

Fundamentals
You may feel it as a persistent mental haze, a frustrating inability to recall information that was once readily available, or a sense of being perpetually overwhelmed. These experiences are data points. They are your body’s method of communicating a change in its internal environment.
This internal world is governed by a sophisticated communication network, and at the heart of its response to pressure and demand is the Hypothalamic-Pituitary-Adrenal (HPA) axis. This system is your primary stress-response mechanism, a finely tuned survival circuit designed to mobilize energy and focus your resources when you face a challenge.
The HPA axis operates through a precise cascade of signals. When your brain perceives a stressor, the hypothalamus releases a molecule that signals the pituitary gland. The pituitary, in turn, releases a different hormone that travels to the adrenal glands, located atop your kidneys. This final step prompts the release of cortisol.
In short bursts, cortisol is incredibly useful. It sharpens your focus, increases blood sugar for immediate energy, and modulates inflammation. Once the perceived threat passes, a negative feedback loop is meant to shut the system down, returning cortisol levels to a healthy baseline. This is a biological design of profound elegance, intended to manage acute challenges and then return to a state of equilibrium, or homeostasis.
The HPA axis is the body’s central stress response system, designed for short-term survival, but its prolonged activation can lead to systemic consequences.
Dysregulation occurs when this system is activated too intensely, too frequently, or for too long. The relentless demands of modern life can create a state of chronic activation, preventing the “off-switch” from working correctly. Instead of a temporary surge, cortisol levels can remain elevated for extended periods.
This sustained exposure to high cortisol begins to alter the very architecture and function of the brain. The cognitive symptoms you experience ∞ the brain fog, the memory lapses, the difficulty concentrating ∞ are direct physiological consequences of this prolonged state of alarm. Your brain, in an effort to protect itself from the unceasing flood of stress hormones, begins to adapt in ways that can unfortunately undermine its own performance.

The Brain’s Communication Breakdown
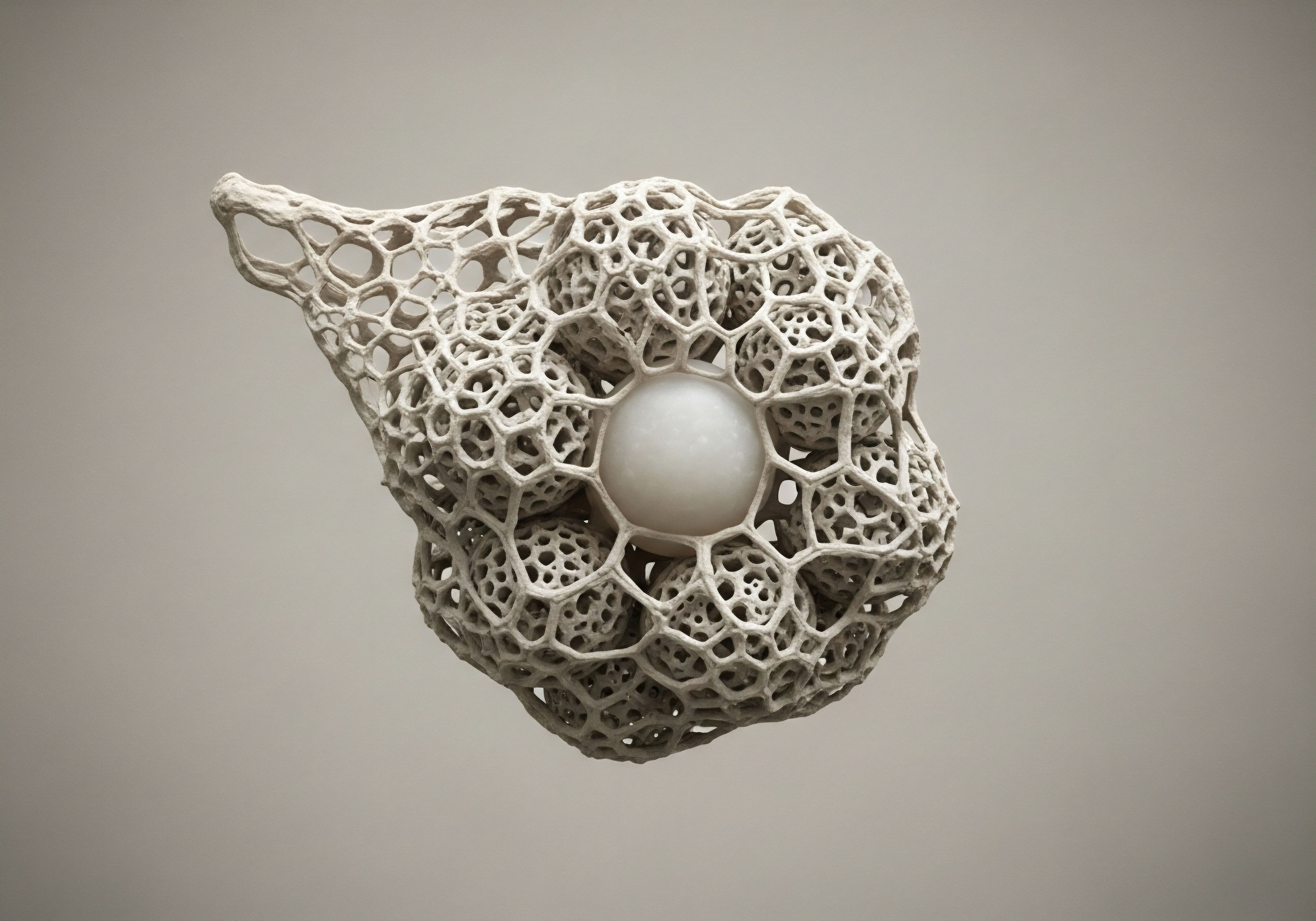
To understand the cognitive effects, it is helpful to visualize your brain as a dense network of connections. Communication between brain cells, or neurons, happens at junctions called synapses. The efficiency of this communication is vital for learning, memory, and clear thought. Prolonged exposure to high levels of cortisol disrupts this delicate process.
It can lead to a phenomenon known as excitotoxicity, where excessive signaling can damage and even destroy neurons. This is particularly true in brain regions that are dense with cortisol receptors, areas that are critical for higher-order cognitive functions.
Two of the most affected regions are:
- The Hippocampus ∞ This seahorse-shaped structure is central to learning and the formation of new memories. It is exceptionally rich in cortisol receptors, making it highly sensitive to stress signals. When the hippocampus is continuously exposed to high cortisol, its ability to form and retrieve memories is impaired. This can manifest as difficulty remembering recent events or learning new information.
- The Prefrontal Cortex (PFC) ∞ Located at the front of your brain, the PFC is your executive control center. It governs attention, decision-making, problem-solving, and emotional regulation. HPA axis dysregulation can weaken the connections in the PFC, leading to the familiar feelings of being easily distracted, struggling with complex tasks, and having a shorter fuse emotionally.
The initial feelings of cognitive disruption are your brain’s direct response to an internal hormonal imbalance. It is a biological signal that the system designed to protect you is now operating under a load it was not designed to carry long-term. Understanding this connection is the first step in recognizing that these cognitive changes are not a personal failing but a physiological state that can be addressed by restoring balance to the underlying systems.


Intermediate
Moving beyond the initial recognition of symptoms requires a deeper look at the biological mechanisms driving cognitive changes. When HPA axis dysregulation becomes chronic, the body’s cells, particularly in the brain, begin to adapt to the relentless presence of cortisol. This adaptation leads to a state known as glucocorticoid receptor (GR) resistance.
Imagine knocking on a door repeatedly; eventually, the person inside might stop answering. Similarly, when cortisol constantly “knocks” on its receptors, the receptors can become downregulated or less sensitive. This desensitization has profound and paradoxical consequences. The brain and immune cells no longer respond effectively to cortisol’s signal to calm down, which can lead to a state of unchecked, low-grade inflammation throughout the body and brain ∞ a condition known as neuroinflammation.
This state of GR resistance also disrupts the HPA axis’s own negative feedback loop. The hippocampus and hypothalamus, now less sensitive to cortisol, fail to send the “stop” signal effectively. The result is that the adrenal glands may continue to produce cortisol, creating a self-perpetuating cycle of high cortisol and receptor resistance.
This process is a key component of what scientists call allostatic load ∞ the cumulative “wear and tear” on the body and brain as they struggle to adapt to chronic stress. High allostatic load is directly associated with poorer performance in executive function and memory.

The Interplay of Hormonal Systems
The HPA axis does not operate in isolation. Its function is deeply intertwined with other major hormonal systems, most notably the Hypothalamic-Pituitary-Gonadal (HPG) axis, which governs reproductive function and produces sex hormones like testosterone and estrogen. These two axes exist in a reciprocal relationship.
Under normal conditions, healthy levels of testosterone and estrogen help to modulate and restrain the HPA axis response. However, chronic activation of the HPA axis has an inhibitory effect on the HPG axis. The body, perceiving a constant state of emergency, effectively decides to down-regulate functions it deems non-essential for immediate survival, including reproduction and long-term metabolic maintenance.
This can lead to decreased production of testosterone in men and dysregulated estrogen and progesterone levels in women, which has its own set of cognitive consequences.
Both testosterone and estrogen are potent neuromodulators that support cognitive health. They play critical roles in maintaining neuronal structure, supporting synaptic plasticity, and influencing neurotransmitter systems that regulate mood and focus. When their levels decline due to HPA-axis-induced suppression, the cognitive effects of high cortisol are compounded. This creates a complex clinical picture where symptoms of “brain fog” or memory decline are driven by multiple interconnected hormonal imbalances.
Chronic stress creates a cascade of hormonal disruptions, where the suppression of sex hormones by the HPA axis further compounds cognitive difficulties.

Phases of HPA Dysregulation and Cognitive Symptoms
HPA axis dysregulation is not a static condition. It often progresses through stages, each with a distinct biochemical profile and a corresponding set of cognitive and physical symptoms. Understanding these phases can help validate an individual’s experience as their symptoms evolve over time.
| Phase of Dysregulation | Primary Cortisol Pattern | Common Cognitive Symptoms | Associated Physical Sensations |
|---|---|---|---|
| Phase 1 ∞ Acute Alarm | High Cortisol, Intact Feedback |
Heightened alertness, but with emerging difficulty in complex problem-solving. A feeling of being “wired but tired.” |
Increased heart rate, anxiety, sleep disturbances (difficulty falling asleep). |
| Phase 2 ∞ Resistance | Sustained High Cortisol, GR Resistance |
Noticeable memory lapses, impaired concentration, significant brain fog, and reduced mental stamina. Executive functions like planning and organization become difficult. |
Persistent fatigue, increased inflammation, cravings for high-sugar or high-fat foods, weight gain around the midsection. |
| Phase 3 ∞ Exhaustion | Low Cortisol (Hypocortisolism) |
Profound cognitive fatigue, poor memory recall, emotional flatness, and an inability to handle even minor stressors. A feeling of being completely “burnt out.” |
Extreme exhaustion, increased susceptibility to illness, low blood pressure, dizziness. |

Restoring Systemic Balance through Clinical Protocols
Addressing the cognitive effects of HPA axis dysregulation requires a systems-based approach. The goal is to recalibrate the body’s internal communication networks. This can involve targeted interventions designed to support hormonal balance and reduce allostatic load.
For instance, when chronic stress has suppressed the HPG axis, protocols like Testosterone Replacement Therapy (TRT) for men or carefully managed hormone therapy for women can be instrumental. Restoring testosterone or estrogen to optimal levels can help re-establish their modulatory effects on the HPA axis, improve neurotransmitter function, and directly support cognitive processes.
In men, a typical TRT protocol might involve weekly injections of Testosterone Cypionate, often combined with Gonadorelin to maintain the body’s own signaling pathways. For women, low-dose Testosterone Cypionate or Progesterone may be used to restore balance, particularly during perimenopause and post-menopause when the HPG axis is naturally undergoing significant changes.
Additionally, certain peptide therapies can support the body’s signaling systems. Peptides like Sermorelin or CJC-1295/Ipamorelin stimulate the body’s own production of growth hormone, which has a complex and often beneficial relationship with the HPA axis and cognitive function. These protocols are not about simply replacing a single hormone but about providing the necessary inputs to encourage the entire endocrine system to return to a state of healthier, more resilient function.


Academic
A granular analysis of the long-term cognitive sequelae of HPA axis dysregulation reveals a cascade of neurobiological changes at the cellular and molecular levels. The sustained elevation of glucocorticoids, or the subsequent state of hypocortisolism, incites structural and functional remodeling in brain regions that are densely populated with mineralocorticoid receptors (MRs) and glucocorticoid receptors (GRs).
The hippocampus, prefrontal cortex, and amygdala are primary targets, and the damage incurred in these areas provides a direct neuroanatomical correlation for the observed deficits in memory, executive function, and emotional regulation.

Neurotoxicity and Structural Remodeling in the Hippocampus
The hippocampus is perhaps the most studied region in the context of stress-induced cognitive decline due to its high density of GRs and its crucial role in declarative memory formation and spatial navigation. Chronic exposure to elevated cortisol initiates a process of dendritic atrophy, particularly in the CA3 subfield of the hippocampus.
This involves the retraction and simplification of dendritic branches, which are the primary structures for receiving synaptic inputs. This structural degradation physically disconnects neurons from their communication networks, impairing the processes of long-term potentiation (LTP), the molecular basis of memory formation.
Furthermore, prolonged glucocorticoid exposure actively suppresses adult neurogenesis in the dentate gyrus of the hippocampus. The birth of new neurons is a critical component of cognitive flexibility and memory consolidation. Its inhibition contributes to a reduced capacity for new learning and can exacerbate mood disorders that often co-occur with HPA dysregulation.
In the most severe cases, the combination of dendritic atrophy, suppressed neurogenesis, and glutamate-mediated excitotoxicity can lead to a measurable reduction in hippocampal volume, a finding consistently observed in individuals with chronic stress-related disorders and a key feature in the pathophysiology of neurodegenerative diseases like Alzheimer’s.
Sustained high cortisol levels physically reshape critical brain areas, shrinking neuronal connections and inhibiting the birth of new brain cells.

Executive Dysfunction and the Prefrontal Cortex
The prefrontal cortex (PFC) is the seat of executive function, responsible for working memory, attentional control, and goal-directed behavior. Like the hippocampus, the PFC is sensitive to glucocorticoids, and chronic stress induces a similar process of dendritic retraction in its pyramidal neurons.
This structural change undermines the synaptic connectivity required for maintaining and manipulating information in working memory. The cognitive result is an inability to filter distractions, impaired decision-making, and a loss of cognitive flexibility. Individuals may find themselves stuck in rigid, habitual thought patterns, unable to adapt to new information or solve complex problems. This is because the PFC’s top-down control over other brain regions, including the emotionally-driven amygdala, is weakened, leading to heightened emotional reactivity and impulsivity.
How Does HPA Dysregulation Alter Neurotransmitter Systems?
The cognitive deficits stemming from HPA axis dysregulation are also mediated by profound changes in key neurotransmitter systems. Cortisol’s influence extends to the synthesis, release, and reuptake of several critical chemical messengers, altering the brain’s entire communication landscape.
| Neurotransmitter System | Effect of Chronic HPA Axis Dysregulation | Resulting Cognitive and Behavioral Impact |
|---|---|---|
| Glutamate |
Excessive release, leading to excitotoxicity. This over-activates NMDA receptors, causing a massive influx of calcium that can trigger cell death pathways. |
Neuronal damage, particularly in the hippocampus. Contributes directly to memory impairment and learning deficits. |
| GABA (Gamma-Aminobutyric Acid) |
Dysregulation of GABAergic inhibition. Initially, there may be an increase to counteract excitotoxicity, but chronic stress can lead to a functional reduction in GABA’s calming effects. |
Increased anxiety, hypervigilance, and an inability to “turn off” the stress response. Contributes to a state of neural hyperexcitability. |
| Dopamine |
Blunted dopamine signaling in the PFC. Chronic stress can reduce dopamine release and downregulate D1 receptors, which are crucial for working memory. |
Anhedonia (loss of pleasure), poor motivation, and deficits in attention and executive function. Affects goal-directed behavior. |
| Serotonin |
Complex and often bidirectional effects. Chronic stress can deplete serotonin precursors and alter receptor sensitivity, contributing to mood dysregulation. |
Depressive symptoms, anxiety, obsessive thoughts, and sleep disturbances. Affects emotional regulation and cognitive processing speed. |
| Acetylcholine |
Reduced cholinergic transmission. Acetylcholine is vital for attention and memory encoding. Chronic stress can impair its function, linking HPA dysregulation to cognitive decline in aging. |
Impaired attention, reduced alertness, and significant deficits in memory formation and retrieval. |

The Role of Neuroinflammation and Microglial Activation
A critical pathway linking HPA dysregulation to cognitive decline is neuroinflammation. Glucocorticoid receptor resistance in the brain’s immune cells, the microglia, is a key event. Under normal conditions, cortisol helps keep microglial activation in check. When GR resistance develops, microglia can shift to a pro-inflammatory state, releasing cytokines like TNF-α and IL-1β.
These inflammatory molecules are directly toxic to neurons, further impairing synaptic plasticity and neurogenesis. This creates a vicious cycle ∞ stress causes GR resistance, which leads to neuroinflammation, which in turn exacerbates neuronal damage and further dysregulates the HPA axis. This inflammatory state is now understood to be a central mechanism in the development of depression and a significant risk factor for the progression of age-related neurodegenerative diseases.

References
- Kim, E. J. Pellman, B. & Kim, J. J. (2015). Stress effects on the hippocampus ∞ a critical review. Learning & Memory, 22(9), 411 ∞ 416.
- McEwen, B. S. (2017). Neurobiological and systemic effects of chronic stress. Chronic Stress (Thousand Oaks, Calif.), 1, 2470547017692328.
- Lupien, S. J. McEwen, B. S. Gunnar, M. R. & Heim, C. (2009). Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nature Reviews Neuroscience, 10(6), 434 ∞ 445.
- Sousa, N. & Almeida, O. F. X. (2012). Corticosteroids and mood ∞ from animal models to clinical practice. In Handbook of Behavioral Neuroscience (Vol. 21, pp. 283-306). Elsevier.
- Sternberg, E. M. (2006). Neural regulation of innate immunity ∞ a coordinated nonspecific host response to pathogens. Nature Reviews Immunology, 6(4), 318 ∞ 328.
- de Kloet, E. R. Joëls, M. & Holsboer, F. (2005). Stress and the brain ∞ from adaptation to disease. Nature Reviews Neuroscience, 6(6), 463 ∞ 475.
- Sapolsky, R. M. (2000). Glucocorticoids and hippocampal atrophy in neuropsychiatric disorders. Archives of General Psychiatry, 57(10), 925 ∞ 935.
- Miller, A. H. & Raison, C. L. (2016). The role of inflammation in depression ∞ from evolutionary imperative to modern treatment target. Nature Reviews Immunology, 16(1), 22 ∞ 34.
- Arnsten, A. F. (2009). Stress signalling pathways that impair prefrontal cortex structure and function. Nature Reviews Neuroscience, 10(6), 410 ∞ 422.
- Wingenfeld, K. & Wolf, O. T. (2014). HPA axis alterations in mental disorders ∞ impact on memory and its relevance for therapeutic interventions. CNS Neuroscience & Therapeutics, 20(8), 701-711.

Reflection

Translating Knowledge into Personal Insight
You have journeyed through the intricate biological pathways that connect your internal stress response system to the clarity of your thoughts. This information serves a purpose beyond academic understanding. It provides a framework for reinterpreting your personal experience. The moments of mental fog, the frustrating search for a word, the feeling of being overwhelmed ∞ these are not character flaws.
They are signals from a biological system operating under immense strain. Your body is not failing you; it is communicating with you in the most direct language it has ∞ the language of physiology.
This knowledge invites you to become a more compassionate observer of your own state. It encourages a shift in perspective, from self-criticism to self-curiosity. What are the inputs that place demand on your system? How does your body respond? Recognizing these patterns is the foundational step toward reclaiming your cognitive vitality.
The path forward is one of recalibration, of consciously working to restore the elegant balance that your body is designed to maintain. This journey is inherently personal, and the insights you have gained are your map and compass, empowering you to navigate toward a state of renewed function and well-being.



