Fundamentals
You feel it before you can name it. A persistent fatigue that sleep does not resolve. A subtle shift in your cognitive sharpness, where focus becomes a more deliberate act. These experiences are valid, tangible signals from within your body. They represent a disruption in a sophisticated, silent conversation that sustains your vitality.
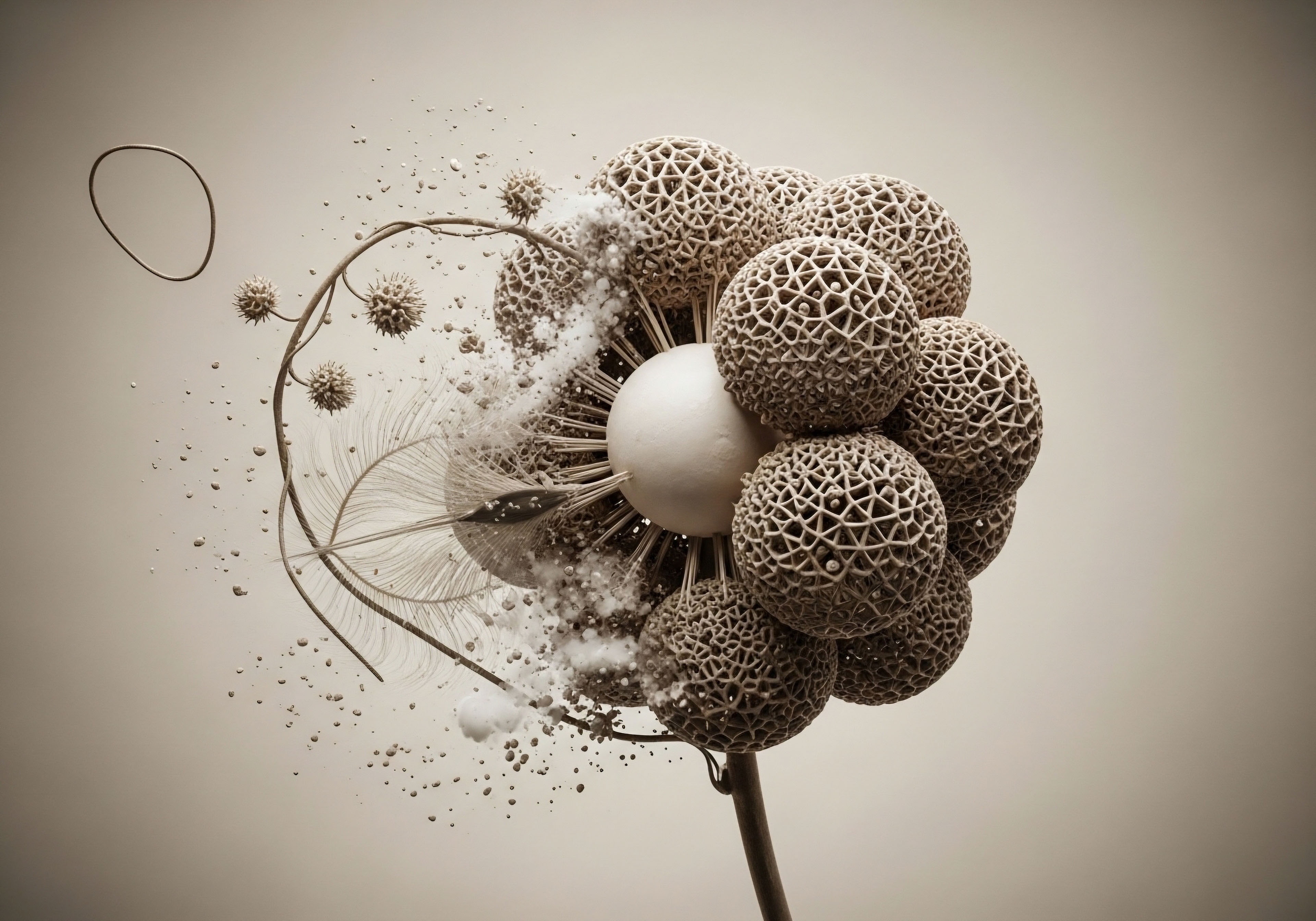
This conversation is conducted by hormones, the chemical messengers that form the body’s primary communication network. When these signals become unregulated, the messages are distorted, and the entire system begins to function inefficiently. The long-term effects of this internal miscommunication extend far beyond simple symptoms, touching every aspect of your systemic health.
Your body operates as an integrated system, much like a complex ecosystem. The endocrine system, the collection of glands that produce hormones, acts as the governing force of this internal environment. Hormones like testosterone, estrogen, progesterone, and growth hormone are potent molecules that travel through the bloodstream, instructing cells and organs on how to perform.
They regulate metabolism, manage energy, direct tissue repair, and influence mood. When the production and balance of these messengers are optimal, the system functions with a quiet efficiency. An imbalance, however, creates a cascade of consequences. For instance, declining testosterone in men is directly linked to a loss of bone density and muscle mass, creating a foundation for osteoporosis and physical frailty.
Similarly, the fluctuations and eventual decline of estrogen and progesterone during perimenopause and menopause in women can alter cardiovascular function and accelerate bone loss.
Unregulated hormones disrupt the body’s internal communication network, leading to a cascade of systemic health consequences.
The experience of living with hormonal dysregulation is one of profound biological dissonance. Your body is receiving incomplete or incorrect instructions. This manifests as a collection of symptoms that can feel disconnected yet share a common origin. Men may experience a decline in libido, energy, and mental acuity, while women may face vasomotor symptoms like hot flashes, sleep disturbances, and mood shifts.
These are the immediate, perceptible results of signal disruption. Over years and decades, these disruptions contribute to the development of chronic conditions. The metabolic shifts initiated by hormonal imbalances can lead to insulin resistance, increased visceral fat, and abnormal cholesterol levels, which are precursors to metabolic syndrome and cardiovascular disease. Understanding your symptoms as signals of a deeper systemic issue is the first step toward reclaiming biological harmony.

What Is the Endocrine System’s Role in Health?
The endocrine system is the bedrock of physiological regulation. It is a network of glands, including the pituitary, thyroid, adrenals, pancreas, and gonads, that synthesizes and secretes hormones directly into the circulatory system. These hormones then bind to specific receptors on target cells, initiating precise biological responses.
This mechanism allows for intricate control over processes that are slow-acting yet have long-lasting effects. For example, the hypothalamic-pituitary-gonadal (HPG) axis is a feedback loop that governs reproductive function and steroid hormone production in both men and women.
The hypothalamus releases gonadotropin-releasing hormone (GnRH), which signals the pituitary gland to release luteinizing hormone (LH) and follicle-stimulating hormone (FSH). These hormones, in turn, stimulate the gonads (testes or ovaries) to produce testosterone or estrogen. This entire axis is a self-regulating circuit, where the output hormones provide feedback to the hypothalamus and pituitary to modulate their own production. A disruption at any point in this axis can lead to systemic hormonal deficiencies.
Consider the role of this system in maintaining structural integrity. Testosterone and estrogen are critical for bone remodeling, a continuous process of breaking down old bone and forming new bone. When levels of these hormones decline, the rate of bone resorption can exceed the rate of bone formation, leading to a net loss of bone mass and the development of osteoporosis.
This condition makes bones fragile and susceptible to fractures, significantly impacting mobility and quality of life in later years. Likewise, these hormones are essential for maintaining lean muscle mass. Sarcopenia, the age-related loss of muscle, is accelerated by hormonal decline, contributing to weakness, reduced metabolic rate, and an increased risk of falls and injury. The endocrine system’s influence is thus woven into the very fabric of your physical structure.


Intermediate
Restoring hormonal balance is an exercise in re-establishing clear biological communication. When the body’s endogenous production of hormones falters, clinical protocols are designed to reintroduce the necessary signals in a precise and physiologic manner. These interventions are not about creating artificially high levels of hormones; they are about biochemical recalibration.
The goal is to restore the endocrine environment to one that supports optimal function, mitigating the long-term risks associated with hormonal deficiencies. Protocols like testosterone replacement therapy (TRT) for men and women, and growth hormone peptide therapy, are sophisticated tools for achieving this restoration.
Hormonal optimization protocols are tailored to the individual’s unique biochemistry, symptomology, and health goals. For men with diagnosed hypogonadism, TRT is a foundational intervention. The standard protocol often involves weekly intramuscular injections of Testosterone Cypionate. This approach provides a stable, consistent level of testosterone, avoiding the peaks and troughs associated with other delivery methods.
The protocol is more complex than simply administering testosterone. It includes ancillary medications to manage the downstream effects of hormonal shifts. For example, Anastrozole, an aromatase inhibitor, is used to control the conversion of testosterone to estrogen, preventing potential side effects like gynecomastia. Gonadorelin is often included to mimic the action of GnRH, stimulating the pituitary to maintain some natural testicular function and preserve fertility. This multi-faceted approach demonstrates a systems-based understanding of endocrinology.
Clinical protocols for hormonal health aim to recalibrate the body’s signaling environment, restoring function and mitigating long-term disease risk.

How Do Male and Female Protocols Differ?
While the principle of restoring balance is universal, the application differs significantly between sexes due to their distinct endocrine environments. Female hormonal optimization is intricate, often addressing the fluctuating interplay of estrogen, progesterone, and testosterone, particularly during the perimenopausal and postmenopausal transitions.

Hormone Optimization for Men
The primary goal for men is often the restoration of testosterone to a healthy physiological range to address symptoms of andropause and mitigate long-term health risks. A comprehensive male protocol is designed to re-establish the proper signaling within the HPG axis.
- Testosterone Cypionate ∞ This is a bioidentical form of testosterone delivered via injection. Weekly administration ensures stable serum levels, supporting consistent improvements in energy, mood, cognitive function, and libido.
- Gonadorelin ∞ A GnRH analogue, this peptide is used to prevent testicular atrophy and maintain endogenous testosterone production by directly stimulating the pituitary gland. This is a key component for men concerned about fertility.
- Anastrozole ∞ This oral medication is an aromatase inhibitor. It blocks the enzyme that converts testosterone into estrogen, helping to maintain an optimal testosterone-to-estrogen ratio and prevent estrogen-related side effects.
- Enclomiphene ∞ Sometimes used as an alternative or adjunct, this selective estrogen receptor modulator (SERM) can stimulate the pituitary to produce more LH and FSH, thereby increasing natural testosterone production.

Hormone Optimization for Women
For women, protocols are highly individualized based on their menopausal status and specific symptoms. The focus is on alleviating symptoms like vasomotor instability (hot flashes), sleep disruption, and mood changes, while also providing long-term protection against osteoporosis and cardiovascular disease.
- Testosterone Cypionate ∞ Women also produce and require testosterone for energy, libido, and bone health. Low-dose weekly subcutaneous injections (typically 0.1-0.2ml) can restore testosterone to youthful levels, significantly improving quality of life.
- Progesterone ∞ This hormone is prescribed based on menopausal status. For post-menopausal women, it is often used in conjunction with estrogen to protect the uterine lining. It also has calming effects that can aid sleep.
- Pellet Therapy ∞ This is an alternative delivery method where small pellets of bioidentical testosterone (and sometimes estradiol) are inserted under the skin, providing a slow, consistent release of hormones over several months.
Another class of therapies involves growth hormone peptides. These are not growth hormone itself, but secretagogues that stimulate the pituitary gland to release its own growth hormone in a natural, pulsatile manner. This approach is favored for its safety profile and its ability to work with the body’s own regulatory systems.
The combination of Ipamorelin and CJC-1295 is a common protocol. Ipamorelin is a ghrelin mimetic that causes a strong, clean pulse of GH release without affecting stress hormones like cortisol. CJC-1295 is a GHRH analogue that extends the duration of the GH pulse. Together, they create a synergistic effect, promoting benefits such as improved sleep quality, enhanced tissue repair, fat loss, and lean muscle preservation.
| Peptide | Mechanism of Action | Primary Benefits | Typical Administration |
|---|---|---|---|
| Sermorelin | GHRH Analogue (short-acting) | Increases natural GH pulses, improves sleep, supports recovery. | Daily subcutaneous injection, typically at night. |
| Ipamorelin | Ghrelin Mimetic / GHRP | Stimulates a strong, clean GH pulse without raising cortisol. | Daily or twice-daily subcutaneous injection. |
| CJC-1295 | GHRH Analogue (long-acting) | Sustains elevated GH and IGF-1 levels for extended periods. | Often combined with Ipamorelin for synergistic effect. |
| Tesamorelin | GHRH Analogue | Specifically targets visceral adipose tissue (belly fat). | Daily subcutaneous injection. |
| Component | Primary Role in Male Protocols | Primary Role in Female Protocols |
|---|---|---|
| Testosterone Cypionate | Foundation of therapy to restore physiological levels for systemic health. | Low-dose application to improve energy, libido, mood, and bone density. |
| Progesterone | Not typically used. | Crucial for uterine protection (if applicable) and often used for its calming effects. |
| Anastrozole | Manages estrogen conversion to prevent side effects. | Used occasionally with pellet therapy if aromatization is a concern. |
| Gonadorelin | Maintains testicular function and fertility signaling. | Not applicable. |


Academic
A deeper examination of hormonal dysregulation reveals a complex interplay between the body’s primary regulatory circuits. The long-term systemic consequences of unregulated hormones are a direct result of crosstalk and reciprocal influence between the hypothalamic-pituitary-gonadal (HPG) axis and the hypothalamic-pituitary-adrenal (HPA) axis.
The HPA axis is the central mediator of the stress response. Chronic activation of this system, a hallmark of modern life, exerts a potent suppressive effect on the HPG axis, creating a state of functional hypogonadism that can precede and exacerbate age-related hormonal decline. This interaction is a critical mechanism underlying the progression from hormonal imbalance to systemic pathologies like metabolic syndrome, neuroinflammation, and cardiovascular disease.
The HPA axis responds to perceived threats by releasing corticotropin-releasing hormone (CRH) from the hypothalamus. CRH stimulates the pituitary to secrete adrenocorticotropic hormone (ACTH), which in turn signals the adrenal glands to produce cortisol. While this is an adaptive short-term survival mechanism, chronic elevation of cortisol initiates a series of deleterious effects on the HPG axis.
Elevated cortisol directly suppresses the hypothalamic release of GnRH, thereby downregulating the entire gonadal steroid production cascade. This creates a physiological environment where the body prioritizes immediate survival over long-term functions like reproduction and tissue repair. The result is a blunted production of testosterone and estradiol, independent of age. This HPA-induced suppression of gonadal function contributes significantly to the clinical picture of hormonal deficiency, accelerating the onset of symptoms and increasing the severity of long-term health risks.
The chronic activation of the HPA stress axis exerts a direct suppressive force on the HPG axis, accelerating hormonal decline and promoting systemic disease.

How Does HPA Axis Crosstalk Drive Metabolic Disease?
The convergence of HPA axis overactivity and HPG axis suppression creates a perfect storm for metabolic derangement. Cortisol’s primary metabolic function is to increase blood glucose to provide energy for a “fight or flight” response. It achieves this by promoting gluconeogenesis in the liver and inducing insulin resistance in peripheral tissues like muscle and fat.
When cortisol levels are chronically elevated, this state of insulin resistance becomes persistent. Concurrently, the decline in testosterone and estrogen further compromises metabolic health. Testosterone plays a direct role in promoting insulin sensitivity and maintaining lean muscle mass, which is the body’s largest reservoir for glucose disposal. Estradiol has protective effects on endothelial function and lipid metabolism.
The synergistic effect of high cortisol and low gonadal hormones is profound. The body is simultaneously being flooded with glucose and rendered incapable of efficiently utilizing it. This leads to hyperinsulinemia, as the pancreas works harder to overcome the resistance.
This state promotes the storage of excess energy as visceral adipose tissue (VAT), the metabolically active fat surrounding the internal organs. VAT is not merely a passive storage depot; it is an endocrine organ in its own right, secreting inflammatory cytokines that further exacerbate insulin resistance and systemic inflammation.
This vicious cycle is the core pathophysiology of metabolic syndrome, characterized by central obesity, hypertension, dyslipidemia, and hyperglycemia. The initial hormonal imbalance, driven by the interplay of the HPA and HPG axes, thus becomes the engine of progressive, systemic metabolic disease. Understanding this deep biological connection is paramount for designing effective, long-term therapeutic strategies that address both the symptoms and the root cause of hormonal dysregulation.

References
- Viau, V. “Functional cross-talk between the hypothalamic-pituitary-gonadal and -adrenal axes.” Journal of Neuroendocrinology, vol. 14, no. 6, 2002, pp. 506-13.
- Araujo, A. B. et al. “Clinical review ∞ Endogenous testosterone and mortality in men ∞ a systematic review and meta-analysis.” The Journal of Clinical Endocrinology & Metabolism, vol. 96, no. 10, 2011, pp. 3007-19.
- Davis, Susan R. et al. “Menopause.” Nature Reviews Disease Primers, vol. 1, 2015, article number 15004.
- Kassi, Eva. “HPA axis abnormalities and metabolic syndrome.” Endocrine Abstracts, vol. 41, 2016, EP295.
- Basaria, Shehzad. “Male hypogonadism.” The Lancet, vol. 383, no. 9924, 2014, pp. 1250-63.
- Teichman, S. L. et al. “CJC-1295, a long-acting growth hormone-releasing factor analog.” The Journal of Clinical Endocrinology & Metabolism, vol. 91, no. 3, 2006, pp. 799-805.
- Whirledge, S. and John A. Cidlowski. “Glucocorticoids, stress, and fertility.” Minerva endocrinologica, vol. 35, no. 2, 2010, pp. 109-25.
- Traish, Abdulmaged M. et al. “The dark side of testosterone deficiency ∞ I. Metabolic syndrome and erectile dysfunction.” Journal of Andrology, vol. 30, no. 1, 2009, pp. 10-22.
Reflection
The information presented here forms a map of your internal biological landscape. It details the communication pathways, the regulatory circuits, and the systemic consequences of their disruption. This knowledge is a tool, providing a framework for understanding the signals your body sends. Your personal health narrative is written in the language of biochemistry.
Learning to interpret this language allows you to move from a reactive position to one of proactive stewardship of your own well-being. The path forward involves a partnership with clinical science, applying these principles to your unique physiology to recalibrate your system and build a foundation for sustained vitality.