

Fundamentals
You feel it before you can name it. A subtle shift in energy, a change in the way your body responds to exercise, a fog that clouds your thinking. These experiences are valid and tangible. They are the first signals from your body’s intricate communication network, the endocrine system, that its operational parameters are changing.
The question of whether hormonal optimization is a part of a modern longevity strategy begins here, with the lived reality of your own biology. It is an inquiry into restoring function, not just masking symptoms. It is about understanding the internal language of your body to reclaim a state of high performance and vitality.
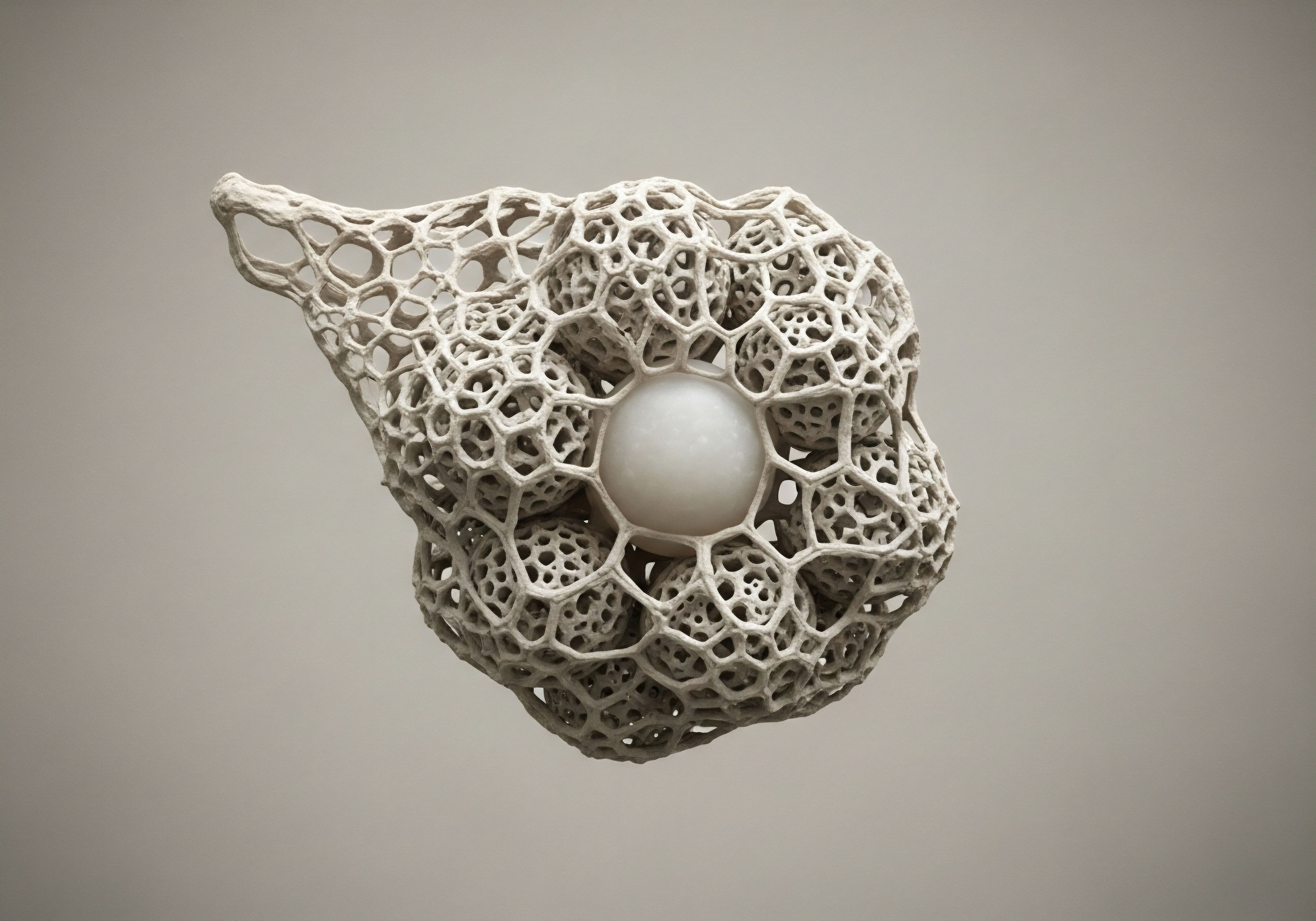
The human body operates as a meticulously integrated system, orchestrated largely by hormones. These chemical messengers, produced by endocrine glands, travel through the bloodstream to tissues and organs, dictating everything from your metabolic rate and mood to your immune response and capacity for repair. When you are young, this hormonal symphony is robust and resilient.
As you age, the production of key hormones like testosterone, estrogen, progesterone, and growth hormone naturally declines. This decline is a primary driver of the aging process itself. The fatigue, weight gain, cognitive slowdown, and loss of libido you may experience are direct physiological consequences of this diminished signaling.
Hormonal decline is a systemic degradation of the body’s internal communication network, directly impacting physical and cognitive function.
Viewing these changes through a clinical lens provides a powerful framework for action. Your symptoms are data points, reflecting a deeper shift in your body’s systemic balance. A longevity-focused approach seeks to understand this data and intervene intelligently. It involves moving beyond a passive acceptance of age-related decline and toward a proactive recalibration of your internal environment.
Hormonal support protocols are a direct method for addressing the root biochemical changes that define so much of the aging experience. They represent a way to work with your body’s own systems to maintain function and extend your healthspan, the period of life spent in good health.

The Language of Hormones
To appreciate the role of hormonal therapies, one must first understand the language these molecules speak. Hormones operate through feedback loops, elegant circuits of cause and effect that maintain homeostasis, or a stable internal state. The Hypothalamic-Pituitary-Gonadal (HPG) axis, for instance, is the central command line for reproductive and metabolic health in both men and women.
The hypothalamus releases Gonadotropin-Releasing Hormone (GnRH), which signals the pituitary gland to release Luteinizing Hormone (LH) and Follicle-Stimulating Hormone (FSH). These hormones, in turn, signal the gonads (testes or ovaries) to produce testosterone or estrogen.
With age, the sensitivity and output of this entire axis diminish. The signals become weaker, and the end-organ response fades. The result is a system-wide deficit that manifests as the symptoms of andropause in men and perimenopause or menopause in women. Addressing this deficit requires a nuanced understanding of the entire feedback loop. It is about restoring the signals, supporting the glands, and ensuring the target tissues can once again receive the messages they need to function optimally.

What Is the True Goal of Hormonal Optimization?
The objective of a modern hormonal protocol is physiological restoration. The goal is to return circulating hormone levels to a range associated with youthful vitality and optimal function. This is achieved through careful, data-driven administration of bioidentical hormones, which are molecules that are structurally identical to those produced by the human body. By replenishing these depleted signaling molecules, we can directly counteract the metabolic slowdown, cognitive decline, and physical frailty that accompany aging.
This approach is fundamentally preventative. Maintaining optimal hormonal levels helps preserve bone density, protect cardiovascular health, sustain lean muscle mass, and support cognitive function. It is a cornerstone of a medical strategy that aims to compress morbidity, meaning to shorten the period of illness and disability at the end of life. By addressing one of the core biological mechanisms of aging, we can extend the years of high-quality, functional living.


Intermediate
Advancing from the foundational understanding of hormonal decline, the next step involves examining the specific clinical protocols designed to counteract it. These are not one-size-fits-all solutions; they are highly personalized interventions based on comprehensive lab work, individual symptoms, and specific health goals.
The central principle is biochemical recalibration, using precise tools to restore the body’s endocrine system to a more youthful and functional state. This section details the mechanics and rationale behind the primary therapeutic modalities used in modern longevity medicine for both men and women.
Male Hormone Optimization Protocols
For men, age-related hormonal decline, often termed andropause or hypogonadism, primarily involves a drop in testosterone production. This leads to symptoms like fatigue, decreased muscle mass, increased body fat, low libido, and cognitive fog. A comprehensive treatment protocol addresses the entire Hypothalamic-Pituitary-Gonadal (HPG) axis.

Testosterone Replacement Therapy (TRT) for Men
The core of male hormone optimization is restoring testosterone to a healthy physiological range. This has demonstrable effects on body composition, energy levels, and mood. A standard, effective protocol involves several components working in concert.
- Testosterone Cypionate ∞ This is a bioidentical, injectable form of testosterone that provides a stable and predictable release into the bloodstream. A typical protocol involves weekly intramuscular injections (e.g. 200mg/ml) to maintain consistent levels, avoiding the peaks and troughs associated with other delivery methods.
- Gonadorelin ∞ When exogenous testosterone is introduced, the body’s natural production via the HPG axis can shut down. Gonadorelin, a synthetic analog of GnRH, is used to stimulate the pituitary gland, preserving testicular function and maintaining fertility. It is typically administered via subcutaneous injection twice a week.
- Anastrozole ∞ Testosterone can be converted into estrogen through a process called aromatization. In men, elevated estrogen can lead to side effects like water retention and gynecomastia (breast tissue development). Anastrozole is an aromatase inhibitor, an oral medication taken to block this conversion and maintain a proper testosterone-to-estrogen ratio.
- Enclomiphene ∞ This medication may be included to directly stimulate the pituitary to produce more LH and FSH, further supporting the body’s endogenous testosterone production pathways.
A well-designed TRT protocol for men does more than just replace testosterone; it manages the entire hormonal axis to maximize benefits and minimize side effects.

Female Hormone Balance Protocols
For women, the hormonal landscape is defined by the complex interplay of estrogen, progesterone, and testosterone. The transition through perimenopause and into post-menopause involves significant fluctuations and eventual decline in all three, leading to a wide array of symptoms. Therapeutic protocols are designed to restore this delicate balance.

Hormone Therapy for Women
The approach for women is highly individualized based on their menopausal status and specific symptoms, which can range from hot flashes and mood swings to low libido and cognitive changes.
- Testosterone Cypionate ∞ While often considered a male hormone, testosterone is vital for female health, contributing to libido, energy, mood, and muscle tone. Women are prescribed much lower doses than men, typically 10 ∞ 20 units (0.1 ∞ 0.2ml) weekly via subcutaneous injection, to restore levels to an optimal physiological range.
- Progesterone ∞ For women who still have a uterus, estrogen therapy must be balanced with progesterone to protect the uterine lining (endometrium) from abnormal growth. Progesterone also has its own benefits, including promoting sleep and reducing anxiety. It is prescribed based on whether a woman is still cycling or is fully post-menopausal.
- Pellet Therapy ∞ This method involves implanting small, long-acting pellets of testosterone (and sometimes estradiol) under the skin. These pellets release a steady dose of hormones over several months, offering a convenient alternative to injections. Anastrozole may be used concurrently if estrogen conversion is a concern.
Clinical studies have shown that the timing of initiating hormone therapy is a significant factor in its risk-benefit profile. The Danish Osteoporosis Study, for instance, found that women who began hormone therapy early in menopause experienced a reduction in cardiovascular disease and all-cause mortality over a 16-year period.
Conversely, the Women’s Health Initiative (WHI) trial, which involved older women who were many years past menopause, showed different outcomes, highlighting that starting therapy later may not confer the same protective benefits.

Growth Hormone and Peptide Therapies
Beyond sex hormones, another critical component of the age-related endocrine decline is the reduction in Growth Hormone (GH). GH is essential for cellular repair, metabolism, muscle maintenance, and sleep quality. Direct replacement with recombinant Human Growth Hormone (rhGH) can be effective but carries risks and can disrupt the body’s natural feedback loops. Peptide therapy offers a more nuanced approach.

How Do Growth Hormone Peptides Work?
Peptides are short chains of amino acids that act as signaling molecules. Certain peptides, known as secretagogues, stimulate the pituitary gland to produce and release its own growth hormone. This method works with the body’s natural pulsatile release of GH, which is considered a safer and more physiologic approach than direct rhGH injections.
This table outlines some of the key peptides used in longevity medicine:
| Peptide | Mechanism of Action | Primary Benefits |
|---|---|---|
| Sermorelin | A GHRH analog that directly stimulates the pituitary gland to produce GH. | Improved sleep quality, increased energy, enhanced recovery, reduced body fat. |
| Ipamorelin / CJC-1295 | A combination where CJC-1295 provides a steady elevation of GH levels and Ipamorelin mimics the natural pulse, creating a powerful synergistic effect. | Significant increase in lean muscle mass, fat loss, improved skin elasticity, enhanced bone density. |
| Tesamorelin | A potent GHRH analog particularly effective at reducing visceral adipose tissue (deep abdominal fat). | Targeted fat loss, improved cognitive function, metabolic optimization. |


Academic
A sophisticated analysis of hormonal optimization as a longevity strategy requires moving beyond symptom management and into the cellular and molecular mechanisms of aging itself. The endocrine system’s decline is deeply interwoven with a fundamental process known as cellular senescence. Understanding this connection provides a compelling, evidence-based rationale for viewing hormonal recalibration as a direct intervention against one of the primary drivers of age-related disease and functional decline.

Hormonal Decline and the Acceleration of Cellular Senescence
Cellular senescence is a state of stable cell cycle arrest triggered by various stressors, including telomere shortening, DNA damage, and oncogenic activation. Senescent cells are not inert; they accumulate in tissues with age and actively degrade their microenvironment through a complex secretome known as the Senescence-Associated Secretory Phenotype (SASP).
The SASP is a cocktail of pro-inflammatory cytokines, chemokines, and matrix-degrading enzymes that promotes chronic, low-grade inflammation (inflammaging), impairs stem cell function, and can even induce senescence in neighboring healthy cells. This process is a direct contributor to the functional decline of organs and the onset of age-related pathologies.
The endocrine system acts as a key regulator of this process. Hormones like estrogen, testosterone, and growth hormone exert protective, anti-inflammatory, and regenerative effects at the cellular level. Their decline with age removes a critical layer of defense, effectively accelerating the accumulation of senescent cells.
For example, estrogen is known to have a role in regulating mitochondrial function and protecting against oxidative stress, a primary trigger for senescence. Its absence during menopause is linked to increased markers of inflammation and cellular stress, contributing to the heightened risk of diseases like osteoporosis and cardiovascular disease.
Similarly, testosterone supports the maintenance of muscle stem cells (satellite cells), and its decline contributes to sarcopenia, the age-related loss of muscle mass, a process exacerbated by the accumulation of senescent cells in muscle tissue.
The withdrawal of key hormones creates a cellular environment permissive to the accumulation of senescent cells, thereby driving the systemic aging process.

The Interplay between the HPA Axis and the SASP
The Hypothalamic-Pituitary-Adrenal (HPA) axis, the body’s central stress response system, is also deeply connected to senescence. Chronic activation of the HPA axis, a common feature of aging, leads to elevated cortisol levels.
While acutely necessary, chronically high cortisol has catabolic (tissue breakdown) effects and can suppress immune function, including the efficient clearance of senescent cells by immune cells like natural killer (NK) cells and macrophages. The SASP itself, being highly pro-inflammatory, acts as a chronic stressor that further activates the HPA axis, creating a detrimental feedback loop. A dysregulated HPA axis and a high senescent cell burden become mutually reinforcing drivers of systemic aging.
Hormonal optimization can help break this cycle. Restoring testosterone and estrogen can mitigate the central nervous system excitability that contributes to HPA axis dysregulation. Furthermore, growth hormone secretagogues like Ipamorelin and CJC-1295 have been shown to improve sleep quality, a critical factor for resetting HPA axis function and promoting cellular repair processes that counteract senescence.

Can Hormonal Therapy Directly Modulate Senescence Pathways?
The molecular pathways that govern senescence, primarily the p53/p21 and p16INK4a/Rb pathways, are influenced by the cellular environment. Hormonal signals can modulate the expression and activity of these key proteins. Research suggests that sex hormones can influence the expression of p16INK4a, a key biomarker of cellular senescence.
By restoring these hormonal signals, it is plausible that we can delay the activation of these senescence pathways in certain cell populations, effectively slowing the rate at which tissues accumulate senescent cells.
This table compares the cellular effects of a youthful hormonal environment with those of a deficient one, in the context of senescence.
| Cellular Process | Optimal Hormonal Environment | Deficient Hormonal Environment (Aging) |
|---|---|---|
| Mitochondrial Function | Supported by estrogen and testosterone, leading to efficient energy production and low oxidative stress. | Impaired function, increased reactive oxygen species (ROS) production, a key trigger for senescence. |
| Inflammation Control | Hormones exert anti-inflammatory effects, suppressing pathways like NF-κB. | Loss of suppression leads to chronic inflammation, which promotes SASP and HPA axis activation. |
| Stem Cell Maintenance | GH and testosterone support the proliferation and differentiation of progenitor cells for tissue repair. | Reduced regenerative capacity, stem cell exhaustion, and senescence of progenitor cells. |
| SASP Regulation | Immune surveillance, aided by a healthy endocrine system, efficiently clears senescent cells. | Impaired clearance allows senescent cells and their SASP to accumulate, degrading tissue function. |
Therefore, a clinical strategy that includes hormonal optimization is a direct intervention into the molecular biology of aging. It is a method for modifying the cellular environment to be less conducive to the accumulation of senescent cells. This approach aligns with other emerging longevity therapies, such as senolytics (drugs that selectively clear senescent cells), and suggests that a combination of these strategies may offer the most powerful defense against age-related functional decline.

References
- Hodis, Howard N. and Wendy J. Mack. “Menopausal Hormone Replacement Therapy and Reduction of All-Cause Mortality and Cardiovascular Disease ∞ It’s About Time and Timing.” Cancer Journal, vol. 20, no. 5, 2014, pp. 350-59.
- Yeo, Eun-Jin, et al. “Lifelong Increased Free Testosterone and Its Effect on Health and Disease Using Mendelian Randomization.” eLife, vol. 9, 2020, e58914.
- Moreno, Anna Camille. “Balancing the Benefits and Risks of Menopausal Hormone Therapy.” Duke Health, 2020.
- Walker, Richard F. “Sermorelin ∞ A better approach to management of adult-onset growth hormone insufficiency?” Clinical Interventions in Aging, vol. 1, no. 4, 2006, pp. 307-308.
- Nehme, Jamil, et al. “Molecular mechanisms of cellular senescence.” Journal of Cell Biology, vol. 219, no. 5, 2020.
- López-Otín, Carlos, et al. “The Hallmarks of Aging.” Cell, vol. 153, no. 6, 2013, pp. 1194-1217.
- Manson, JoAnn E. et al. “Menopausal Hormone Therapy and Long-term All-Cause and Cause-Specific Mortality ∞ The Women’s Health Initiative Randomized Trials.” JAMA, vol. 318, no. 10, 2017, pp. 927-938.
- Bhasin, Shalender, et al. “Testosterone Therapy in Men With Hypogonadism ∞ An Endocrine Society Clinical Practice Guideline.” The Journal of Clinical Endocrinology & Metabolism, vol. 103, no. 5, 2018, pp. 1715-1744.
- Di Micco, Raffaella, et al. “Cellular senescence in ageing ∞ from mechanisms to therapeutic opportunities.” Nature Reviews Molecular Cell Biology, vol. 22, no. 2, 2021, pp. 75-95.

Reflection
The information presented here offers a clinical and biological framework for understanding your body’s internal systems. The knowledge that your subjective feelings of vitality are tied to objective, measurable biochemical processes is a powerful realization. It shifts the perspective from one of passive aging to one of active, informed self-stewardship.
The science provides the map, but you are the one navigating the territory of your own health. How does this understanding of your body as a system of interconnected signals change the way you view your own wellness journey? What does operating at your full potential, with all your internal communication channels clear and strong, look like for you?
This journey is deeply personal, and the decision to act upon this knowledge is the first step toward a future of sustained vitality.



