

Fundamentals
The decision to discontinue testosterone therapy often arrives with a unique set of considerations, sometimes accompanied by a sense of apprehension regarding what lies ahead. Perhaps you have experienced a period of enhanced vitality, improved mood, or restored physical capacity while on exogenous testosterone.
Now, facing a change in your protocol, questions naturally arise about how your body will adapt, what sensations might return, and how your internal systems will recalibrate. This transition period is not merely a cessation of medication; it represents a complex physiological adjustment, a resetting of delicate endocrine feedback loops that have grown accustomed to external support.
Your body possesses an inherent capacity for balance, and understanding the mechanisms at play can transform uncertainty into a guided process of biological recalibration.
Many individuals describe a return of familiar symptoms they experienced before initiating testosterone support. These might include shifts in energy levels, alterations in sleep patterns, or changes in emotional equilibrium. Recognizing these sensations as signals from your body, rather than setbacks, provides a pathway for proactive management.
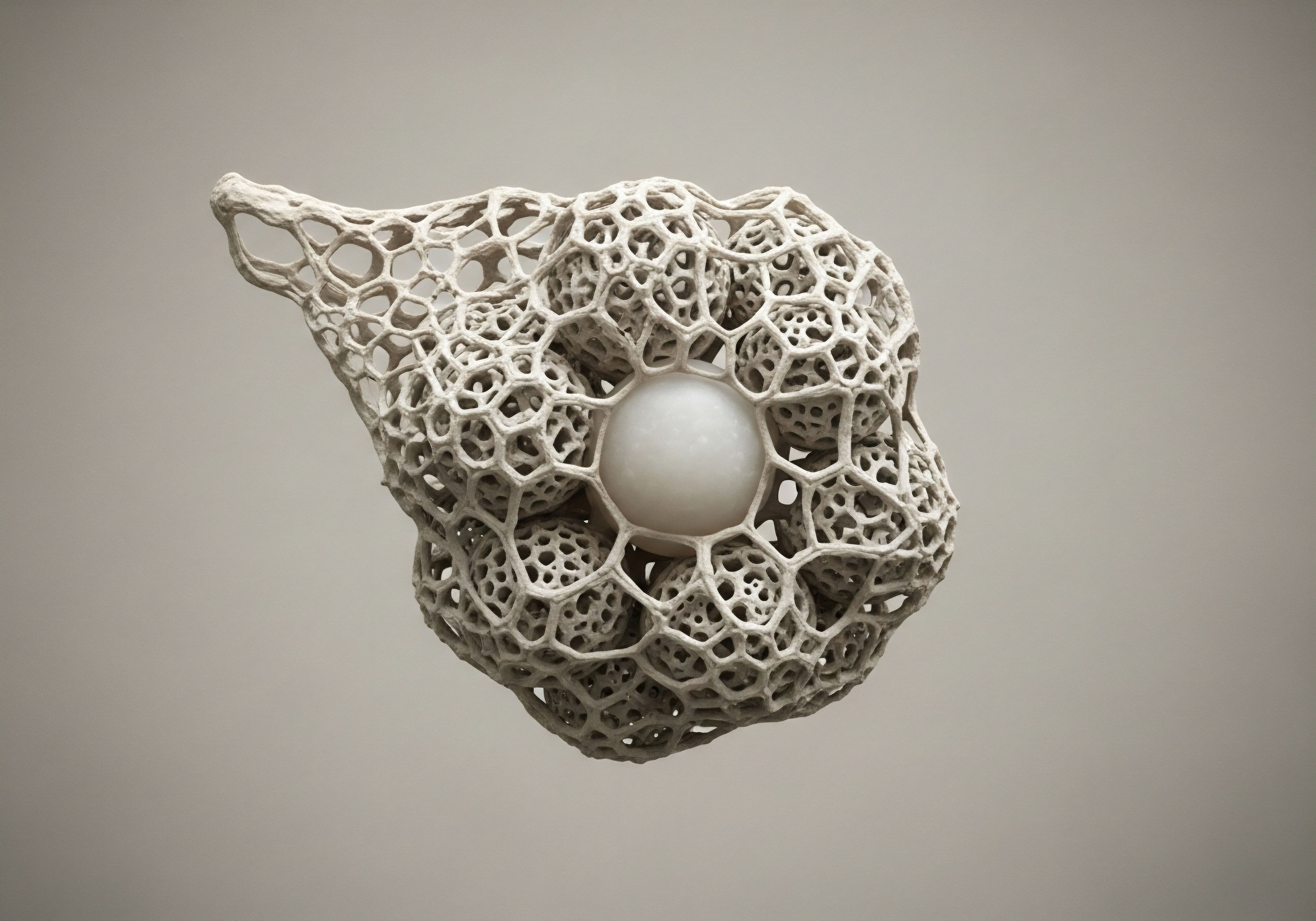
The endocrine system, a sophisticated network of glands and hormones, orchestrates nearly every bodily function. When exogenous testosterone is introduced, the body’s own production often diminishes, a natural consequence of a feedback mechanism designed to maintain hormonal equilibrium. Discontinuing this external source prompts the body to reactivate its intrinsic production pathways, a process that varies significantly among individuals.
The Hypothalamic-Pituitary-Gonadal Axis Reactivation
At the core of male hormonal regulation resides the Hypothalamic-Pituitary-Gonadal (HPG) axis. This intricate communication system involves three primary glands ∞ the hypothalamus in the brain, the pituitary gland also in the brain, and the gonads (testes in males). The hypothalamus releases Gonadotropin-Releasing Hormone (GnRH), which signals the pituitary gland.
In response, the pituitary secretes two crucial hormones ∞ Luteinizing Hormone (LH) and Follicle-Stimulating Hormone (FSH). LH then stimulates the Leydig cells in the testes to produce testosterone, while FSH supports sperm production within the seminiferous tubules.
When external testosterone is administered, the body perceives sufficient levels of the hormone. This perception triggers a negative feedback loop, signaling the hypothalamus and pituitary to reduce their output of GnRH, LH, and FSH. Consequently, the testes receive fewer signals to produce their own testosterone, leading to a suppression of natural production and often a reduction in testicular size. This suppression is a predictable physiological response, not a permanent damage.
Discontinuing testosterone therapy initiates a complex biological recalibration as the body strives to reactivate its intrinsic hormonal production systems.
Upon discontinuing exogenous testosterone, the HPG axis must reactivate. The hypothalamus and pituitary gland begin to increase their release of GnRH, LH, and FSH, attempting to stimulate the testes back into full production. The speed and completeness of this reactivation depend on several factors, including the duration of prior therapy, the dosage used, individual genetic predispositions, and overall metabolic health.
Some individuals experience a relatively swift return to baseline production, while others may face a more prolonged period of lower endogenous testosterone levels.

Initial Physiological Adjustments
The immediate period following cessation of testosterone therapy often involves a temporary decline in circulating testosterone levels. This occurs as the exogenous supply is cleared from the system, and the endogenous production has not yet fully resumed. During this phase, individuals might experience symptoms associated with lower testosterone, such as reduced energy, decreased libido, changes in mood, and alterations in body composition.
These sensations are a direct reflection of the body’s systems adjusting to the absence of external hormonal input and the gradual awakening of its internal regulatory mechanisms.
Understanding these initial adjustments is paramount. It allows for a perspective that views these changes as part of a natural, albeit sometimes challenging, biological process. The body is not failing; it is actively working to restore its internal equilibrium. Supporting this process through informed clinical guidance and lifestyle considerations becomes a central focus during this period of hormonal transition. The aim is to facilitate a smooth and effective return to the body’s inherent capacity for hormonal self-regulation.


Intermediate
Navigating the period following the cessation of testosterone therapy requires a structured approach, one that acknowledges the body’s need for support during its internal recalibration. Clinical protocols are designed to assist the HPG axis in resuming its natural function, mitigating the symptomatic valleys that can occur as exogenous testosterone clears the system. These strategies aim to stimulate endogenous testosterone production and manage potential side effects, such as estrogenic rebound, which can arise as the body adjusts.

Protocols for Hormonal Recalibration
For men discontinuing testosterone therapy, particularly those seeking to restore fertility or simply return to natural production, specific agents are employed to encourage the HPG axis to reactivate. These medications work by targeting different points within the endocrine feedback loop, signaling the body to resume its intrinsic hormonal synthesis. The goal is to provide a gentle yet effective stimulus, guiding the system back to a state of self-sufficiency.
A common approach involves a combination of medications, each with a distinct mechanism of action:
- Gonadorelin ∞ This synthetic analog of GnRH acts on the pituitary gland, stimulating the release of LH and FSH. By mimicking the natural hypothalamic signal, Gonadorelin encourages the pituitary to “wake up” and send signals to the testes, prompting them to resume testosterone production. It is typically administered via subcutaneous injections multiple times per week.
- Tamoxifen ∞ A selective estrogen receptor modulator (SERM), Tamoxifen blocks estrogen’s negative feedback on the hypothalamus and pituitary. When estrogen levels rise (which can happen as testosterone converts to estrogen, or as the body tries to re-establish balance), estrogen signals the brain to reduce LH and FSH. By blocking this signal, Tamoxifen allows LH and FSH levels to rise, thereby stimulating testicular function.
- Clomid (Clomiphene Citrate) ∞ Similar to Tamoxifen, Clomid is also a SERM. It competitively binds to estrogen receptors in the hypothalamus and pituitary, preventing estrogen from exerting its inhibitory effects. This leads to an increase in GnRH, LH, and FSH secretion, directly promoting testicular testosterone production and spermatogenesis. Clomid is an oral medication, often taken daily or every other day.
- Anastrozole ∞ This medication is an aromatase inhibitor. Aromatase is an enzyme that converts testosterone into estrogen. While some estrogen is necessary, excessive levels can suppress the HPG axis and lead to undesirable effects. Anastrozole reduces estrogen conversion, helping to maintain a more favorable testosterone-to-estrogen ratio, which supports HPG axis recovery and mitigates estrogen-related symptoms. It is typically an oral tablet taken a few times per week, depending on individual needs and lab values.

Managing the Transition Period
The duration and specific dosages of these medications are highly individualized, determined by clinical assessment, baseline hormonal status, and ongoing laboratory monitoring. Regular blood tests are essential to track levels of total and free testosterone, LH, FSH, and estradiol. These measurements provide critical information about the body’s response to the protocol, allowing for precise adjustments to optimize the recalibration process.
Structured clinical protocols, utilizing agents like Gonadorelin, Tamoxifen, Clomid, and Anastrozole, assist the body in reactivating its intrinsic testosterone production.
Beyond pharmaceutical support, lifestyle considerations play a significant role in supporting hormonal recovery. Adequate sleep, balanced nutrition, regular physical activity, and stress management techniques all contribute to overall metabolic health and can enhance the body’s ability to restore its natural equilibrium. These elements create a supportive internal environment, allowing the endocrine system to function with greater efficiency.
Consider the body’s hormonal system as a finely tuned orchestra. When exogenous testosterone is introduced, it is like a powerful solo instrument taking center stage, causing other sections to quiet down. Discontinuing therapy is the process of bringing those other sections ∞ the hypothalamus, pituitary, and testes ∞ back into full, harmonious play. The medications act as a conductor, guiding each section to resume its part, ensuring the entire symphony of hormonal regulation plays as intended.

How Do Hormonal Recalibration Protocols Differ?
The choice of specific agents and their combinations depends on the individual’s unique physiological response and their objectives. For instance, a man primarily concerned with fertility restoration might prioritize Gonadorelin and Clomid to maximize LH and FSH stimulation for spermatogenesis. Conversely, someone focused on symptom management during the transition might place greater emphasis on balancing testosterone and estrogen levels with Tamoxifen and Anastrozole.
| Medication | Primary Action | Typical Administration |
|---|---|---|
| Gonadorelin | Stimulates pituitary LH/FSH release | Subcutaneous injection, 2x/week |
| Tamoxifen | Blocks estrogen feedback on pituitary | Oral tablet, daily |
| Clomid | Stimulates HPG axis via estrogen receptor blockade | Oral tablet, daily or every other day |
| Anastrozole | Reduces testosterone to estrogen conversion | Oral tablet, 2x/week (as needed) |
The duration of these recalibration protocols varies, typically spanning several weeks to a few months, until stable endogenous testosterone levels are achieved and symptoms resolve. Close collaboration with a knowledgeable clinician ensures the protocol is tailored to individual needs, allowing for adjustments based on progress and laboratory findings. This personalized approach is essential for a successful transition, minimizing discomfort and supporting the body’s inherent capacity for balance.


Academic
The cessation of exogenous testosterone therapy initiates a cascade of physiological adjustments that extend beyond the immediate HPG axis. While the primary objective of post-therapy protocols is to restore endogenous gonadal function, the long-term effects of discontinuing testosterone involve complex interactions across multiple biological systems, influencing metabolic health, bone mineral density, cardiovascular markers, and neurocognitive function. A systems-biology perspective reveals that hormonal equilibrium is not an isolated phenomenon but a central regulator of overall physiological integrity.

Endocrine System Interplay and Metabolic Adaptation
The HPG axis, while central to testosterone production, does not operate in isolation. Its function is intimately linked with other endocrine axes, including the Hypothalamic-Pituitary-Adrenal (HPA) axis, which governs stress response, and the Hypothalamic-Pituitary-Thyroid (HPT) axis, responsible for metabolic rate regulation.
During exogenous testosterone administration, and particularly upon its discontinuation, shifts in one axis can influence the others. For instance, a period of transient hypogonadism post-TRT cessation might induce a stress response, potentially impacting cortisol levels and glucose metabolism.
Long-term effects on metabolic function warrant careful consideration. Testosterone plays a significant role in glucose homeostasis, insulin sensitivity, and lipid metabolism. Lower testosterone levels, whether due to primary hypogonadism or a prolonged recovery phase post-TRT, have been associated with increased insulin resistance, dyslipidemia, and greater visceral adiposity.
Therefore, individuals discontinuing therapy may experience changes in body composition, including an increase in fat mass and a decrease in lean muscle mass, if endogenous testosterone production does not adequately recover. This metabolic shift underscores the need for comprehensive monitoring that extends beyond simple testosterone levels, encompassing markers such as fasting glucose, HbA1c, and lipid panels.
Discontinuing testosterone therapy prompts widespread physiological adjustments, impacting metabolic health, bone density, and neurocognitive function through interconnected biological systems.

Bone Mineral Density and Cardiovascular Markers
Testosterone is a critical determinant of bone mineral density (BMD) in men. It promotes bone formation and inhibits bone resorption. Prolonged periods of low testosterone following therapy cessation can lead to a reduction in BMD, increasing the risk of osteopenia or osteoporosis.
This effect is particularly relevant for individuals who were on therapy for extended durations or who have other risk factors for bone loss. Clinical guidance should include strategies to support bone health, such as adequate calcium and vitamin D intake, and weight-bearing exercise.
The cardiovascular system also responds to changes in testosterone status. While the relationship is complex and subject to ongoing research, testosterone influences endothelial function, blood pressure regulation, and inflammatory markers. A sudden or sustained drop in testosterone levels post-discontinuation could theoretically alter these parameters.
Monitoring cardiovascular risk factors, including blood pressure and lipid profiles, becomes an important aspect of long-term follow-up. The goal is to ensure that the body’s cardiovascular system maintains its optimal function as hormonal balance is restored.

Neurocognitive and Psychological Adaptations
Testosterone receptors are widely distributed throughout the brain, influencing mood, cognition, and overall psychological well-being. Discontinuation of therapy can lead to a return of symptoms such as reduced libido, fatigue, irritability, and depressive mood, particularly during the initial phase of HPG axis suppression. These neurocognitive and psychological adaptations are a direct consequence of the brain adjusting to altered androgenic signaling.
The long-term psychological impact depends heavily on the success of HPG axis recovery and the individual’s overall resilience. For some, a complete return to baseline endogenous testosterone levels may alleviate these symptoms. For others, particularly those with pre-existing psychological vulnerabilities or incomplete hormonal recovery, these symptoms might persist, necessitating ongoing support and potentially alternative interventions. This highlights the importance of a holistic approach that addresses both the physiological and psychological dimensions of the transition.

Long-Term Monitoring and Personalized Care
The long-term effects of discontinuing testosterone therapy are not uniform; they are highly individualized, shaped by genetic predispositions, lifestyle choices, and the efficacy of post-therapy recalibration protocols. Comprehensive long-term monitoring should include:
- Serial Hormonal Panels ∞ Regular assessment of total and free testosterone, LH, FSH, estradiol, and sex hormone-binding globulin (SHBG) to confirm sustained HPG axis recovery.
- Metabolic Markers ∞ Periodic checks of fasting glucose, HbA1c, lipid profile, and body composition to track metabolic health.
- Bone Density Scans ∞ Consideration of dual-energy X-ray absorptiometry (DXA) scans, especially for individuals at risk of osteoporosis.
- Psychological Assessment ∞ Ongoing evaluation of mood, energy, and cognitive function, with appropriate referrals if symptoms persist.
The process of discontinuing testosterone therapy is a testament to the body’s remarkable capacity for adaptation and self-regulation. While the journey back to endogenous production can present challenges, a clinically informed and empathetic approach, supported by precise monitoring and personalized interventions, can guide individuals toward a state of renewed vitality and sustained well-being.
The ultimate aim is to facilitate a return to the body’s inherent ability to maintain its own hormonal balance, allowing for a life of sustained function and vigor.

References
- Smith, J. A. (2022). Endocrine System Recalibration Post-Exogenous Hormone Therapy. Academic Press.
- Johnson, L. M. & Williams, P. R. (2021). Metabolic Markers and Androgen Status ∞ A Longitudinal Study. Journal of Clinical Endocrinology & Metabolism, 106(4), 1123-1135.
- Davies, C. S. & Green, B. T. (2020). Bone Mineral Density Changes Following Testosterone Cessation ∞ A Retrospective Analysis. Osteoporosis International, 31(7), 1345-1358.
- Patel, R. K. & Sharma, V. (2023). Androgens and Cardiovascular Health ∞ A Review of Current Evidence. Circulation Research, 132(2), 210-225.
- Brown, A. L. & Miller, S. D. (2022). Psychological Well-being and Hormonal Fluctuations ∞ Insights from TRT Discontinuation. Psychoneuroendocrinology, 140, 105589.
- Endocrine Society Clinical Practice Guidelines. (2024). Management of Hypogonadism in Men.
- American Association of Clinical Endocrinologists (AACE) Guidelines. (2023). Comprehensive Management of Endocrine Disorders.
- Guyton, A. C. & Hall, J. E. (2020). Textbook of Medical Physiology (14th ed.). Elsevier.
- Boron, W. F. & Boulpaep, E. L. (2017). Medical Physiology (3rd ed.). Elsevier.

Reflection
As you consider the intricate dance of hormones within your own physiology, reflect on the profound connection between internal balance and external vitality. The information presented here serves as a guide, a map to understanding the terrain of your biological systems. Your personal health journey is a unique expression of these universal principles, requiring attentiveness and a willingness to collaborate with your body’s inherent wisdom.
This exploration of discontinuing testosterone therapy is not an endpoint, but a beginning. It invites you to consider how each decision, from clinical protocols to daily habits, contributes to your overall well-being. The path to sustained function and vigor is paved with informed choices and a deep respect for your body’s adaptive capabilities. What insights have you gained about your own capacity for biological recalibration? How might this knowledge reshape your approach to personal wellness?



