

Fundamentals
Your body is a finely tuned orchestra, a complex system of communication where hormones act as the messengers, carrying vital instructions from one part to another. You feel this system in your energy levels, your mood, your sleep quality, and your resilience to stress.
When you experience symptoms like persistent fatigue, unexplained weight changes, or shifts in your mental clarity, it is a direct signal that this internal communication network may be facing disruptions. These are not just abstract feelings; they are the tangible result of your unique biology at work. The source of these disruptions often lies within your genetic blueprint, the very code that instructs your body how to build and regulate itself.
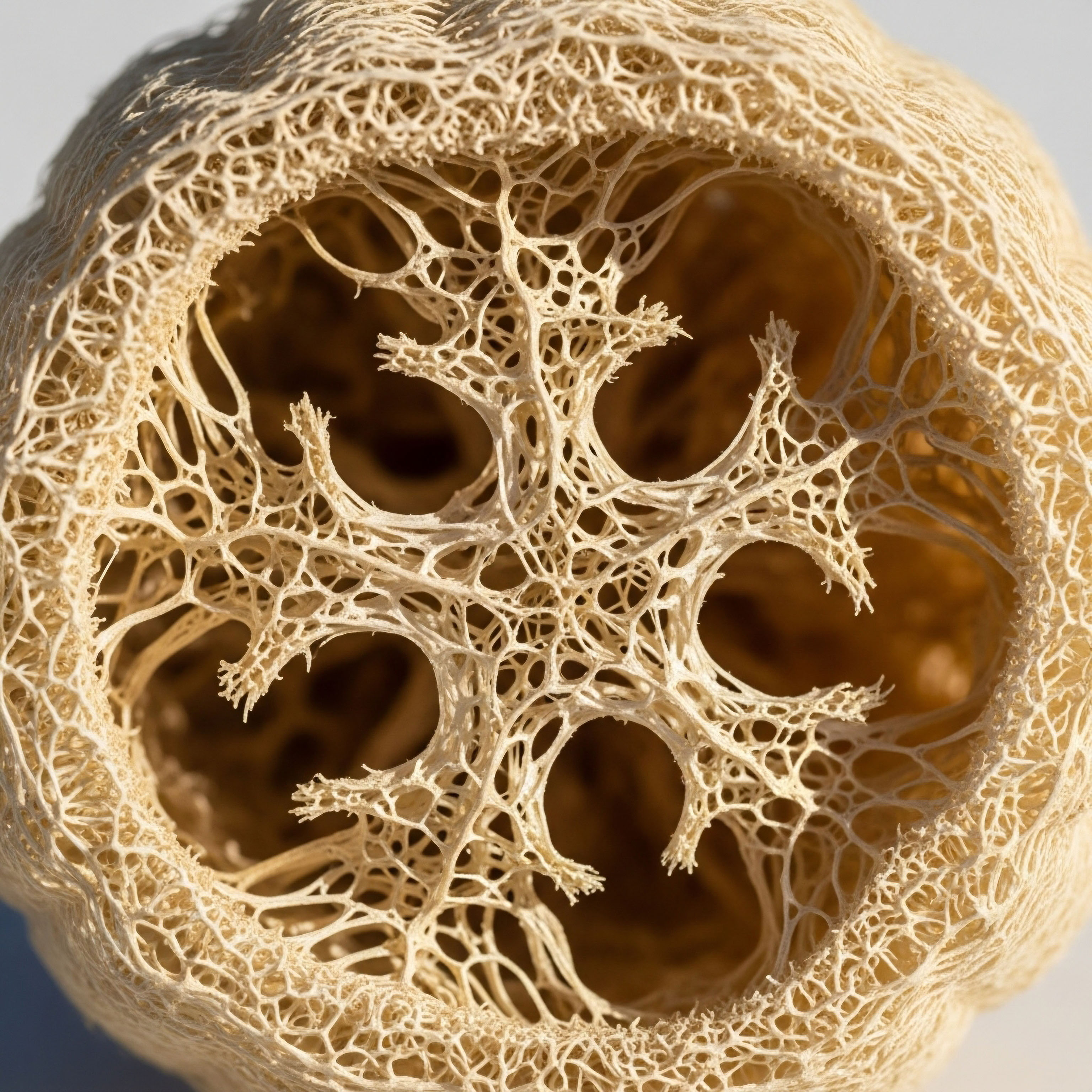
Genetic variations are subtle differences in your DNA sequence, the inherited instruction manual for your body. Think of them as slight variations in a recipe. Most of these variations are harmless, contributing to the diversity that makes each of us unique. Some variations, however, can alter the instructions for building components of your endocrine system.
This system includes glands like the thyroid, adrenals, and gonads, which produce and release hormones. A genetic variation might change how a hormone is produced, how it is transported through the bloodstream, or how it is received by a target cell. The long-term effects of these variations are deeply personal and can manifest over a lifetime, influencing your susceptibility to certain health conditions.
Genetic variations provide a foundational blueprint for your endocrine system, but they do not solely determine your health outcomes.

How Do Genes Influence Hormones?
The connection between your genes and your hormonal health Meaning ∞ Hormonal Health denotes the state where the endocrine system operates with optimal efficiency, ensuring appropriate synthesis, secretion, transport, and receptor interaction of hormones for physiological equilibrium and cellular function. is direct and profound. Genes contain the codes for producing proteins, and hormones are either proteins themselves or are synthesized by protein-based enzymes. A variation in a gene can lead to several outcomes:
- Altered Hormone Production A genetic change can affect the efficiency of an enzyme responsible for creating a hormone. This might result in lower-than-optimal levels of a crucial hormone like testosterone or thyroid hormone.
- Modified Hormone Receptors For a hormone to deliver its message, it must bind to a specific receptor on a cell, much like a key fitting into a lock. Genetic variations can change the shape of these receptors, making them more or less sensitive to the hormone.
- Changes in Hormone Transport Many hormones travel through the bloodstream attached to carrier proteins. Your genes dictate the structure of these proteins. A variation could affect how tightly a hormone is bound, influencing how much of it is readily available for your cells to use.
These subtle genetic shifts can predispose an individual to certain endocrine-related conditions. For instance, specific genetic markers are associated with an increased likelihood of developing Polycystic Ovary Syndrome Meaning ∞ Polycystic Ovary Syndrome (PCOS) is a complex endocrine disorder affecting women of reproductive age. (PCOS), a common endocrine disorder in women characterized by hormonal imbalances and metabolic issues. Similarly, certain genetic variants are known to play a role in the development of both type 1 and type 2 diabetes.

The Concept of Genetic Predisposition
It is important to understand that having a genetic variation linked to a particular condition does not mean you will inevitably develop it. It signifies a predisposition, an increased susceptibility. Your genetic makeup is one part of a larger equation. Environmental factors, lifestyle choices, and diet all interact with your genes to shape your health journey.
This interaction is at the heart of a field called epigenetics, which explores how external factors can modify how your genes are expressed without changing the DNA sequence itself. For example, exposure to endocrine-disrupting chemicals (EDCs) found in everyday products can trigger epigenetic changes that affect hormonal function. This means that while your genes provide the script, your life experiences and choices have a powerful influence on how that script is read.


Intermediate
Understanding that your genetic makeup influences your endocrine function Meaning ∞ Endocrine function describes the biological processes where specialized glands produce and secrete hormones directly into the bloodstream. is the first step. The next is to appreciate how this knowledge can be translated into precise clinical strategies. When we see a pattern of symptoms ∞ for instance, the persistent fatigue and low libido associated with low testosterone in men, or the complex constellation of issues in women with PCOS ∞ we are observing the functional outcome of an individual’s unique genetic and physiological landscape. Clinical protocols are designed to address these functional outcomes, recalibrating the system to restore optimal signaling.
The interplay between genetic predisposition Meaning ∞ Genetic predisposition signifies an increased likelihood of developing a specific disease or condition due to inherited genetic variations. and endocrine health becomes particularly clear when we examine conditions like monogenic diabetes. Unlike the more common forms of diabetes, monogenic diabetes results from a mutation in a single gene. Identifying the specific genetic cause is clinically significant because it dictates the most effective treatment.
For example, individuals with a mutation in the HNF1A gene respond much better to sulfonylurea medications than to insulin, a discovery that has transformed treatment for this subgroup of patients. This illustrates a core principle of personalized medicine ∞ a precise diagnosis based on genetic information allows for a targeted and more effective therapeutic intervention.

Genetic Insights into Common Endocrine Conditions
While monogenic diseases offer a clear link between a single gene and a condition, the genetic influence on more common endocrine disorders is typically polygenic, meaning it involves multiple genetic variations, each with a small effect. These variations, combined with environmental factors, contribute to the development of conditions like PCOS and autoimmune thyroid Meaning ∞ Autoimmune thyroid describes conditions where the body’s immune system mistakenly targets the thyroid gland, causing its dysfunction. disease.

Polycystic Ovary Syndrome (PCOS)
PCOS is a prime example of a complex endocrine disorder with a strong genetic component. It is characterized by a collection of symptoms, including irregular menstrual cycles, high levels of androgens (male hormones), and cysts on the ovaries. Research has identified several genes associated with PCOS, many of which are involved in insulin regulation and androgen production.
This genetic predisposition helps explain why PCOS often runs in families. From a clinical perspective, understanding this link informs treatment strategies, which often focus on managing insulin resistance Meaning ∞ Insulin resistance describes a physiological state where target cells, primarily in muscle, fat, and liver, respond poorly to insulin. with medications like metformin and addressing hormonal imbalances with targeted therapies.
Genetic testing can help differentiate between various forms of diabetes, leading to more personalized and effective treatment plans.

Autoimmune Thyroid Disease
Autoimmune thyroid conditions, such as Hashimoto’s thyroiditis and Graves’ disease, also have a significant genetic underpinning. Certain genes, particularly those within the human leukocyte antigen (HLA) complex, are known to increase susceptibility to these conditions. These genes are involved in the immune system’s ability to distinguish between self and non-self.
A genetic variation can make the immune system more likely to mistakenly attack the thyroid gland, leading to hormonal disruption. While we cannot change these underlying genetic predispositions, we can implement strategies to support immune function and manage the inflammatory processes that drive the disease.
The Role of Epigenetics in Endocrine Health
The concept of epigenetics Meaning ∞ Epigenetics describes heritable changes in gene function that occur without altering the underlying DNA sequence. provides a crucial bridge between our fixed genetic code and the dynamic nature of our health. Epigenetic modifications Meaning ∞ Epigenetic modifications are reversible chemical changes to DNA or its associated proteins, like histones, altering gene activity without changing the DNA sequence. are chemical tags that attach to our DNA, influencing which genes are turned on or off. These modifications can be influenced by a wide range of factors, including:
- Diet Nutritional components can directly influence DNA methylation, a key epigenetic mechanism.
- Environmental Exposures Chemicals like phthalates and bisphenol A (BPA) are known endocrine disruptors that can alter epigenetic patterns.
- Stress Chronic stress can lead to long-term changes in gene expression through epigenetic modifications.
These epigenetic changes can be heritable, meaning they can be passed down through generations. This has profound implications for understanding the long-term impact of environmental exposures Meaning ∞ Environmental exposures refer to a broad category of external factors encountered in daily life that interact with the human body and can influence physiological processes. on endocrine health. It suggests that the health choices and environmental conditions experienced by one generation can influence the endocrine function and disease risk of the next.
| Factor | Mechanism of Action | Clinical Relevance |
|---|---|---|
| Genetic Variations | Alter the structure or expression of proteins involved in hormone synthesis, transport, or reception. | Can create a predisposition to conditions like PCOS, diabetes, and thyroid disorders. |
| Epigenetic Modifications | Chemical tags on DNA that regulate gene expression in response to environmental cues. | Explains how lifestyle and environmental factors can influence long-term endocrine function and disease risk. |


Academic
The relationship between genetic architecture and endocrine function represents a sophisticated and dynamic interplay that extends beyond simple Mendelian inheritance. At a more granular level, we must consider the influence of non-coding DNA, higher-order chromatin structure, and the subtle yet cumulative effects of single nucleotide polymorphisms (SNPs) on endocrine homeostasis.
The traditional view of genetics as a static blueprint is giving way to a more fluid understanding of the genome as a responsive and adaptable entity, continuously interacting with its environment through epigenetic mechanisms. This perspective is essential for comprehending the long-term trajectory of endocrine health Meaning ∞ Endocrine health denotes the optimal functioning of the body’s endocrine glands and the balanced production and action of their secreted hormones. and disease.

What Are the Deeper Implications of Non-Coding DNA Variants?
A significant portion of the genetic variations Meaning ∞ Genetic variations are inherent differences in DNA sequences among individuals within a population. associated with common endocrine disorders, such as type 2 diabetes and PCOS, are located in non-coding regions of the genome. These regions, once dismissed as “junk DNA,” are now understood to contain regulatory elements like enhancers and promoters, which control the expression of distant genes.
A variant within an enhancer region, for example, might not alter a protein’s structure but can profoundly affect the amount of that protein produced. This is particularly relevant in the context of hormonal regulation, where the precise quantity of a hormone or its receptor can be as critical as its quality.
Recent research has illuminated the role of three-dimensional chromatin architecture in this process. Enhancers can physically loop around to interact with gene promoters that are thousands of base pairs away. Heritable variations in the proteins that mediate this looping or in the DNA sequences of the enhancers themselves can disrupt these long-range interactions, leading to dysregulated gene expression Meaning ∞ Gene expression defines the fundamental biological process where genetic information is converted into a functional product, typically a protein or functional RNA. and, consequently, endocrine dysfunction.
This provides a mechanistic explanation for how common variants with seemingly small effects can contribute to complex disease phenotypes over time.

How Does Genetic Risk Translate to Clinical Reality?
The clinical utility of genetic information in endocrinology is advancing rapidly. One of the most powerful applications is in risk stratification and diagnosis. For example, a Type 1 Diabetes Genetic Risk Score (T1DGRS) can be used to help differentiate between type 1 diabetes and monogenic forms of diabetes, especially in children who present with atypical features.
This is not merely an academic exercise; it has direct consequences for treatment and prognosis. A high T1DGRS, coupled with the presence of islet autoantibodies, strongly suggests an autoimmune etiology, whereas a low score in an antibody-negative individual would prompt further investigation for a monogenic cause.
The cumulative effect of multiple small-effect genetic variants, combined with epigenetic modifications, shapes an individual’s long-term endocrine health trajectory.
This approach, which integrates genetic data with clinical and biochemical markers, allows for a more nuanced understanding of an individual’s disease process. It moves us beyond a one-size-fits-all diagnostic label and toward a more personalized assessment of endocrine health. This is particularly important in conditions with heterogeneous presentations, like PCOS, where genetic markers may one day help to subtype patients based on their underlying pathophysiology, such as insulin resistance versus adrenal hyperandrogenism.

The Transgenerational Inheritance of Endocrine Disruption
Perhaps one of the most profound long-term implications of genetic and epigenetic interactions is the potential for transgenerational inheritance of endocrine disruption. Exposure to environmental factors, particularly endocrine-disrupting chemicals (EDCs), can induce epigenetic changes in germ cells (sperm and eggs).
These “epimutations” do not alter the DNA sequence but can be passed down to subsequent generations, influencing their endocrine function and disease susceptibility. For example, studies have shown that prenatal exposure to famine can lead to higher rates of obesity and diabetes in offspring, effects that are linked to epigenetic silencing of key metabolic genes.
This concept challenges the traditional boundaries of individual health, suggesting that the endocrine health of an individual is influenced by the environmental exposures of their ancestors. From a public health perspective, this raises significant concerns about the long-term impact of widespread environmental contaminants. From a clinical standpoint, it underscores the importance of taking a comprehensive patient history that includes not only personal but also familial and environmental exposures.
| Concept | Description | Long-Term Implication |
|---|---|---|
| Non-Coding DNA Variants | Variations in regulatory regions of DNA (enhancers, promoters) that control gene expression. | Subtle, lifelong alterations in hormone and receptor levels, contributing to polygenic disease risk. |
| Chromatin Architecture | The three-dimensional folding of DNA within the nucleus, which facilitates long-range gene regulation. | Heritable variations in chromatin structure can lead to systemic dysregulation of gene networks. |
| Transgenerational Epigenetics | The inheritance of epigenetic modifications through germ cells, influenced by ancestral environmental exposures. | The health impacts of environmental factors like EDCs may persist across multiple generations. |

References
- Florez, J. C. “Genetics of Common Endocrine Disease ∞ The Present and the Future.” The Journal of Clinical Endocrinology & Metabolism, vol. 100, no. 8, 2015, pp. 2853-62.
- Gore, A. C. et al. “Epigenetics meets endocrinology.” Journal of Endocrinology, vol. 211, no. 1, 2011, pp. 1-14.
- Ben Maamar, M. et al. “Impact of Endocrine Disruptors upon Non-Genetic Inheritance.” International Journal of Molecular Sciences, vol. 23, no. 3, 2022, p. 1474.
- “Children with diabetes and at least one non-autoimmune feature should be considered for monogenic diabetes testing.” The Journal of Clinical Endocrinology & Metabolism, 2025.
- “Polycystic ovary syndrome.” Wikipedia, Wikimedia Foundation, 2 Aug. 2025.

Reflection
The information presented here is a map, a detailed guide to the intricate landscape of your own biology. It reveals the deep connections between your inherited blueprint, the world you inhabit, and the way you feel every day. This knowledge is a powerful tool, shifting the perspective from one of passive symptom management to proactive, informed self-stewardship.
Your health journey is uniquely yours, a personal narrative written in the language of your genes and expressed through the dynamic functioning of your endocrine system. Understanding this language is the first, most critical step toward authoring your own story of vitality and well-being.














