Fundamentals
You are here because you are contemplating a significant step toward reclaiming your vitality through testosterone therapy. You may be feeling the pervasive effects of low androgen levels ∞ the mental fog, the physical fatigue, the decline in drive ∞ and you are seeking a solution.
Yet, a critical question stands in your path, a question that speaks to the future, to legacy, and to the continuation of your own story ∞ How do you pursue this personal optimization without sacrificing your ability to have children? This is a profound and valid concern.
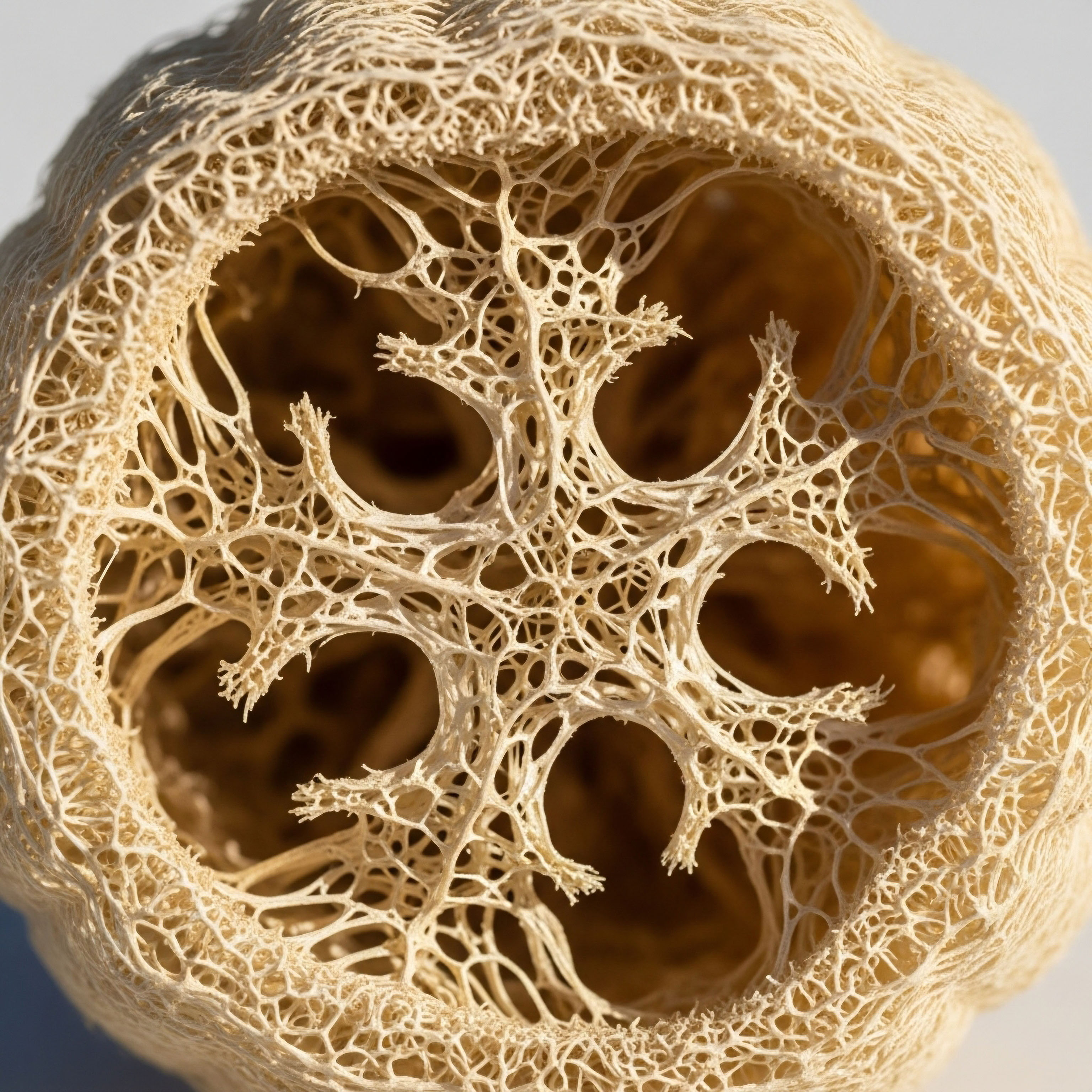
Your body’s hormonal system is a finely tuned orchestra, a complex network of communication that governs everything from your energy levels to your reproductive capacity. Introducing an external hormone, even one your body desperately needs, changes the conversation within this network.
To understand how to preserve fertility, we must first appreciate the biological dialogue that testosterone therapy interrupts. Your brain, specifically the hypothalamus and pituitary gland, is in constant communication with your testes. This is known as the Hypothalamic-Pituitary-Gonadal (HPG) axis. Think of it as a command-and-control system.
The pituitary gland, acting on instructions from the hypothalamus, sends out two key messenger hormones ∞ Luteinizing Hormone (LH) and Follicle-Stimulating Hormone (FSH). LH is the direct signal to the Leydig cells in your testes to produce testosterone. FSH is the signal to the Sertoli cells, also in the testes, to support and mature sperm production, a process called spermatogenesis. These two signals work in concert, creating the internal environment necessary for both virility and fertility.
Exogenous testosterone therapy suppresses the body’s natural signals for sperm production, creating a need for proactive fertility preservation strategies.
When you begin testosterone replacement therapy (TRT), you are introducing testosterone from an external source. Your brain, ever vigilant, detects these high levels of circulating testosterone. It concludes that the testes are overproducing and, in an effort to maintain balance, it shuts down its own signals.
It dramatically reduces the production of both LH and FSH. The command center goes quiet. Without the LH signal, your testes stop their own testosterone production. Without the FSH signal, the intricate process of spermatogenesis slows and can eventually halt completely. This is the biological root of TRT-induced infertility. The testes, deprived of their instructions, shrink and cease their dual functions of hormone and sperm production.
The methods to preserve fertility during this process are all designed to address this fundamental interruption. They are not workarounds; they are sophisticated strategies to either maintain the body’s internal signaling, provide a substitute for it, or create a definitive safeguard before the process begins.
These approaches can be understood through three distinct philosophies of intervention. The first is to provide a direct, alternative signal to the testes, keeping them active despite the silence from the brain. The second is to persuade the brain to keep sending its own natural signals, maintaining the integrity of the entire HPG axis.
The third, and most absolute, is to secure your fertility potential before altering your body’s hormonal environment. Each path offers a different set of considerations, and understanding them is the first, most empowering step in making an informed decision that aligns with both your immediate wellness goals and your long-term life plans.

The Core Challenge the HPG Axis
The relationship between your brain and your testes is a delicate feedback loop. Healthy function depends on this continuous, dynamic communication. The introduction of exogenous testosterone disrupts this loop by creating what is known as negative feedback.
The elevated hormone levels signal to the hypothalamus that no more gonadotropin-releasing hormone (GnRH) is needed, which in turn tells the pituitary to stop secreting LH and FSH. This is a natural, self-regulating mechanism designed to prevent excessive hormone production. In the context of TRT, however, it leads to the shutdown of testicular function. The core challenge, therefore, is to administer testosterone to alleviate the symptoms of hypogonadism while simultaneously preventing this negative feedback from silencing sperm production.
Successfully navigating this requires a protocol that acknowledges the complexity of the endocrine system. It requires moving beyond a simple “replacement” mindset to one of “system support.” The goal is to keep the testicular machinery running.
This involves understanding that intratesticular testosterone ∞ the concentration of testosterone inside the testes ∞ is the key driver of spermatogenesis and is normally present at levels 100 times higher than in the bloodstream. TRT alone raises blood levels but causes intratesticular levels to plummet. The best preservation methods are those that specifically maintain this high intratesticular testosterone concentration, ensuring the environment for sperm development remains viable.


Intermediate
Having grasped the foundational concept of the Hypothalamic-Pituitary-Gonadal (HPG) axis and the suppressive effect of testosterone therapy, we can now examine the specific clinical protocols designed to counteract this effect. These methods are targeted interventions, each with a unique mechanism of action aimed at preserving testicular function and, by extension, your fertility.
The choice of protocol depends on individual goals, baseline health metrics, and a collaborative discussion with your healthcare provider. The primary strategies involve either mimicking the body’s natural stimulating hormones or preventing the feedback loop that causes their suppression in the first place. A third strategy provides a definitive, non-biological assurance.

Protocol 1 Mimicking the Luteinizing Hormone Signal with hCG
One of the most established methods for preserving fertility on TRT is the concurrent use of Human Chorionic Gonadotropin (hCG). hCG is a hormone that is structurally very similar to Luteinizing Hormone (LH), the body’s primary signal for testosterone production. It works by binding to and activating the same LH receptors on the Leydig cells within the testes.
In essence, hCG acts as a direct replacement for the LH signal that is suppressed by TRT. By directly stimulating the testes, hCG accomplishes two critical objectives ∞ it maintains the production of intratesticular testosterone at the high levels necessary for spermatogenesis, and it prevents the testicular atrophy, or shrinkage, that commonly occurs with TRT alone.
A typical clinical protocol involves administering low doses of hCG via subcutaneous injection two to three times per week, alongside the standard weekly testosterone injection. For instance, a dose of 250 to 500 IU of hCG injected every other day or twice weekly is often sufficient to maintain testicular volume and sperm production in many men.
This approach allows an individual to receive the systemic benefits of optimized testosterone levels from TRT while keeping the reproductive machinery within the testes functional. It is a proactive measure to keep the local testicular environment primed for fertility.
Protocols using hCG or Gonadorelin are designed to actively maintain testicular function by providing a substitute for the body’s suppressed hormonal signals.

What Are the Clinical Considerations for Using hCG?
While effective, the use of hCG requires careful management. Because it stimulates the testes to produce testosterone, it can also increase the production of estrogen as a byproduct, through the action of the aromatase enzyme. This may necessitate the use of an aromatase inhibitor, such as Anastrozole, to manage potential estrogenic side effects like water retention or mood changes.
Monitoring of blood levels for testosterone, estradiol, LH, and FSH is essential to ensure the protocol is balanced and effective. The goal is to use the lowest effective dose of hCG to maintain testicular function without causing excessive hormonal fluctuations.
| Parameter | TRT Alone | TRT with Concurrent hCG |
|---|---|---|
| Systemic Testosterone | Optimized (normalized) | Optimized (normalized) |
| LH/FSH Production | Suppressed / Near-zero | Suppressed / Near-zero |
| Intratesticular Testosterone | Dramatically reduced | Maintained or restored |
| Spermatogenesis | Suppressed or halted | Preserved in most cases |
| Testicular Volume | Reduced (atrophy) | Maintained |
| Primary Mechanism | Exogenous hormone replacement | Exogenous T plus direct testicular stimulation |

Protocol 2 Stimulating the Pituitary with Gonadorelin
An alternative to directly stimulating the testes with an LH analog is to stimulate the pituitary gland itself. This is accomplished using Gonadorelin, a synthetic version of Gonadotropin-Releasing Hormone (GnRH). In a healthy HPG axis, the hypothalamus releases GnRH in pulses to trigger the pituitary to release LH and FSH.
By administering Gonadorelin, the protocol aims to mimic this natural trigger, prompting the pituitary to continue its function despite the negative feedback from TRT. It is an upstream intervention compared to hCG.
The use of Gonadorelin is intended to maintain the entire HPG axis in a more physiologic state. By stimulating the release of both LH and FSH, it supports both testosterone production (via LH) and the qualitative aspects of sperm maturation (via FSH). However, its effectiveness can be more complex.
The pituitary can become desensitized to a constant GnRH signal, which is why natural GnRH is pulsatile. Therefore, the dosing strategy for Gonadorelin is critical. While some protocols use small, frequent subcutaneous injections to mimic this pulse, its practical application and efficacy compared to hCG are subjects of ongoing clinical discussion. Some clinicians find hCG to be a more robust and reliable agent for maintaining testicular function during TRT due to its direct action on the testes.

Protocol 3 Maintaining the HPG Axis with SERMs
A third approach involves using a class of compounds known as Selective Estrogen Receptor Modulators (SERMs), with Enclomiphene citrate being a prominent example. This method works on a different principle. Instead of adding a stimulating hormone, Enclomiphene blocks estrogen receptors in the brain.
Estrogen is part of the negative feedback loop; when the brain detects estrogen, it suppresses GnRH production. By blocking these receptors, Enclomiphene essentially tricks the brain into thinking estrogen levels are low. In response, the hypothalamus increases GnRH production, which in turn stimulates the pituitary to produce more LH and FSH.
This stimulation of the body’s own endocrine pathways makes Enclomiphene a powerful tool. It can raise testosterone levels on its own, sometimes being used as a standalone alternative to TRT for men with secondary hypogonadism who wish to preserve fertility. It can also be used in conjunction with TRT.
In such a protocol, Enclomiphene works to counteract the suppressive effects of exogenous testosterone at the source, compelling the brain to keep the LH and FSH signals active. This preserves the entire HPG axis, maintains testicular function, and supports spermatogenesis.
- hCG ∞ Acts as an LH substitute, directly stimulating the testes. This is a downstream, direct-acting approach.
- Gonadorelin ∞ Acts as a GnRH substitute, stimulating the pituitary. This is an upstream approach designed to maintain more of the natural hormonal cascade.
- Enclomiphene ∞ Blocks estrogen feedback to the brain, causing an increase in the body’s own production of GnRH, LH, and FSH. This approach works at the very top of the signaling cascade.

Protocol 4 the Ultimate Insurance Policy of Cryopreservation
The only method that guarantees the preservation of your fertility potential with 100% certainty is sperm cryopreservation, commonly known as sperm banking. This process involves collecting, analyzing, freezing, and storing semen samples before you begin testosterone therapy. It is the most definitive and foolproof strategy because it creates a backup of your genetic material that is completely independent of your future hormonal status.
Regardless of how your body responds to TRT or adjunctive therapies, your stored samples remain viable for future use in assisted reproductive technologies like in vitro fertilization (IVF) or intrauterine insemination (IUI).
The process is straightforward:
- Consultation and Screening ∞ You will consult with a fertility clinic or cryobank and undergo infectious disease screening.
- Sample Collection ∞ You will provide one or more semen samples. It is often recommended to store multiple vials from several collections to ensure an adequate supply for future use.
- Semen Analysis ∞ Each sample is analyzed in a laboratory to assess sperm count, motility (movement), and morphology (shape). This confirms the viability of the sample for freezing.
- Cryopreservation ∞ A cryoprotectant agent is added to the sperm to protect the cells during the freezing process. The samples are then cooled and stored in liquid nitrogen at -196°C.
- Long-Term Storage ∞ The frozen samples can be stored indefinitely without degradation in quality.
For any man for whom future biological fatherhood is a priority, cryopreservation should be strongly considered as the first step before initiating TRT. The other protocols are highly effective for many, but individual responses can vary. Sperm banking provides complete peace of mind.


Academic
A sophisticated understanding of fertility preservation during testosterone therapy requires a systems-biology perspective of the Hypothalamic-Pituitary-Gonadal (HPG) axis. This regulatory network is not a simple linear pathway but a complex interplay of feedback loops, pulsatile signaling, and paracrine communication within the testicular microenvironment.
Exogenous testosterone administration acts as a powerful external input that disrupts the homeostatic equilibrium of this network, primarily through potent negative feedback at the hypothalamic and pituitary levels. The resulting suppression of gonadotropin secretion leads to a state of hypogonadotropic hypogonadism, which is the direct cause of impaired spermatogenesis.
The academic approach to fertility preservation, therefore, is centered on targeted pharmacological manipulations of this network to maintain the critical elements required for sperm production, most notably, high levels of intratesticular testosterone (ITT).

The Central Role of Intratesticular Testosterone
Spermatogenesis is an androgen-dependent process that is critically reliant on a very high concentration of testosterone within the seminiferous tubules of the testes. Research has established that ITT levels in eugonadal men are approximately 50 to 100 times higher than circulating serum testosterone levels.
Standard TRT protocols, while normalizing serum testosterone, fail to replicate this high ITT environment. In fact, by suppressing endogenous LH secretion, TRT causes a profound drop in ITT, leading to the cessation of spermatogenesis. Therefore, the primary objective of any fertility-preserving adjunct therapy is the maintenance of supraphysiologic ITT. This principle forms the basis for evaluating the efficacy of different pharmacological interventions.
The maintenance of this ITT concentration is primarily the function of the Leydig cells, which are stimulated by LH. The resulting testosterone diffuses into the adjacent seminiferous tubules, where it acts on the Sertoli cells. Sertoli cells, often called the “nurse cells” of the testes, are essential for providing the structural and nutritional support for developing germ cells.
They are responsive to both FSH and testosterone, and their proper function is indispensable for the successful progression of spermatogonia to mature spermatozoa. While FSH is important for initiating spermatogenesis and determining the total output of sperm, high ITT is essential for the completion of meiosis and the maturation of spermatids. Thus, an effective protocol must ensure the continued stimulation of this local, high-androgen environment.

How Do Different Protocols Modulate the HPG Network?
The primary pharmacological agents used for fertility preservation ∞ hCG, Gonadorelin, and SERMs like Enclomiphene ∞ each interact with the HPG axis at different nodes. Their efficacy can be analyzed based on their ability to restore the necessary signaling for ITT production and spermatid maturation.
Human Chorionic Gonadotropin (hCG) ∞ As an LH analog, hCG bypasses the suppressed hypothalamic and pituitary components of the axis and acts directly on the LH receptor (LHCGR) on Leydig cells. This initiates the steroidogenic cascade, leading to the production of testosterone and the restoration of ITT.
Studies have demonstrated that low-dose hCG (e.g. 500 IU every other day) co-administered with TRT can successfully maintain ITT levels and preserve spermatogenesis in the majority of men. A study demonstrated that co-administration of low-dose hCG with TRT maintained ITT and preserved spermatogenesis at one year of follow-up. This direct, downstream intervention is robust and reliable, as it does not depend on the responsiveness of the suppressed pituitary gland.
Gonadorelin ∞ As a GnRH analog, Gonadorelin targets the GnRH receptor on pituitary gonadotrophs. Its intended action is to stimulate the endogenous secretion of both LH and FSH. Theoretically, this is a more physiologic approach as it preserves the production of both gonadotropins. However, the pharmacology is complex.
The GnRH receptor is known to downregulate in response to continuous stimulation, which is why endogenous GnRH is released in a highly regulated, pulsatile fashion. Continuous administration of a GnRH agonist can lead to a paradoxical suppression of gonadotropin release.
While some protocols attempt to use low, frequent doses of Gonadorelin to mimic pulsatility, the clinical evidence supporting its superiority or even equivalence to hCG in the context of concurrent TRT is less extensive. Some clinical experience suggests hCG is more effective at reversing testicular atrophy and maintaining fertility markers.
Enclomiphene Citrate ∞ This SERM acts at the apex of the axis. It functions as an antagonist at the estrogen receptor-alpha (ERα) in the hypothalamus. Estrogen is a key mediator of negative feedback on GnRH secretion. By blocking this feedback, enclomiphene leads to an increase in GnRH pulse frequency and amplitude, resulting in elevated serum LH and FSH.
Studies have shown that enclomiphene can effectively raise serum testosterone into the normal range while preserving or even improving semen parameters. Its utility as an adjunct to TRT is based on its potential to “override” the negative feedback from exogenous testosterone, thereby maintaining endogenous gonadotropin support to the testes. It represents a strategy of preserving the entire native signaling pathway.
The choice between hCG, Enclomiphene, or Gonadorelin hinges on a clinical decision of whether to bypass, stimulate, or unblock the native hormonal axis.
| Agent | Mechanism of Action | Target Receptor/Tissue | Effect on HPG Axis | Effect on ITT | Clinical Considerations |
|---|---|---|---|---|---|
| hCG | LH analog; directly stimulates Leydig cells. | LH Receptor (Testes) | Bypasses hypothalamus/pituitary; maintains testicular stimulation. | Directly increases ITT. | Robust and well-studied. May increase estradiol, requiring monitoring. |
| Gonadorelin | GnRH analog; stimulates pituitary gonadotrophs. | GnRH Receptor (Pituitary) | Stimulates endogenous LH/FSH release. | Indirectly increases ITT via LH stimulation. | Efficacy depends on dosing protocol to avoid receptor desensitization. Less clinical data than hCG. |
| Enclomiphene | Estrogen receptor antagonist at the hypothalamus. | Estrogen Receptor (Hypothalamus) | Blocks negative feedback, increasing endogenous GnRH, LH, and FSH. | Indirectly increases ITT via endogenous LH. | Can be used as monotherapy or adjunct. Preserves the entire axis. |
| Cryopreservation | Physical preservation of gametes. | N/A (Laboratory Procedure) | Independent of the HPG axis. | N/A | The only definitive guarantee. Recommended as a primary step before initiating therapy. |

Post-TRT Fertility Recovery Protocols
For individuals who did not use concurrent fertility-preserving therapies and wish to restore spermatogenesis after ceasing TRT, specific protocols are employed. The timeline for recovery can be prolonged, sometimes taking months or even years. The goal of these protocols is to vigorously stimulate the HKG axis to restart endogenous function.
A common approach involves discontinuing exogenous testosterone and initiating a combination therapy. This often includes high-dose hCG (e.g. 3000 IU every other day) to directly stimulate the testes, combined with a SERM like Clomiphene or Tamoxifen to block estrogenic feedback and stimulate pituitary output of LH and FSH.
In cases where FSH levels remain suppressed, recombinant FSH (Gonal-f) may be added to the regimen. These aggressive restart protocols highlight the profound suppression that can occur and underscore the value of proactive, concurrent preservation methods from the outset.

References
- Wenker, E. P. et al. “The Use of HCG-Based Combination Therapy for Recovery of Spermatogenesis after Testosterone Use.” Journal of Sexual Medicine, vol. 12, no. 6, 2015, pp. 1334-1340.
- Kim, E. D. et al. “Enclomiphene Citrate for the Treatment of Secondary Male Hypogonadism.” Expert Opinion on Investigational Drugs, vol. 23, no. 11, 2014, pp. 1563-1569.
- Hsieh, T. C. et al. “Concomitant Human Chorionic Gonadotropin Preserves Spermatogenesis in Men Undergoing Testosterone Replacement Therapy.” The Journal of Urology, vol. 189, no. 2, 2013, pp. 647-650.
- Ramasamy, R. et al. “Preserving fertility in the hypogonadal patient ∞ an update.” Translational Andrology and Urology, vol. 4, no. 2, 2015, pp. 125-130.
- Wheeler, K. M. et al. “A review of the clinical efficacy and safety of enclomiphene citrate.” Translational Andrology and Urology, vol. 8, no. 4, 2019, pp. 385-393.
- Brito, L. F. C. et al. “The role of intratesticular testosterone in spermatogenesis.” Animal Reproduction, vol. 9, no. 1, 2012, pp. 50-59.
- Rastrelli, G. et al. “Testosterone replacement therapy and fertility.” Current Opinion in Endocrinology, Diabetes and Obesity, vol. 26, no. 3, 2019, pp. 166-174.

Reflection

Charting Your Personal Health Trajectory
You have now journeyed through the biological landscape of your endocrine system, from the command center in your brain to the intricate cellular machinery within your testes. You have seen how the introduction of testosterone, while beneficial for systemic vitality, alters a fundamental biological conversation.
The knowledge of hCG, Gonadorelin, Enclomiphene, and cryopreservation provides you with a map of the available strategies to navigate this change. Each protocol is a tool, a way to consciously guide your physiology toward a desired outcome that includes both present well-being and future potential.
This information is the essential first step. Your own health story, however, is unique. It is written in your specific biology, your baseline lab values, your personal and family goals, and your lived experience. The path forward is one of collaboration ∞ a partnership between your growing understanding of your own body and the guidance of a clinician who sees you as a whole person.
The data and the science are the foundation, but the application is personal. Consider what vitality means to you, what your vision for the future holds, and how these powerful tools can be tailored to build that reality, without compromise.