

Fundamentals
Perhaps you have noticed a subtle shift in your daily experience ∞ a persistent weariness that sleep does not resolve, a diminished spark in your usual pursuits, or a sense that your body is simply not responding as it once did.
These feelings, often dismissed as inevitable aspects of aging or daily stress, frequently point to a deeper, more systemic imbalance within your biological architecture. Understanding these internal signals represents the first step toward reclaiming your vitality and functional capacity. Your body communicates through a complex network of chemical messengers, and when these messages become garbled or insufficient, the impact on your well-being can be profound.
The endocrine system, a sophisticated internal messaging service, orchestrates nearly every physiological process. Hormones, the chemical agents of this system, regulate metabolism, energy levels, mood, cognitive sharpness, and physical performance. They influence how you sleep, how your immune system functions, and even your reproductive health.
When these vital chemical signals are out of sync, whether due to the natural progression of age, persistent stress, or environmental influences, a cascade of symptoms can arise. These symptoms might include a lack of energy, mental fogginess, changes in body composition, or shifts in emotional regulation.
Hormonal balance forms the foundation for enduring health, energy, and overall well-being.
A decline in hormonal equilibrium can contribute to long-term health challenges. These include cardiovascular system concerns, bone density reduction, and metabolic dysregulation. Addressing these imbalances proactively offers a path to support long-term health, sustain vigor, and elevate overall well-being. This proactive stance moves beyond merely alleviating symptoms; it establishes a robust physiological foundation.

The Body’s Internal Communication System
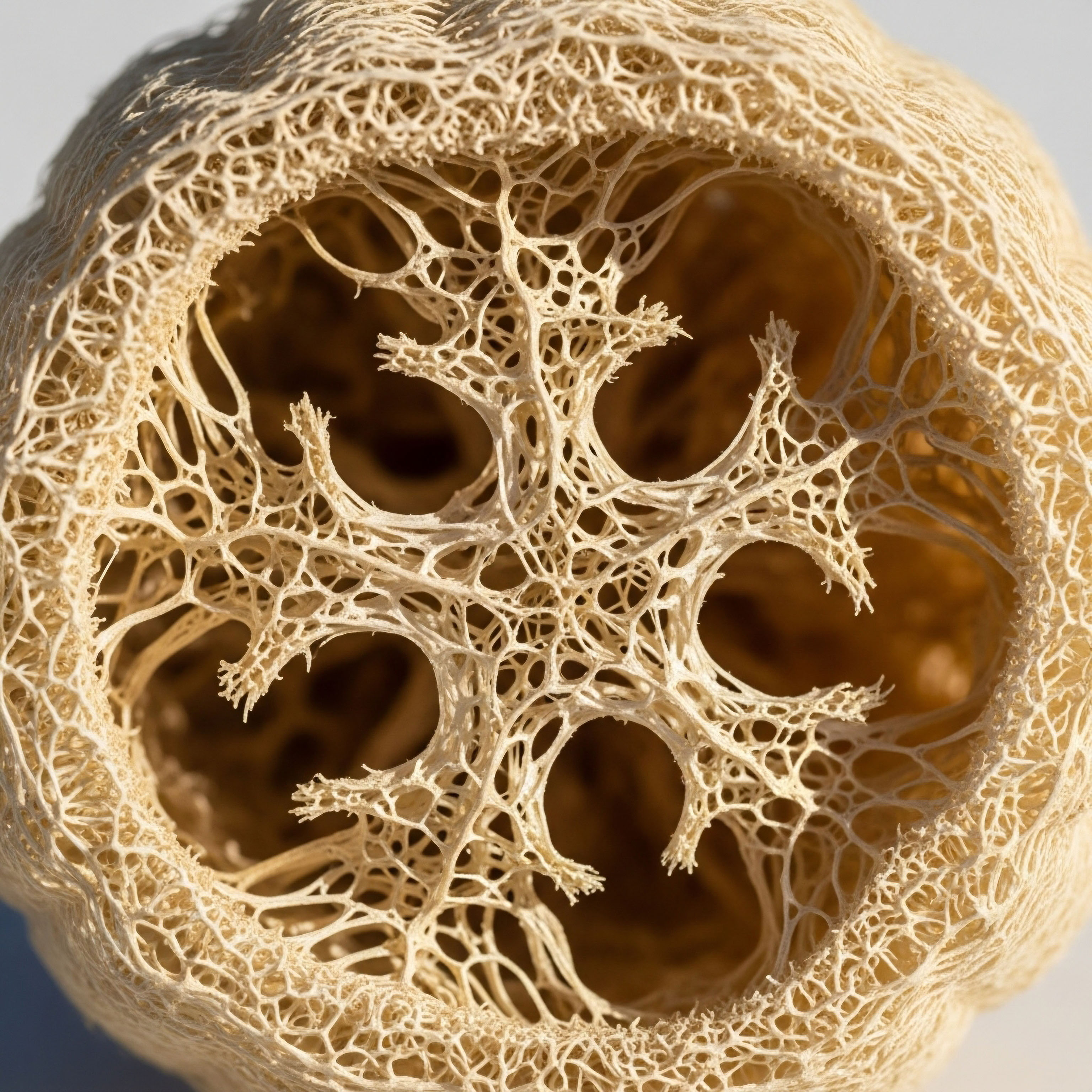
The human body operates through a remarkable system of communication, where specialized glands release hormones directly into the bloodstream. These hormones then travel to target cells and tissues, delivering specific instructions. This intricate process ensures that various bodily functions are coordinated and maintained within optimal ranges.
Consider the adrenal glands, which produce cortisol, a hormone vital for stress response and metabolism. When cortisol levels are consistently elevated due to chronic stress, it can disrupt other hormonal pathways, leading to widespread systemic effects.
The nervous system and the endocrine system are intimately connected, working in concert to regulate and coordinate bodily activities. This connection is particularly evident in the hypothalamic-pituitary-gonadal (HPG) axis, a central regulatory pathway. The hypothalamus, a region in the brain, releases neurohormones that direct the pituitary gland.
The pituitary, often called the “master gland,” then secretes hormones that control peripheral endocrine glands, such as the gonads (testes in men, ovaries in women). This hierarchical cascade ensures precise control over hormone production throughout the body.
Peripheral endocrine glands, including the adrenal glands, thyroid gland, and gonads, respond to pituitary signals by releasing their own hormones. These hormones exert widespread effects on target tissues, modulating metabolism, immune system activity, and reproductive processes. A tightly regulated feedback loop governs the neuroendocrine system. Peripheral hormones often send signals back to the hypothalamus and pituitary, either inhibiting or stimulating further hormone release. This feedback mechanism ensures that hormone levels remain within a healthy range, preventing overproduction or underproduction.

Why Hormonal Balance Matters for Longevity?
Maintaining hormonal equilibrium is not solely about feeling better today; it significantly influences your health trajectory over decades. Hormones impact cellular repair, inflammatory responses, and even genetic expression. When these systems are balanced, the body’s capacity for self-regulation and resilience is enhanced. This translates into a reduced susceptibility to age-related decline and chronic health conditions.
For instance, balanced levels of hormones like testosterone and estrogen contribute to maintaining bone mineral density, supporting cardiovascular health, and preserving cognitive function. These protective effects extend beyond mere symptom management, contributing to a longer, more vibrant life. The objective is to support the body’s innate intelligence, allowing it to function optimally and resist the wear and tear of time.
Optimizing hormonal balance supports the body’s inherent capacity for self-regulation and resilience.
Consider the impact on metabolic health. Hormones such as insulin, thyroid hormones, and cortisol play critical roles in regulating blood sugar, energy expenditure, and fat storage. Dysregulation in any of these can lead to insulin resistance, weight gain, and increased inflammation, all of which accelerate biological aging. By addressing hormonal imbalances, individuals can improve metabolic markers, supporting a healthier body composition and reducing the risk of metabolic syndrome.
The long-term benefits extend to mental and emotional well-being. Hormones directly influence neurotransmitter activity, impacting mood, stress response, and sleep quality. Balanced hormonal states contribute to emotional stability, improved stress adaptation, and more restorative sleep cycles. These elements are fundamental to a sustained sense of well-being and cognitive sharpness throughout life.


Intermediate
Moving beyond the foundational understanding of hormonal systems, we can now consider the specific clinical protocols designed to restore and maintain optimal hormonal balance. These interventions are not merely about replacing what is missing; they represent a strategic recalibration of the body’s intricate biochemical signaling. The aim is to support physiological function, allowing individuals to experience renewed vitality and improved health markers.
The application of targeted hormonal optimization protocols requires a precise understanding of individual needs, guided by comprehensive laboratory assessments and a thorough clinical evaluation. These protocols often involve specific therapeutic agents, each with a distinct mechanism of action, working to re-establish a harmonious internal environment.

Testosterone Replacement Therapy for Men
For men experiencing symptoms of low testosterone, often referred to as hypogonadism or andropause, Testosterone Replacement Therapy (TRT) offers a well-established pathway to improved well-being. Symptoms can include persistent fatigue, reduced muscle mass, diminished libido, erectile dysfunction, and mood changes. A diagnosis typically requires consistently low morning serum total testosterone levels, usually below 300 ng/dL, confirmed by repeat testing.
A standard protocol for male testosterone optimization often involves weekly intramuscular injections of Testosterone Cypionate (200mg/ml). This injectable form provides a stable and predictable delivery of the hormone. The goal is to restore testosterone levels to a mid-normal physiological range, typically between 400-700 ng/dL, while carefully monitoring for any adverse effects.
Alongside testosterone administration, additional medications are frequently incorporated to manage potential side effects and preserve endogenous testicular function.
- Gonadorelin ∞ Administered via subcutaneous injections, typically twice weekly, this peptide helps maintain natural testosterone production and fertility. It acts as a synthetic form of gonadotropin-releasing hormone (GnRH), stimulating the pituitary gland to release follicle-stimulating hormone (FSH) and luteinizing hormone (LH), which are crucial for testicular function.
- Anastrozole ∞ This oral tablet, often taken twice weekly, functions as an aromatase inhibitor. It blocks the conversion of testosterone into estrogen, helping to mitigate estrogen-related side effects such as gynecomastia or fluid retention.
- Enclomiphene ∞ This selective estrogen receptor modulator (SERM) may be included to support LH and FSH levels, further encouraging the body’s own testosterone production and preserving testicular size.
Regular monitoring of blood parameters, including serum testosterone, hematocrit, and prostate-specific antigen (PSA), is essential to ensure the safety and efficacy of the therapy. Adjustments to dosing are made based on these laboratory results and the patient’s symptomatic response.
Male testosterone optimization protocols aim to restore physiological levels while preserving endogenous function and mitigating side effects.
Testosterone Replacement Therapy for Women
Hormonal balance in women, particularly during peri-menopause and post-menopause, also benefits significantly from targeted interventions. Women can experience symptoms such as irregular cycles, mood fluctuations, hot flashes, and reduced libido due to declining hormonal levels. While estrogen replacement often takes precedence, optimizing testosterone levels plays a vital role in addressing symptoms like low sexual desire, fatigue, and overall well-being.
Protocols for female testosterone optimization typically involve low-dose administration to achieve physiological premenopausal ranges.
- Testosterone Cypionate ∞ A common approach involves weekly subcutaneous injections, usually 10 ∞ 20 units (0.1 ∞ 0.2ml). This low-dose method allows for precise titration and consistent delivery.
- Progesterone ∞ Prescribed based on menopausal status, progesterone is crucial for endometrial health in women with an intact uterus receiving estrogen therapy, and it also contributes to mood and sleep quality.
- Pellet Therapy ∞ Long-acting testosterone pellets, inserted subcutaneously, offer a convenient option for sustained release. Anastrozole may be co-administered when appropriate to manage estrogen conversion, similar to male protocols.
It is important to note that testosterone therapy for women is often considered “off-label” in many regions, meaning few products are specifically approved for female use. Despite this, clinical guidelines and extensive experience support its efficacy when administered by knowledgeable practitioners.
Monitoring includes baseline and periodic total testosterone levels, aiming for the upper range of normal female levels (typically 20-70 ng/dL), along with assessments of sex hormone binding globulin (SHBG) and potential side effects like increased body hair or skin changes.

Post-TRT or Fertility-Stimulating Protocol for Men
For men who have discontinued TRT or are actively trying to conceive, specific protocols aim to restore natural testicular function and spermatogenesis. Exogenous testosterone suppresses the body’s own production of LH and FSH, which are essential for sperm creation. The goal of these protocols is to reactivate the hypothalamic-pituitary-gonadal (HPG) axis.
A typical protocol includes a combination of agents ∞
- Gonadorelin ∞ This stimulates the pituitary to release LH and FSH, directly signaling the testes to resume testosterone and sperm production.
- Tamoxifen ∞ A selective estrogen receptor modulator (SERM), tamoxifen blocks estrogen receptors in the pituitary, reducing negative feedback and increasing LH and FSH secretion. It can also help prevent or treat gynecomastia.
- Clomid (Clomiphene Citrate) ∞ Another SERM, clomid works similarly to tamoxifen by blocking estrogen receptors, thereby stimulating the release of GnRH, LH, and FSH, which in turn boosts endogenous testosterone production and spermatogenesis.
- Anastrozole ∞ Optionally included, anastrozole can manage estrogen levels, particularly if they rise significantly during the recovery phase, which might otherwise inhibit the HPG axis.
Recovery of spermatogenesis can take several months, and success rates vary depending on the duration of prior TRT and individual physiological response.

Growth Hormone Peptide Therapy
Growth hormone peptide therapy represents a distinct approach to optimizing physiological function, particularly for active adults and athletes seeking benefits related to anti-aging, muscle gain, fat reduction, and sleep quality. These peptides are not synthetic growth hormone itself, but rather growth hormone secretagogues (GHSs), which stimulate the body’s own pituitary gland to produce and release more natural growth hormone.
Key peptides utilized in these protocols include ∞
| Peptide Name | Primary Mechanism of Action | Targeted Benefits |
|---|---|---|
| Sermorelin | Analog of Growth Hormone-Releasing Hormone (GHRH), stimulating pituitary GH release. | Improved body composition, sleep quality, recovery. |
| Ipamorelin / CJC-1295 | Ipamorelin is a GHRP; CJC-1295 is a GHRH analog. Often combined for synergistic GH release. | Enhanced muscle mass, fat reduction, anti-aging effects. |
| Tesamorelin | A GHRH analog, specifically targeting visceral fat reduction. | Reduction of abdominal fat, cardiovascular health support. |
| Hexarelin | A potent GHRP, stimulating GH release and potentially improving cardiac function. | Muscle growth, tissue repair, anti-inflammatory effects. |
| MK-677 (Ibutamoren) | A non-peptide GHS, orally active, stimulating GH and IGF-1. | Increased appetite, muscle gain, improved sleep, skin health. |
These peptides work by interacting with specific receptors in the pituitary gland and hypothalamus, leading to a pulsatile release of growth hormone, mimicking the body’s natural rhythm. This approach aims to restore more youthful levels of growth hormone, which naturally decline with age, without directly introducing exogenous hormone.
Growth hormone peptides stimulate the body’s own production, offering benefits for body composition, recovery, and vitality.

Other Targeted Peptides
Beyond growth hormone secretagogues, other specialized peptides address specific physiological needs, offering targeted support for various aspects of health.
- PT-141 (Bremelanotide) ∞ This peptide is specifically designed for sexual health. It acts on melanocortin receptors in the brain, particularly the melanocortin 4 receptor (MC4R), to stimulate sexual arousal and desire. Unlike traditional medications that primarily affect blood flow, PT-141 works on the central nervous system, addressing the neurological pathways involved in sexual response. It has shown promise in treating hypoactive sexual desire disorder (HSDD) in women and erectile dysfunction (ED) in men, particularly when psychological or central components are involved.
- Pentadeca Arginate (PDA) ∞ This innovative peptide is gaining recognition for its role in tissue repair, healing, and inflammation management. PDA is a synthetic peptide that supports the body’s natural healing processes, accelerating the repair of damaged tissues, tendons, and ligaments. It also exhibits potent anti-inflammatory effects, which are crucial for faster recovery from injuries and alleviating chronic discomfort. PDA is often utilized in regenerative medicine and for enhancing recovery in active individuals.
These peptides represent a frontier in personalized wellness, offering precise biological signaling to address specific concerns and optimize physiological function. Their mechanisms of action are distinct, yet they collectively contribute to the broader goal of systemic balance and enhanced well-being.


Academic
A deep understanding of hormonal balance necessitates an exploration of the intricate interplay within the endocrine system and its profound connections to other physiological networks. This academic perspective moves beyond symptomatic relief, seeking to comprehend the underlying molecular and cellular mechanisms that govern long-term health outcomes. Optimizing hormonal balance involves a sophisticated recalibration of these biological systems, influencing everything from cellular metabolism to neurocognitive function.
The endocrine system functions as a highly integrated regulatory network, where the activity of one gland or hormone profoundly influences others. This interconnectedness is exemplified by the various biological axes, such as the hypothalamic-pituitary-adrenal (HPA) axis and the hypothalamic-pituitary-thyroid (HPT) axis, which operate in concert with the HPG axis to maintain systemic homeostasis.
Dysregulation in one axis can create ripple effects throughout the entire endocrine landscape, leading to a complex array of symptoms that often defy simple categorization.

The Neuroendocrine Axis and Systemic Homeostasis
The central nervous system and the endocrine system are not merely adjacent entities; they are inextricably linked through neuroendocrine pathways. The hypothalamus, a critical brain region, serves as the primary interface, translating neural signals into hormonal responses. It synthesizes and releases neurohormones that control the pituitary gland, which in turn regulates peripheral endocrine glands. This continuous dialogue ensures that the body’s internal environment remains stable despite external stressors or internal fluctuations.
Consider the HPA axis, which governs the body’s stress response. Chronic activation of this axis, leading to sustained elevated cortisol levels, can suppress thyroid function, reduce gonadal hormone production, and impair insulin sensitivity. This demonstrates how a persistent stress response can directly contribute to broader hormonal dysregulation, impacting metabolic health, reproductive function, and overall energy balance. Understanding these cross-talk mechanisms is essential for developing comprehensive optimization strategies.
Hormonal balance is a dynamic state, influenced by intricate feedback loops and cross-system communication.
The precise mechanisms by which hormones exert their effects involve binding to specific receptors on target cells, initiating intracellular signaling cascades that alter gene expression and cellular function. For instance, steroid hormones like testosterone and estrogen, being lipid-soluble, can pass through cell membranes and bind to intracellular receptors, directly influencing DNA transcription.
Peptide hormones, conversely, typically bind to receptors on the cell surface, triggering secondary messenger systems. This molecular precision underscores the profound impact even subtle hormonal shifts can have on cellular physiology.

Metabolic Pathways and Hormonal Interplay
The relationship between hormonal balance and metabolic function is particularly critical for long-term health. Hormones are key regulators of glucose metabolism, lipid synthesis, and energy expenditure. Insulin, produced by the pancreas, is central to glucose uptake and utilization. Insulin resistance, a condition where cells become less responsive to insulin, is often linked to imbalances in other hormones, including cortisol and sex steroids.
Thyroid hormones (T3 and T4) regulate basal metabolic rate, influencing nearly every cell in the body. Suboptimal thyroid function can lead to reduced energy expenditure, weight gain, and cognitive slowing. Similarly, testosterone in men and estrogen in women play roles in maintaining lean muscle mass and healthy body fat distribution. Declining levels of these hormones can contribute to sarcopenia (muscle loss) and increased visceral adiposity, both of which are risk factors for metabolic syndrome and cardiovascular disease.
| Hormone | Primary Metabolic Role | Impact of Imbalance |
|---|---|---|
| Insulin | Glucose uptake, energy storage | Insulin resistance, type 2 diabetes, weight gain |
| Thyroid Hormones (T3/T4) | Basal metabolic rate, energy production | Fatigue, weight gain, cognitive impairment |
| Cortisol | Stress response, glucose regulation | Insulin resistance, abdominal fat accumulation, muscle breakdown |
| Testosterone | Muscle mass, fat distribution, insulin sensitivity | Sarcopenia, increased adiposity, metabolic syndrome risk |
| Estrogen | Glucose metabolism, lipid profile, bone density | Insulin resistance, dyslipidemia, bone loss |
Optimizing these hormonal interactions can lead to significant improvements in metabolic flexibility, allowing the body to efficiently switch between fuel sources and maintain stable energy levels. This metabolic resilience is a hallmark of healthy aging and a powerful defense against chronic disease.

Neurotransmitter Function and Cognitive Health
The influence of hormones extends deeply into the realm of neurotransmitter function and cognitive health. Hormones act as neuromodulators, directly affecting the synthesis, release, and receptor sensitivity of neurotransmitters in the brain. This direct interaction explains the profound impact of hormonal shifts on mood, memory, and overall brain performance.
For example, estrogen plays a significant role in maintaining synaptic plasticity and neuronal health, particularly in areas of the brain associated with memory and executive function. Declining estrogen levels during menopause can contribute to cognitive changes, including memory lapses and reduced mental clarity. Similarly, testosterone influences dopamine and serotonin pathways, affecting mood, motivation, and spatial cognition in both men and women.
Hormonal balance profoundly influences neurotransmitter activity, shaping mood, memory, and cognitive resilience.
Peptides, such as PT-141, offer a compelling example of this neuro-hormonal connection. By directly stimulating melanocortin receptors in the hypothalamus, PT-141 modulates dopamine release in brain regions associated with sexual desire. This central mechanism, distinct from peripheral vascular effects, highlights the brain’s role as the ultimate orchestrator of physiological responses, influenced by precise peptide signaling.
The intricate dance between hormones and neurotransmitters underscores the holistic nature of well-being. Addressing hormonal imbalances can therefore yield benefits that extend far beyond the endocrine system, contributing to enhanced cognitive function, emotional stability, and a sustained sense of mental sharpness throughout the lifespan. This comprehensive approach recognizes the body as an integrated system, where optimal function in one area supports resilience across all others.

References
- Guyton, Arthur C. and John E. Hall. Textbook of Medical Physiology. 13th ed. Elsevier, 2016.
- Boron, Walter F. and Emile L. Boulpaep. Medical Physiology. 3rd ed. Elsevier, 2017.
- Speroff, Leon, and Marc A. Fritz. Clinical Gynecologic Endocrinology and Infertility. 8th ed. Lippincott Williams & Wilkins, 2011.
- Bhasin, Shalender, et al. “Testosterone Therapy in Adult Men with Androgen Deficiency Syndromes ∞ An Endocrine Society Clinical Practice Guideline.” Journal of Clinical Endocrinology & Metabolism, vol. 95, no. 6, 2010, pp. 2536-2559.
- Wierman, Margaret E. et al. “Androgen Therapy in Women ∞ A Reappraisal ∞ An Endocrine Society Clinical Practice Guideline.” Journal of Clinical Endocrinology & Metabolism, vol. 99, no. 10, 2014, pp. 3489-3510.
- Vance, Mary L. and Michael O. Thorner. “Growth Hormone-Releasing Hormone (GHRH) and Growth Hormone-Releasing Peptides (GHRPs).” Endocrine Reviews, vol. 18, no. 5, 1997, pp. 605-619.
- Papadakis, Maxine A. et al. Current Medical Diagnosis & Treatment 2024. 63rd ed. McGraw Hill, 2024.
- Rosen, Raymond C. et al. “Bremelanotide for the Treatment of Hypoactive Sexual Desire Disorder in Women ∞ An Overview of Clinical Efficacy and Safety.” Sexual Medicine Reviews, vol. 7, no. 3, 2019, pp. 463-471.
- Sato, Kazuo, et al. “Pentadecapeptide BPC 157 Promotes Tendon Healing by Activating Tendon Fibroblasts and Enhancing Collagen Synthesis.” Journal of Orthopaedic Research, vol. 38, no. 1, 2020, pp. 138-147.
- Katz, Neil P. et al. “The Role of Growth Hormone in Metabolism and Body Composition.” Clinical Therapeutics, vol. 26, no. 11, 2004, pp. 1775-1785.

Reflection
As you consider the intricate biological systems discussed, pause to reflect on your own experiences. Have you recognized any of these subtle shifts in your energy, mood, or physical capacity? Understanding the language of your body, particularly its hormonal communications, represents a powerful act of self-discovery. This knowledge is not merely academic; it serves as a compass, guiding you toward a more aligned and vibrant existence.
The journey toward optimal hormonal balance is a deeply personal one, unique to your individual physiology and lived experience. It invites a proactive engagement with your health, moving beyond passive observation to active participation. This path requires a partnership with knowledgeable clinical guidance, translating complex scientific principles into actionable strategies tailored precisely for you.
Consider this exploration a foundational step. The insights gained here can serve as a catalyst for deeper inquiry into your own biological systems. Reclaiming vitality and functional capacity without compromise is a tangible aspiration, rooted in a precise understanding of your internal landscape. Your body possesses an inherent capacity for balance; the objective is to provide it with the precise support it needs to express that capacity fully.



