

Fundamentals
The feeling often begins as a subtle dissonance, a sense that the person you are does not quite align with the body you inhabit. It could be a persistent fatigue that sleep does not resolve, a fog that clouds concentration, or a quiet decline in physical strength and desire.
Your internal world feels off-key. This experience is a valid and frequent starting point for investigating your hormonal health. The body’s endocrine system Meaning ∞ The endocrine system is a network of specialized glands that produce and secrete hormones directly into the bloodstream. is its internal communication network, a collection of glands that produce and secrete hormones. These chemical messengers travel through the bloodstream, instructing tissues and organs on what to do, how to function, and when to adapt. This network maintains the body’s internal balance, a state known as homeostasis.
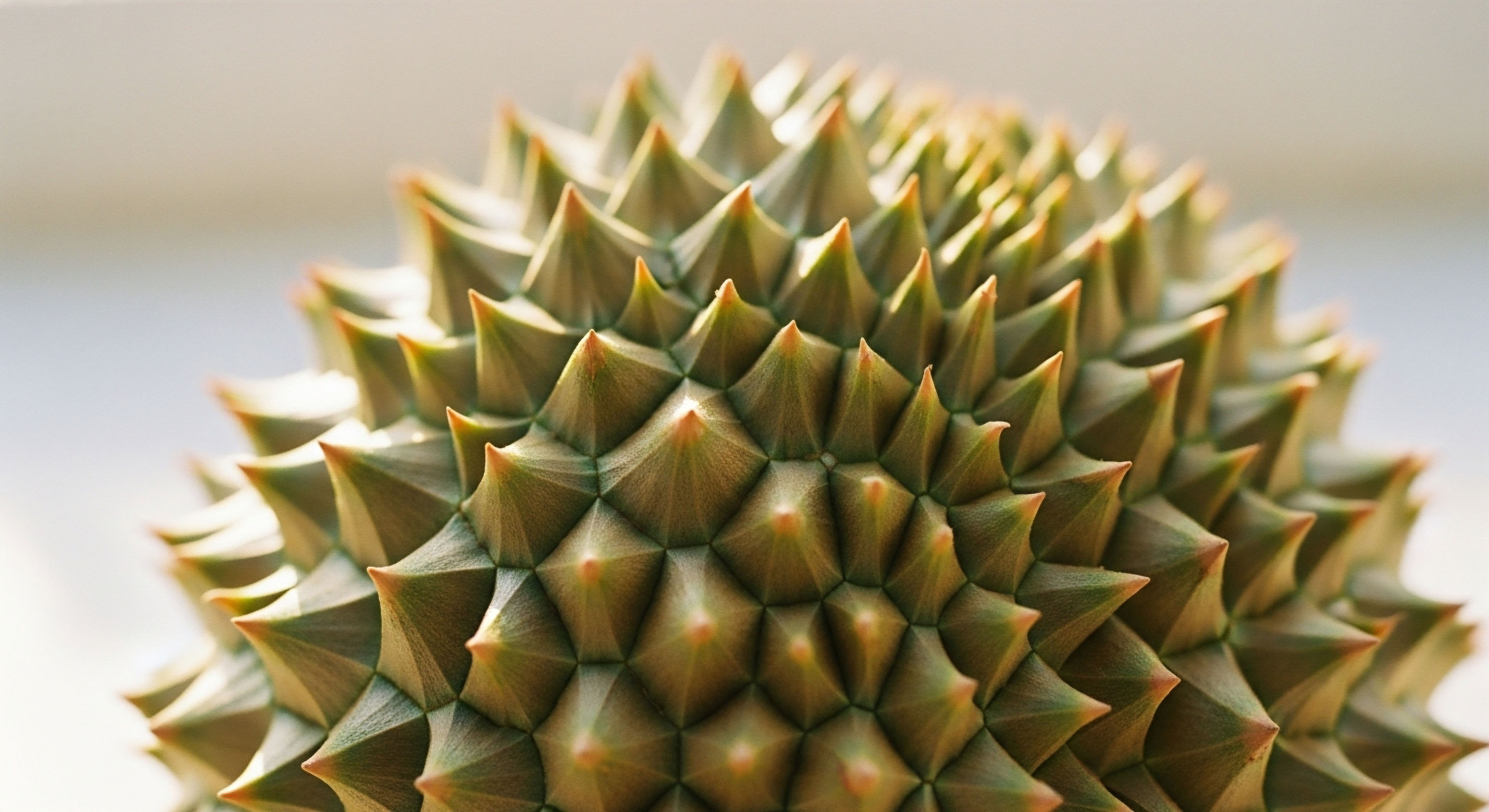
Think of this intricate system as a biological orchestra. Each hormone is an instrument, and each gland is a section of that orchestra. For the music to be coherent and powerful, every instrument must play in concert, guided by a conductor who understands the entire composition.
The hypothalamic-pituitary-gonadal (HPG) axis, for instance, is a primary trio in this orchestra, a feedback loop where the brain signals the pituitary gland, which in turn signals the testes or ovaries to produce hormones like testosterone or estrogen. The levels of these hormones then signal back to the brain, creating a self-regulating circuit. This constant communication ensures that hormonal concentrations remain within a precise and healthy range, much like a thermostat maintains a room’s temperature.

What Is the Conductor’s Role in Hormonal Health?
A monitored hormonal therapy Meaning ∞ Hormonal therapy is the medical administration of hormones or agents that modulate the body’s natural hormone production and action. protocol is one where a clinician acts as the conductor. This professional reads the entire score ∞ your unique combination of symptoms, comprehensive lab results, and personal health history. This detailed information allows for precise adjustments, ensuring that any therapeutic intervention supports the entire system’s equilibrium.
The goal of a guided protocol is to restore the orchestra’s intended harmony, allowing each biological system to perform its function optimally. The process is dynamic, requiring periodic checks and fine-tuning as the body adapts and changes over time.
Unmonitored hormonal therapy introduces a powerful instrument to the body’s orchestra without a conductor, risking systemic discord.
Conversely, unmonitored hormonal therapy is akin to an instrument deciding to play its own tune at maximum volume, disregarding the rest of the orchestra. Sourcing hormones without clinical oversight or attempting to manage your own dosage based on generalized information introduces a potent biochemical agent into a delicate system without understanding its downstream consequences.
Because every hormone is interconnected, altering one without accounting for the others can initiate a cascade of imbalances. An unguided approach might temporarily address one symptom while creating several new, and potentially more severe, problems elsewhere in the body. It is a biological gamble with your long-term wellness as the stake.


Intermediate
When hormonal therapies are administered without diligent clinical supervision, the intended benefits can become obscured by a host of unintended consequences. The body’s response to an influx of exogenous hormones is complex and systemic. A dose of testosterone, for example, does not simply increase testosterone levels in isolation.
It influences a wide array of interconnected metabolic and physiological pathways. Without monitoring, these secondary effects can progress unchecked, undermining long-term health Meaning ∞ Long-Term Health signifies a sustained state of optimal physiological function, disease resilience, and mental well-being over an extended period. in profound ways. The core issue is a disruption of the body’s finely tuned feedback mechanisms, creating a state of sustained biological stress.

The Domino Effect of Unchecked Hormones
One of the most immediate risks of unmanaged testosterone therapy is the development of erythrocytosis, a condition characterized by an overproduction of red blood cells. While testosterone does stimulate red blood cell production, a medically supervised protocol involves monitoring hematocrit levels to keep them within a safe range.
Unchecked, elevated hematocrit thickens the blood, increasing the risk of blood clots, stroke, and other serious cardiovascular events. This is a clear example of how a therapeutic agent can produce a dangerous side effect when its physiological impact is not properly tracked and managed.
Another critical area of concern is the balance between testosterone and estrogen. The enzyme aromatase converts a portion of testosterone into estradiol, a form of estrogen. This conversion is a normal and necessary process for both male and female health. However, introducing high levels of testosterone without managing this conversion can lead to elevated estrogen levels.
In men, this can manifest as gynecomastia (enlargement of breast tissue), water retention, and mood instability. Clinically monitored protocols often include an aromatase inhibitor Meaning ∞ An aromatase inhibitor is a pharmaceutical agent specifically designed to block the activity of the aromatase enzyme, which is crucial for estrogen production in the body. like Anastrozole to maintain this delicate balance, a step that is almost always overlooked in unmonitored scenarios.
Properly supervised hormonal therapy anticipates and manages downstream biochemical conversions, a critical safety measure absent in unguided approaches.
The following table illustrates the contrast between the goals of a therapeutic protocol and the potential systemic consequences when that protocol is not guided by clinical oversight.
| Therapeutic Goal | Potential Unmonitored Consequence | Mechanism of Imbalance |
|---|---|---|
| Increase Energy and Libido | Cardiovascular Strain | Unchecked erythrocytosis (high red blood cell count) thickens the blood, increasing clot risk. |
| Enhance Muscle Mass | Hormonal Imbalance (High Estrogen) | Excess testosterone converts to estradiol via the aromatase enzyme, leading to side effects. |
| Improve Mood and Cognition | Natural Production Shutdown | The HPG axis detects high external hormone levels and ceases its own production, leading to testicular atrophy. |
| Strengthen Bone Density | Worsening of Pre-existing Conditions | Conditions like benign prostatic hyperplasia (BPH) or sleep apnea can be exacerbated without proper screening and management. |

Key Biomarkers for Safe Hormonal Optimization
A supervised protocol relies on regular blood work to ensure the therapy is both effective and safe. These tests provide a clear view of the body’s response and allow for precise adjustments. Key markers include:
- Total and Free Testosterone ∞ To ensure levels are within the optimal therapeutic range.
- Estradiol (E2) ∞ To manage the conversion of testosterone to estrogen and prevent related side effects.
- Complete Blood Count (CBC) ∞ Specifically monitoring hematocrit and hemoglobin to prevent erythrocytosis.
- Prostate-Specific Antigen (PSA) ∞ To monitor prostate health, as therapy could potentially accelerate the growth of an undiagnosed cancer.
- Sex Hormone-Binding Globulin (SHBG) ∞ To understand how much testosterone is bioavailable to the body’s tissues.
- Luteinizing Hormone (LH) and Follicle-Stimulating Hormone (FSH) ∞ To assess the degree of natural production suppression.
Without this information, any attempt at hormonal therapy is effectively flying blind. The long-term health consequences, including an increased risk for certain cancers and cardiovascular events, are not theoretical possibilities; they are direct outcomes of sustained biological imbalance.


Academic
A sophisticated analysis of unmonitored hormonal therapies requires a deep appreciation for the molecular architecture of the endocrine system. The long-term health consequences extend beyond simple side effects; they represent a fundamental disruption of cellular signaling, gene expression, and homeostatic regulation.
Examining the specific interplay between exogenous androgens, the aromatase enzyme system, and sex hormone-binding globulin Meaning ∞ Sex Hormone-Binding Globulin, commonly known as SHBG, is a glycoprotein primarily synthesized in the liver. (SHBG) provides a compelling case study in the risks of unsupervised biochemical intervention. The individuality of these systems, influenced by genetic polymorphisms, makes a standardized, unmonitored approach particularly hazardous.

Molecular Mechanisms of Endocrine Disruption
When exogenous testosterone is introduced, it saturates androgen receptors, producing desired effects on muscle and bone. Simultaneously, it becomes a substrate for the enzyme aromatase (cytochrome P450 19A1), which catalyzes its conversion to 17β-estradiol. The rate of this conversion is highly variable among individuals, partly due to genetic variations in the CYP19A1 gene.
In an unmonitored setting, an individual with high aromatase activity can experience a dramatic surge in estradiol levels. This supraphysiological estrogen environment has profound effects. It can downregulate androgen receptor expression, increase SHBG production in the liver, and contribute to insulin resistance. The resulting high SHBG levels further reduce the amount of free, biologically active testosterone, paradoxically recreating some of the symptoms of testosterone deficiency that the therapy was intended to treat.
This creates a problematic feedback scenario where an individual might increase their testosterone dose to chase the desired effects, further exacerbating the underlying estradiol and SHBG imbalance. This is a state of iatrogenic endocrine chaos. A clinically supervised protocol preempts this by measuring estradiol and SHBG and titrating the testosterone dose accordingly, sometimes adding a specific aromatase inhibitor to control the conversion process. This level of precision is impossible to achieve without regular, detailed laboratory analysis.
How Does Lifelong Exposure Inform Therapeutic Risks?
Mendelian randomization studies offer a powerful tool for understanding the lifelong causal effects of hormone levels. By using genetic variants as proxies for lifelong exposure to higher or lower testosterone levels, researchers can infer long-term health outcomes without the time and cost constraints of decades-long clinical trials.
A significant 2020 study in eLife used this method to analyze data from over 160,000 men. The findings suggest that lifelong increased free testosterone is causally linked to beneficial effects like increased bone mineral density and decreased body fat. The same data also revealed causal links to adverse effects, including an increased risk of prostate cancer and hypertension.
Genetic studies suggest that while higher testosterone offers some benefits, it is causally linked to increased risks of certain diseases, making clinical oversight of therapy essential.
These findings are critical. They demonstrate that the risks associated with high testosterone are not merely correlational; they are embedded in the biological pathways that testosterone influences over a lifetime. Unmonitored therapy that pushes testosterone levels into the supraphysiological range, even intermittently, is essentially replicating a high-risk genetic profile.
It exposes the individual to the long-term consequences of elevated androgen activity without any of the body’s natural compensatory mechanisms. The increased risk for prostate cancer, for example, underscores why PSA screening and digital rectal exams are non-negotiable components of any responsible TRT protocol.
The following table presents a hypothetical case study to illustrate the divergence between an unmonitored and a monitored therapeutic path.
| Parameter | Patient on Unmonitored Therapy (6 Months) | Patient on Monitored Protocol (6 Months) |
|---|---|---|
| Presenting Complaint | Initial improvement, now has fatigue, moodiness, and breast tenderness. | Sustained improvement in energy, mood, and libido. |
| Total Testosterone | 1200 ng/dL (Supraphysiological) | 850 ng/dL (High-Normal Therapeutic Range) |
| Free Testosterone | 15 pg/mL (Low-Normal) | 25 pg/mL (Optimal) |
| Estradiol (E2) | 65 pg/mL (High) | 30 pg/mL (Controlled) |
| Hematocrit | 54% (High Risk) | 48% (Safe Range) |
| SHBG | 70 nmol/L (High) | 35 nmol/L (Normal) |
| Clinical Outcome | High risk of thromboembolic event; experiencing side effects from hormonal imbalance; natural production fully suppressed. | Symptoms resolved; risks managed; protocol includes measures to maintain some natural function (e.g. Gonadorelin). |

References
- Khera, M. & Naughton, C. (2016). Adverse effects of testosterone replacement therapy ∞ an update on the evidence and controversy. Therapeutic Advances in Urology, 8(6), 395 ∞ 403.
- Rizk, P. J. Kedia, S. & Khera, M. (2014). Risks of testosterone replacement therapy in men. Indian Journal of Urology, 30(4), 411 ∞ 416.
- Morgentaler, A. (2016). How Safe is Long Term Testosterone Replacement Therapy Use? Urology Austin.
- Mayo Clinic Staff. (2022). Testosterone therapy ∞ Potential benefits and risks as you age. Mayo Clinic.
- Paré, G. et al. (2020). Effects of lifelong testosterone exposure on health and disease using Mendelian randomization. eLife, 9, e58914.

Reflection
You arrived here seeking to understand the dissonance between how you feel and how you wish to function. The information presented clarifies that your body’s hormonal system is a complex, interconnected network where every action has a reaction. The path toward reclaiming your vitality is paved with this understanding.
This knowledge is the first and most powerful step. It transforms you from a passive recipient of symptoms into an active, informed participant in your own health. Your biology is not a mystery to be solved by a single, isolated intervention. It is a dynamic system waiting to be guided back into balance. What is the next question you will ask on your path to wellness?










