

Fundamentals
The experience of feeling disconnected from your own body is a deeply personal and often disquieting one. It can manifest as a persistent fog clouding your thoughts, an unexplainable fatigue that settles deep within your bones, or a subtle shift in mood that colors your entire perception of the world.
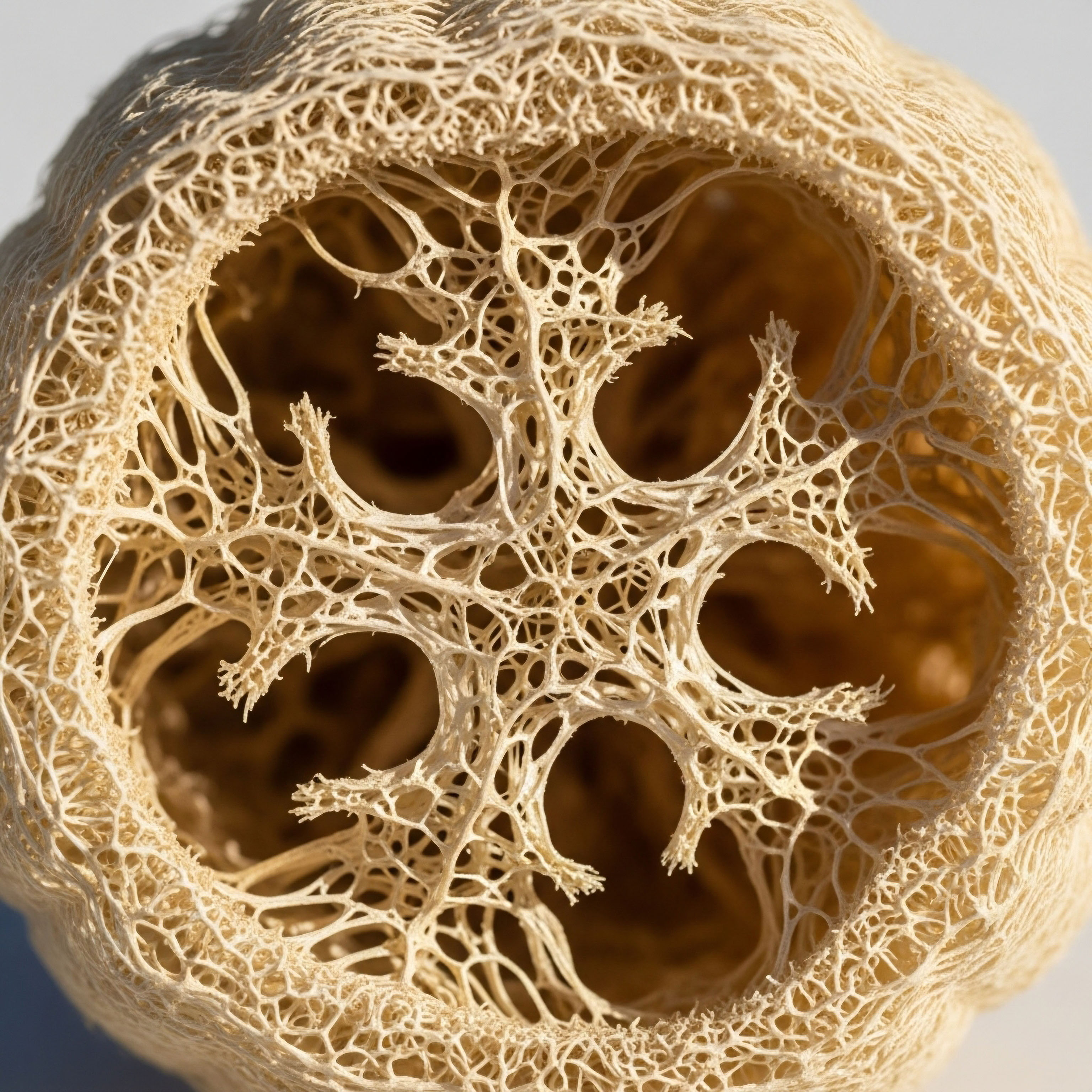
These feelings are valid, and they frequently originate from the silent, intricate dialogue happening within your endocrine system. This system is your body’s internal communication network, a collection of glands that produce and secrete hormones. These chemical messengers travel through your bloodstream, carrying precise instructions that regulate everything from your metabolism and sleep cycles to your stress response and reproductive health. Understanding this network is the first step toward reclaiming your vitality.
Your body functions as a cohesive whole, where each system is in constant communication with the others. The endocrine system is a primary conductor of this biological orchestra. When one hormonal pathway is altered, it creates a ripple effect that can influence numerous other functions.
For instance, the thyroid gland, which sets the pace of your metabolism, is in constant dialogue with the pituitary gland in your brain, which in turn communicates with your adrenal glands, the architects of your stress response. This is a system built on feedback loops, much like a thermostat in a home that constantly samples the temperature to maintain a stable environment.
When these feedback loops are disrupted, whether by age, environmental factors, or stress, the entire internal ecosystem can be affected, leading to the symptoms you may be experiencing.
Compounding addresses the interconnectedness of endocrine systems by creating patient-specific formulations that provide precise, multi-faceted support to restore hormonal equilibrium.

The Concept of Hormonal Interplay
To truly grasp how compounding can be a powerful tool, we must first appreciate the concept of hormonal interplay. Hormones do not operate in isolation. They exist in a dynamic, interconnected web. The relationship between cortisol (a primary stress hormone) and insulin (the key regulator of blood sugar) is a foundational example.
Chronic stress elevates cortisol, which can signal the body to release more glucose into the bloodstream. This, in turn, requires the pancreas to produce more insulin to manage the sugar, potentially leading to insulin resistance over time. This single interaction demonstrates how the stress response system (the hypothalamic-pituitary-adrenal or HPA axis) directly impacts the metabolic system.
Similarly, the sex hormones ∞ testosterone and estrogen ∞ have profound effects that extend far beyond reproduction. They influence bone density, cognitive function, mood, and cardiovascular health. These hormones are regulated by another critical feedback loop known as the hypothalamic-pituitary-gonadal (HPG) axis.
A disruption in this axis, common during andropause in men or perimenopause in women, affects not only sexual health but can also impact energy levels, muscle mass, and emotional well-being. The body’s major hormonal axes are constantly cross-referencing one another. A change in one requires an adaptation in the others. This is why a single-hormone approach to therapy can sometimes fall short; it may address one symptom while inadvertently creating an imbalance elsewhere in the system.

What Is Pharmaceutical Compounding
Pharmaceutical compounding is the art and science of creating personalized medications for individual patients. A compounding pharmacist combines, mixes, or alters ingredients to create a medication tailored to the unique needs of an individual, based on a prescription from a healthcare practitioner. This practice allows for a level of customization that is unavailable with mass-produced pharmaceuticals.
For hormonal health, this customization is particularly valuable. Commercially available hormone products come in a limited range of standard doses and delivery forms. Compounding, on the other hand, can provide:
- Customized Dosages ∞ Hormonal needs are highly individual. Compounding allows for the creation of medications in the precise strength required by the patient, which can be adjusted over time as their needs change.
- Unique Delivery Forms ∞ Some individuals may have difficulty with certain delivery methods, such as injections or pills. Compounding pharmacists can prepare medications in various forms, including topical creams, gels, sublingual troches, or capsules, to improve patient adherence and comfort.
- Combined Formulations ∞ To address the interconnectedness of the endocrine system, a practitioner may prescribe a formula that combines multiple hormones or supportive nutrients in a single application. This can simplify a treatment regimen and ensure the hormones are delivered in a balanced ratio.
- Allergen-Free Preparations ∞ Patients may have sensitivities or allergies to dyes, preservatives, or fillers used in commercial products. Compounding can create formulations that are free of these specific ingredients.
This level of personalization is the core principle behind using compounding to address endocrine health. It acknowledges that each person’s biochemistry is unique and that effective therapy requires a nuanced approach that respects the body’s intricate hormonal architecture. It shifts the focus from a one-size-fits-all model to a patient-centric one, where the treatment is designed to fit the individual, not the other way around.


Intermediate
As we move beyond the foundational understanding of the endocrine system, we can begin to appreciate the clinical application of compounding in restoring hormonal balance. The intermediate perspective requires us to look at the specific protocols and the biological rationale behind them.
When a clinician designs a hormonal optimization protocol, they are thinking like a systems engineer, considering the upstream and downstream effects of each intervention. The goal is to gently guide the body’s feedback loops back into a state of optimal function. Compounding becomes the precision toolkit that allows for this level of detailed intervention, providing the exact molecules in the exact doses and combinations needed to recalibrate the system without overwhelming it.
The human body’s endocrine network is a system of exquisite sensitivity. The hypothalamic-pituitary-gonadal (HPG) axis, for example, operates on a pulsatile release of hormones, with signaling molecules being secreted in carefully timed bursts. A therapeutic intervention must respect this natural rhythm.
This is where the limitations of standard pharmaceuticals can become apparent, and the advantages of a compounded approach come into focus. By being able to fine-tune dosages and combine synergistic agents, a clinician can more closely mimic the body’s natural hormonal symphony, addressing deficiencies while supporting the integrity of the entire system.

Male Hormone Optimization a Systems Approach
When a man experiences symptoms of low testosterone, such as fatigue, reduced libido, and loss of muscle mass, it is often a sign of dysregulation within the HPG axis. A comprehensive treatment protocol aims to restore testosterone levels while simultaneously managing the downstream consequences and preserving the body’s natural hormonal machinery. A standard protocol for men often involves more than just testosterone alone, illustrating the systems-based approach.

The Core Components of Male TRT
A typical, well-structured Testosterone Replacement Therapy (TRT) protocol for men integrates several components, each with a specific role in maintaining systemic balance. This multi-faceted approach is where compounding often plays a key part, allowing for the creation of specific dosages and combinations tailored to the individual’s lab results and clinical response.
- Testosterone Cypionate ∞ This is a bioidentical form of testosterone, the primary male androgen. It is typically administered via intramuscular or subcutaneous injection. The dose is carefully calculated based on baseline testosterone levels, body mass, and treatment goals. Compounding pharmacies can prepare this in specific concentrations, often in carrier oils like grapeseed oil to minimize irritation.
- Gonadorelin ∞ When exogenous testosterone is introduced, the body’s natural feedback loop can signal the pituitary to reduce its production of Luteinizing Hormone (LH). This can lead to a decrease in the body’s own testosterone production and testicular atrophy. Gonadorelin is a peptide that mimics Gonadotropin-Releasing Hormone (GnRH). By administering it, the protocol stimulates the pituitary to continue producing LH, thereby preserving natural testicular function and fertility. This is a prime example of addressing the interconnectedness of the HPG axis.
- Anastrozole ∞ Testosterone can be converted into estradiol (a form of estrogen) through a process called aromatization. In men, while some estrogen is necessary for health, excessive levels can lead to side effects like water retention and gynecomastia. Anastrozole is an aromatase inhibitor; it blocks the enzyme responsible for this conversion. It is used in very small, precise doses to maintain a healthy testosterone-to-estrogen ratio, preventing side effects while ensuring testosterone can perform its functions effectively. Compounding is essential here, as the required doses are often much smaller than those available in commercial tablets.
- Enclomiphene ∞ In some protocols, enclomiphene may be used. It is a selective estrogen receptor modulator (SERM) that can block estrogen’s negative feedback at the pituitary, leading to an increase in LH and Follicle-Stimulating Hormone (FSH), further supporting the body’s endogenous testosterone production.
Effective male hormone optimization requires a multi-pronged protocol that supports the entire hypothalamic-pituitary-gonadal axis, a task made possible through the precision of compounding.

Female Hormone Balance a Delicate Recalibration
For women, hormonal balance is a complex and fluctuating dynamic, particularly during the transitions of perimenopause and menopause. The symptoms experienced ∞ hot flashes, mood swings, sleep disturbances, and low libido ∞ are the direct result of changes in the HPG axis, primarily the decline of estrogen and progesterone, but also of testosterone.
A personalized approach is even more critical for women, as their needs can change significantly over time. Compounding allows for the gentle and precise recalibration required to restore well-being.

Key Protocols in Female Hormonal Support
The goal of hormonal therapy in women is to alleviate symptoms by restoring hormones to a physiological level that is appropriate for the individual. This often involves a combination of hormones in doses that are not commercially available.
Low-Dose Testosterone ∞ Testosterone is a vital hormone for women, influencing libido, mood, energy, and muscle tone. However, the amount needed is a fraction of that required for men. FDA-approved testosterone products are formulated for male physiology, making them unsuitable for women.
Compounding pharmacies can prepare testosterone in very low-dose topical creams or for subcutaneous injection (e.g. 0.1-0.2ml of a 200mg/ml solution weekly), allowing for the administration of a dose that restores healthy levels without causing masculinizing side effects.
Progesterone ∞ Progesterone plays a crucial role in balancing the effects of estrogen, particularly in protecting the uterine lining. It also has calming effects and can aid in sleep. While oral progesterone is available commercially, doses are limited. Compounding allows for customized oral doses or the creation of topical progesterone creams.
It is important to note that for uterine protection in women taking systemic estrogen, oral progesterone is the evidence-based standard. Topical progesterone creams are not sufficiently absorbed to provide this protective effect.
Bi-Est or Tri-Est Preparations ∞ Some protocols may involve a combination of different estrogens (estradiol, estriol, and sometimes estrone). The theory is that a blend of estrogens may provide a more balanced effect. These combinations are only available through compounding. However, the clinical consensus is evolving, and many practitioners now favor using bioidentical estradiol, the body’s most potent estrogen, as it is well-researched and available in FDA-approved forms.
| Component | Typical Male Protocol Focus | Typical Female Protocol Focus | Role of Compounding |
|---|---|---|---|
| Testosterone | Restore levels to the mid-to-high normal range for men to address andropause symptoms. | Restore levels to the normal physiological range for women to address libido, energy, and mood. | Creating very low-dose formulations for women; providing specific concentrations for men. |
| Estrogen Management | Control conversion of testosterone to estradiol using an aromatase inhibitor (Anastrozole). | Supplement declining estrogen levels (primarily estradiol) to manage menopausal symptoms. | Providing micro-doses of Anastrozole for men; creating custom estrogen blends for women. |
| Pituitary/Gonadal Support | Use of Gonadorelin to maintain natural LH production and testicular function. | Primary focus is on replacing declining gonadal output; pituitary support is less common. | Providing peptides like Gonadorelin in precise formulations. |
| Progesterone | Not typically a component of male TRT. | Essential for balancing estrogen and protecting the uterus; also supports mood and sleep. | Creating customized oral doses or topical preparations. |

What Are the Regulatory Considerations for Compounded Hormones in China?
The regulatory landscape for compounded pharmaceuticals, particularly hormones, in China presents a unique set of considerations. The National Medical Products Administration (NMPA), the governing body for drugs and medical devices, maintains stringent oversight. While hospital pharmacies are permitted to compound preparations for their own patients under specific circumstances, the practice is not as widespread or accessible as in some Western countries.
The regulations prioritize the use of NMPA-approved, commercially manufactured drugs. Therefore, any practitioner considering compounded hormonal therapy within China must navigate a complex legal framework. The emphasis is heavily on demonstrating a clinical necessity for a compounded formulation over an available commercial product. This often requires extensive documentation and justification, making patient access to such personalized therapies more challenging and necessitating a deep understanding of the local procedural requirements.


Academic
An academic exploration of compounding’s role in endocrine management requires a shift in perspective toward the molecular and physiological mechanisms that govern hormonal homeostasis. We move from the “what” and “how” to the “why,” examining the intricate biochemical pathways and receptor-level interactions that these personalized therapies seek to influence.
The endocrine system’s interconnectedness is not just a concept; it is a physical reality dictated by the shared origins of steroid hormones, the competitive binding for transport proteins, and the complex feedback signals that integrate the Hypothalamic-Pituitary-Adrenal (HPA), Hypothalamic-Pituitary-Gonadal (HPG), and Hypothalamic-Pituitary-Thyroid (HPT) axes. Compounding, from this academic viewpoint, is a form of applied pharmacology that attempts to modulate this multi-axis network with a high degree of specificity.
The foundation of this approach lies in understanding steroidogenesis. All steroid hormones, including cortisol, aldosterone, testosterone, and estradiol, are derived from a common precursor molecule ∞ cholesterol. The enzymatic pathways that convert cholesterol into these various end-products are complex and interconnected.
A therapeutic intervention that introduces a high dose of one hormone can create a substrate shift, altering the production of other hormones downstream. For example, supplementing with pregnenolone, a precursor hormone, can potentially increase levels of both cortisol and DHEA. The clinical outcome depends on the individual’s unique enzymatic efficiencies. It is this biochemical reality that necessitates a personalized and carefully monitored approach, one that compounding is uniquely suited to provide.

The HPA and HPG Axis Crosstalk a Target for Compounded Peptides
The relationship between the body’s stress response system (HPA axis) and reproductive system (HPG axis) is a critical area of endocrine science. Chronic activation of the HPA axis, leading to elevated levels of corticotropin-releasing hormone (CRH) and cortisol, has a known suppressive effect on the HPG axis.
CRH can directly inhibit the release of Gonadotropin-Releasing Hormone (GnRH) from the hypothalamus, thereby reducing the pituitary’s output of LH and FSH. This can lead to suppressed testosterone levels in men and menstrual irregularities in women. This interaction explains why periods of intense stress can profoundly impact reproductive health. This crosstalk provides a compelling rationale for therapies that can modulate these axes with precision, a role increasingly filled by compounded peptides.

Growth Hormone Secretagogues Modulating the Pituitary
Peptides are short chains of amino acids that act as signaling molecules. Several compounded peptides, known as Growth Hormone Secretagogues (GHS), are used to stimulate the pituitary gland’s natural production and release of Human Growth Hormone (HGH). This approach is fundamentally different from administering synthetic HGH directly.
By stimulating the body’s own production, these peptides preserve the natural, pulsatile release of HGH, which is crucial for its physiological effects and safety profile. This mimics the body’s own regulatory mechanisms, making it a more nuanced intervention.
- Sermorelin ∞ Sermorelin is an analogue of the first 29 amino acids of Growth Hormone-Releasing Hormone (GHRH). It binds to the GHRH receptor on the pituitary, directly stimulating it to produce and release HGH. Its action is dependent on a functioning pituitary and is subject to the body’s own negative feedback mechanisms via somatostatin, which prevents excessive HGH release.
- CJC-1295 and Ipamorelin ∞ This is a commonly used synergistic combination. CJC-1295 is another GHRH analogue with a much longer half-life, providing a sustained stimulus for HGH production. Ipamorelin is a ghrelin mimetic and a selective GH-releasing peptide (GHRP). It acts on a different receptor in the pituitary (the GHS-R) to stimulate HGH release. By stimulating the pituitary through two different pathways simultaneously (GHRH receptor and ghrelin receptor), this combination can produce a more robust and synergistic release of HGH, while still operating within the body’s physiological control systems.
The use of these peptides has implications beyond just increasing HGH. HGH influences metabolism, body composition, and tissue repair. By optimizing HGH levels in a physiological manner, these peptides can help counteract some of the catabolic effects of chronic cortisol elevation from HPA axis activation, thereby indirectly supporting the function of other endocrine axes, including the HPG axis.
Compounded peptides represent a sophisticated therapeutic modality, enabling precise, receptor-level modulation of the pituitary to restore physiological hormonal rhythms.

Advanced Peptide Applications in Systemic Regulation
Beyond the Growth Hormone Secretagogues, compounding pharmacies prepare other specialized peptides that target specific pathways related to sexual health, tissue repair, and inflammation. These peptides further illustrate how a personalized approach can address the interconnected nature of physiological function.

PT-141 a Neuromodulatory Approach to Sexual Health
PT-141, or Bremelanotide, operates on a completely different axis from traditional sexual health medications. While drugs like sildenafil target the vascular system to improve blood flow, PT-141 is a melanocortin receptor agonist. It acts within the central nervous system to directly influence the pathways of sexual desire and arousal.
It was approved by the FDA for hypoactive sexual desire disorder (HSDD) in premenopausal women. Its mechanism highlights the profound connection between the brain (neurotransmitters and neuromodulators) and the endocrine system’s expression of sexual function. Compounding allows PT-141 to be prepared as a subcutaneous injection or a nasal spray, providing a targeted intervention for individuals whose sexual dysfunction may have a central, rather than purely vascular, origin.

Pentadeca Arginate (PDA) for Tissue Repair and Inflammation
Inflammation is a key process that links metabolic dysfunction, stress, and hormonal imbalance. Chronic inflammation can impair hormone receptor sensitivity and contribute to a wide range of age-related diseases. Pentadeca Arginate (PDA) is a peptide used for its systemic effects on tissue repair and inflammation modulation.
It is a stable analogue of a naturally occurring peptide, BPC-157. PDA is believed to promote angiogenesis (the formation of new blood vessels), modulate nitric oxide production, and accelerate the healing of various tissues, including muscle, tendon, and the gut lining.
By addressing systemic inflammation and supporting tissue integrity, peptides like PDA can help create a more favorable internal environment for the endocrine system to function optimally. A healthy gut barrier, for instance, reduces the inflammatory load on the body, which can lessen the burden on the HPA axis and improve overall metabolic health.
| Peptide | Primary Target Receptor/Pathway | Physiological Effect | Connection to Endocrine Interconnectedness |
|---|---|---|---|
| Sermorelin / CJC-1295 | Growth Hormone-Releasing Hormone Receptor (GHRH-R) in the pituitary. | Stimulates natural, pulsatile release of Human Growth Hormone (HGH). | Modulates the pituitary, a central endocrine gland, impacting metabolism and body composition, which influences other hormonal axes. |
| Ipamorelin | Ghrelin Receptor (GHS-R) in the pituitary. | Stimulates HGH release; mimics the action of the “hunger hormone” ghrelin. | Acts synergistically with GHRH analogues, demonstrating how multiple signaling pathways converge on the pituitary to regulate HGH. |
| PT-141 (Bremelanotide) | Melanocortin Receptors (MC3-R, MC4-R) in the central nervous system. | Increases sexual desire and arousal through neuromodulation. | Directly links the central nervous system to the expression of sexual function, bypassing peripheral hormonal and vascular pathways. |
| Pentadeca Arginate (PDA) | Multiple pathways involved in angiogenesis and inflammation. | Accelerates tissue repair, reduces inflammation, and supports gut integrity. | Addresses systemic inflammation, a factor that negatively impacts all endocrine axes by impairing receptor sensitivity and increasing allostatic load. |

How Might International Regulations Impact the Sourcing of Raw Materials for Compounding in China?
The global nature of the pharmaceutical supply chain means that international regulations can significantly impact the availability and quality of Active Pharmaceutical Ingredients (APIs) used for compounding in China. The NMPA has its own set of rigorous standards for API importation, often requiring documentation equivalent to Good Manufacturing Practices (GMP) certification from the country of origin.
Geopolitical tensions, trade policies, or regulatory changes in major API-exporting countries can disrupt the supply chain, leading to shortages or increased costs. Furthermore, China’s own “dual circulation” economic strategy, which aims to boost domestic production while remaining open to international trade, could incentivize the development of a more robust domestic API manufacturing sector.
For compounding pharmacies, this means that ensuring a consistent supply of high-quality, legally imported raw materials for hormonal and peptide preparations requires a sophisticated understanding of both domestic and international regulatory landscapes, as well as meticulous supply chain management.

References
- Bhasin, S. et al. “Testosterone Therapy in Men with Hypogonadism ∞ An Endocrine Society Clinical Practice Guideline.” The Journal of Clinical Endocrinology & Metabolism, vol. 103, no. 5, 2018, pp. 1715 ∞ 1744.
- Santoro, N. et al. “Compounded Bioidentical Hormones in Endocrinology Practice ∞ An Endocrine Society Scientific Statement.” The Journal of Clinical Endocrinology & Metabolism, vol. 101, no. 4, 2016, pp. 1318 ∞ 1343.
- Walker, W. H. “Sermorelin ∞ a better approach to management of adult-onset growth hormone insufficiency?” Clinical Interventions in Aging, vol. 1, no. 4, 2006, pp. 307 ∞ 308.
- Glaser, R. & York, A. E. “Subcutaneous testosterone anastrozole therapy in men ∞ rationale, dosing, and levels on therapy.” Postgraduate Medicine, vol. 131, no. 3, 2019, pp. 195-203.
- Davis, S. R. & Wahlin-Jacobsen, S. “Testosterone in women ∞ the clinical significance.” The Lancet Diabetes & Endocrinology, vol. 3, no. 12, 2015, pp. 980 ∞ 992.
- Molinoff, P. B. & Rudd, G. D. “Bremelanotide for hypoactive sexual desire disorder.” The Medical Letter on Drugs and Therapeutics, vol. 61, no. 1581, 2019, pp. 132-134.
- Teichman, S. L. et al. “CJC-1295, a long-acting growth hormone-releasing factor analog.” The Journal of Clinical Endocrinology & Metabolism, vol. 91, no. 3, 2006, pp. 799-805.
- Sei, Y. et al. “The stomach-derived peptide ghrelin increases voluntary running distance in mice.” The Journal of Endocrinology, vol. 196, no. 3, 2008, pp. 621-628.
- Tsikouras, P. et al. “The role of HPG and HPA axis in the pathogenesis of adolescent PCOS.” Reproductive Biology and Endocrinology, vol. 12, no. 1, 2014, p. 49.

Reflection

Charting Your Own Biological Course
The information presented here offers a map of the intricate biological landscape within you. It details the pathways, the messengers, and the systems that collectively create your daily experience of health and well-being. This knowledge is a powerful tool. It transforms abstract feelings of being “off” into understandable physiological processes.
It provides a language to articulate your experience and a framework to understand potential solutions. This map, however, is not the territory. Your personal biology, your life experiences, and your unique goals define the terrain.
The journey toward optimal health is a personal one. The data from lab reports and the insights from clinical science are the navigational aids, but you are the one at the helm. Reflect on how these systems might be playing out in your own life.
Consider the subtle connections between your energy levels, your stress, your sleep, and your mood. Understanding the science is the foundational step. The next is to use that understanding to ask more informed questions and to engage in a collaborative partnership with a knowledgeable practitioner who can help you interpret your unique map. The potential to recalibrate your system and reclaim your vitality lies within this informed, proactive, and deeply personal process.

Glossary

endocrine system

stress response

hpa axis

hpg axis

compounding pharmacies

testosterone cypionate

gonadorelin

anastrozole

progesterone

low-dose testosterone

compounded peptides

growth hormone secretagogues

growth hormone

sermorelin

ipamorelin

cjc-1295

tissue repair
central nervous system

sexual desire

hypoactive sexual desire disorder




