle choices determines the ultimate physiological outcome.

The Impact of Nutrition and Exercise on TRT
The interaction between your choices and your protocol is constant and measurable. Consider these two pillars of health:
Nutrition’s Role A diet high in processed carbohydrates and sugar drives insulin resistance and systemic inflammation. Inflammation can blunt the sensitivity of androgen receptors, meaning the testosterone you administer has a weaker effect at the cellular level.
Conversely, a diet rich in healthy fats, quality proteins, and micronutrients provides the building blocks for endogenous hormone production and reduces the inflammatory load, allowing receptors to function optimally. Zinc, for example, is a mineral crucial for testosterone production and also acts as a natural aromatase inhibitor. Ensuring adequate intake through diet or supplementation can support the goals of the entire protocol.
Exercise as a Sensitizer Physical activity, particularly resistance training, is one of the most powerful ways to enhance a TRT protocol. Lifting weights increases the density and sensitivity of androgen receptors in muscle tissue. This means the testosterone in your system becomes more effective at stimulating protein synthesis, leading to improvements in muscle mass, strength, and metabolic rate.
The choice of exercise matters. While chronic, excessive endurance exercise can sometimes elevate cortisol and be counterproductive, a balanced routine incorporating strength training and moderate cardiovascular activity creates the ideal physiological environment for hormonal optimization.

Recalibrating the Female Endocrine System
For women navigating the complex hormonal shifts of perimenopause and post-menopause, protocols are designed to address deficiencies in estrogen, progesterone, and often testosterone. Lifestyle is an inseparable component of successful therapy.
| Therapeutic Agent | Primary Function | Key Lifestyle Interaction |
|---|---|---|
| Testosterone Cypionate (low dose) | Improves libido, energy, mood, and muscle tone. | Resistance training enhances muscle response and body composition changes. |
| Progesterone | Balances estrogen, supports sleep, and provides calming effects. | Stress management techniques (e.g. meditation, yoga) lower cortisol, allowing progesterone to work more effectively. |
| Estrogen (various forms) | Alleviates hot flashes, night sweats, and vaginal dryness; protects bone density. | A diet rich in calcium and vitamin D, combined with weight-bearing exercise, works synergistically to prevent osteoporosis. |
| Peptide Therapy (e.g. Ipamorelin) | Stimulates natural growth hormone release for recovery and body composition. | Administering peptides in a fasted state and ensuring adequate protein intake maximizes their anabolic effects. |
For women, managing blood sugar and inflammation is paramount. Fluctuations in blood sugar can exacerbate symptoms like hot flashes and mood swings, even when on therapy. A diet focused on whole foods, fiber, and protein helps stabilize insulin and glucose levels, creating a stable baseline upon which the hormone therapy can act.
Furthermore, the gut microbiome plays a crucial role in estrogen metabolism through an enzyme called beta-glucuronidase. A healthy gut, cultivated through a fiber-rich diet, helps ensure proper estrogen clearance, which is vital for maintaining hormonal balance and reducing long-term risks.


Academic
A sophisticated analysis of the long-term interaction between lifestyle and hormone therapy requires moving beyond symptom management to the cellular and molecular level. The central organizing principle is that lifestyle choices directly modulate the signaling environment of the entire organism.
Factors like nutrition, physical activity, and stress regulate the epigenetic expression of genes, the function of cellular receptors, and the activity of key metabolic enzymes. These modulations profoundly influence the risk-benefit profile and ultimate efficacy of any exogenous hormonal intervention. The discussion will focus on the interplay between metabolic health, specifically insulin sensitivity, and its downstream effects on hormone receptor function and inflammatory pathways.

Metabolic Health as the Master Regulator
The state of an individual’s metabolic health is arguably the most critical variable determining the long-term outcome of hormone replacement. Chronic hyperinsulinemia, a consequence of a diet high in refined carbohydrates and a sedentary lifestyle, creates a cascade of deleterious effects that directly conflict with the goals of hormonal optimization.
Insulin resistance at the cellular level leads to compensatory high levels of circulating insulin. This has several critical implications for a person on hormone therapy:
- Increased Aromatase Activity Adipose tissue is a primary site of the aromatase enzyme, which converts androgens to estrogens. Insulin promotes lipid storage (lipogenesis) and is strongly correlated with increased visceral adiposity. This excess adipose tissue functions as an endocrine organ, significantly upregulating aromatase activity. In a male on TRT, this means a greater portion of the administered testosterone is converted to estradiol, potentially leading to an unfavorable hormonal ratio and necessitating higher doses of an aromatase inhibitor. This introduces additional medication with its own potential side effects, complicating the protocol.
- Reduced Sex Hormone-Binding Globulin (SHBG) Insulin directly suppresses the liver’s production of SHBG. SHBG is a protein that binds to sex hormones, transporting them through the bloodstream. Lower SHBG levels result in a higher percentage of “free” or unbound testosterone and estrogen. While this might seem beneficial initially, chronically low SHBG is a hallmark of metabolic syndrome and is associated with an increased risk of type 2 diabetes and cardiovascular disease. It disrupts the body’s natural buffering system for hormone delivery, leading to less stable levels and potentially more aggressive hormonal effects at the tissue level.
- Inflammatory Signaling Insulin resistance is intrinsically linked to chronic low-grade inflammation. The resulting pro-inflammatory cytokines, such as TNF-α and IL-6, can interfere with hormone receptor signaling. This phenomenon, known as receptor desensitization, means that even with restored serum hormone levels, the target cells are less responsive. The message is being sent, but the receiver is functionally impaired.

What Is the Role of Receptor Sensitivity in Therapy Outcomes?
The ultimate success of hormone therapy is determined at the receptor level. The introduction of exogenous hormones is futile if the target cells cannot receive the signal. Lifestyle choices are potent modulators of receptor sensitivity.
Resistance exercise, for example, has been shown to increase the expression and sensitivity of androgen receptors (AR) in skeletal muscle. This is a primary mechanism through which exercise potentiates the effects of testosterone therapy, leading to superior outcomes in muscle accretion and metabolic function. Conversely, a sedentary lifestyle combined with a diet that promotes inflammation has the opposite effect, downregulating receptor function and creating a state of hormonal resistance.
| Lifestyle Factor | Biochemical Mechanism | Impact on Hormone Therapy |
|---|---|---|
| High Omega-6/Omega-3 Ratio | Promotes the synthesis of pro-inflammatory eicosanoids. | Increases systemic inflammation, potentially blunting receptor sensitivity and exacerbating side effects. |
| Consistent Resistance Training | Increases androgen receptor density in muscle; improves insulin sensitivity. | Enhances the anabolic and metabolic effects of testosterone; improves overall metabolic health. |
| Chronic Sleep Deprivation | Elevates cortisol and sympathetic nervous system tone; impairs glucose metabolism. | Antagonizes the effects of therapy by promoting a catabolic state and insulin resistance. |
| High Fiber/Polyphenol Intake | Supports a healthy gut microbiome and estrogen metabolism (via β-glucuronidase activity). | Crucial for women on HRT to ensure proper clearance of estrogen metabolites, reducing potential risks. |

A Systems Biology View of Long-Term Risk
The long-term data on hormone therapy, particularly from large-scale studies like the Women’s Health Initiative (WHI), highlight certain statistical risks, such as venous thromboembolism with oral estrogens or a potential increase in breast cancer diagnoses with combined synthetic progestins.
A systems biology perspective, informed by our understanding of lifestyle’s molecular impact, allows for a more personalized risk stratification. The risks identified in the WHI were based on a broad population with varying underlying health statuses and lifestyles, using older formulations.
Consider the risk of blood clots with oral estrogen. This is primarily due to the first-pass metabolism in the liver, which increases the synthesis of clotting factors. A lifestyle that promotes inflammation and endothelial dysfunction would logically amplify this risk.
Conversely, a patient with excellent metabolic health, a low inflammatory state maintained through diet and exercise, and who opts for a transdermal delivery system (which bypasses the first-pass liver metabolism) would have a profoundly different risk profile. Lifestyle choices, therefore, become a primary tool for risk mitigation, moving a patient from a population-based statistical risk to a personalized, and likely much lower, actual risk.

References
- Manson, JoAnn E. et al. “Menopausal Hormone Therapy and Long-term All-Cause and Cause-Specific Mortality ∞ The Women’s Health Initiative Randomized Trials.” JAMA, vol. 318, no. 10, 2017, pp. 927-938.
- Rosano, G. M. C. et al. “Menopausal hormone therapy and women’s health ∞ an update.” European Heart Journal, vol. 42, no. 33, 2021, pp. 3217-3219.
- Garnier, C. et al. “Hormone replacement therapy in postmenopausal women ∞ A review of the safety of estrogen and progestogen.” Maturitas, vol. 142, 2020, pp. 26-34.
- Vlachopoulos, C. et al. “The effect of testosterone on endothelial function.” Journal of Clinical Endocrinology & Metabolism, vol. 92, no. 8, 2007, pp. 3175-3181.
- Traish, A. M. et al. “The dark side of testosterone deficiency ∞ III. Cardiovascular disease.” Journal of Andrology, vol. 30, no. 5, 2009, pp. 477-494.
- Genazzani, A. R. et al. “Effect of long-term local or systemic hormone replacement therapy on post-menopausal mood disturbances. Influences of socio-economic and personality factors.” Maturitas, vol. 32, no. 1, 1999, pp. 47-53.
- Ryan, J. et al. “The effect of hormone replacement therapy on cognitive function in older women ∞ a randomised, placebo-controlled trial.” Medical Journal of Australia, vol. 190, no. 11, 2009, pp. 621-624.
- Espeland, Mark A. et al. “Effect of postmenopausal hormone therapy on cognitive function.” JAMA, vol. 289, no. 20, 2003, pp. 2663-2672.

Reflection
The information presented here provides a map of the intricate biological landscape where your choices and your therapy meet. It details the mechanisms and pathways that connect a decision made at the dinner table to a cellular response deep within your body. This knowledge is the foundation.
It moves you from being a passenger in your health journey to being the pilot. The data and protocols are essential tools, yet the true art of wellness lies in their application to your unique physiology and life context.

Where Do Your Choices Lead You?
Consider your own daily rhythms. How does your body feel after a night of deep, restorative sleep versus one that was short and interrupted? What is the difference in your energy and mental clarity when your meals are composed of whole, nutrient-dense foods compared to when they are rushed and processed?
This sensory, intuitive data is as valid as any lab report. It is the feedback from your own biological system. The path forward involves learning to listen to these signals with greater acuity and using this awareness to make choices that consistently support your body’s innate drive toward equilibrium. The goal is a state of vitality and function that allows you to engage with your life without compromise.