

Fundamentals
The sensation of waking up feeling unrestored, as if the night offered no respite, is a deeply personal and often frustrating experience. You might trace it to a stressful day or a late meal, yet the pattern persists, weaving itself into the fabric of your daily life.
This experience of unrefreshing sleep is frequently a direct communication from your body’s intricate internal messaging system, the endocrine network. The quality of your sleep is profoundly linked to the rhythmic rise and fall of hormones, the chemical conductors of your biological orchestra. When these hormonal signals become distorted or faint, the symphony of sleep is disrupted, leaving you feeling the consequences long after the sun has risen.
Understanding this connection is the first step toward reclaiming your nights. Your body operates on a sophisticated 24-hour cycle, a circadian rhythm that governs nearly every physiological process, including the release of key hormones that either promote wakefulness or induce sleep.
This is a delicate, reciprocal relationship; hormones direct sleep, and in turn, the quality and duration of your sleep directly influence hormonal production. A disruption in one area creates a cascade of effects in the other, initiating a cycle that can be difficult to break without a clear comprehension of the underlying mechanics.

The Core Sleep Regulators
At the heart of your sleep-wake cycle are several key hormonal players. Cortisol, often labeled the “stress hormone,” naturally peaks in the morning to promote alertness and gradually declines throughout the day, reaching its lowest point at night to allow for sleep.
Conversely, melatonin, produced in the pineal gland in response to darkness, signals to your body that it is time to rest. This elegant opposition of cortisol and melatonin is fundamental to a healthy sleep pattern. When the rhythm is disturbed ∞ for instance, with elevated evening cortisol levels due to chronic stress ∞ the body receives a confusing signal to stay alert, making it difficult to fall asleep and stay asleep.
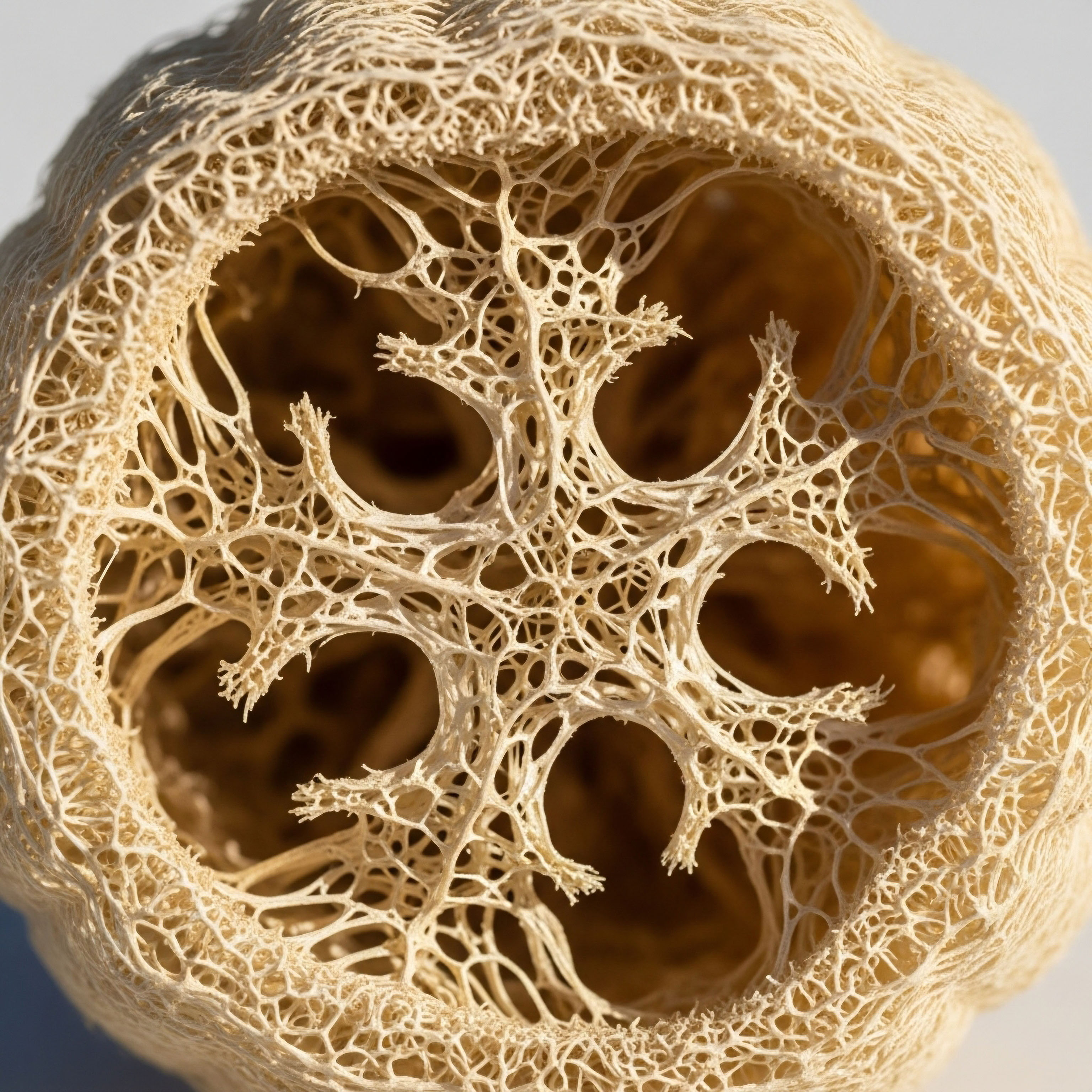
Simultaneously, growth hormone (GH) is released in pulses during the deepest stages of sleep, known as slow-wave sleep. This period is critical for cellular repair, muscle growth, and overall physical restoration. Insufficient deep sleep, often a consequence of hormonal imbalance, curtails this vital restorative process, contributing to daytime fatigue and a diminished sense of well-being.
The intricate dance between these hormones dictates the architecture of your sleep, from the ease of falling asleep to the time spent in each restorative stage.

Hormonal Shifts through Life’s Seasons
The stability of this hormonal system is not static; it evolves throughout your lifespan, presenting unique challenges at different stages. These transitions are not pathological events but natural progressions in your biological timeline. Each phase, however, brings a new hormonal landscape that can significantly alter sleep quality.
- Puberty ∞ The surge of sex hormones, including testosterone and estrogen, during adolescence can recalibrate the sleep-wake cycle, often leading to a natural shift toward later bedtimes and wake times.
- The Menstrual Cycle ∞ Throughout a woman’s reproductive years, the monthly fluctuation of estrogen and progesterone can influence sleep architecture. Progesterone has a sleep-promoting, sedative-like effect, while its decline before menstruation can contribute to sleep disturbances.
- Pregnancy ∞ This period involves dramatic hormonal shifts, with soaring levels of progesterone in the first trimester often causing daytime sleepiness, while physical discomfort and other hormonal changes can disrupt sleep in later stages.
- Perimenopause and Menopause ∞ For women, the decline in estrogen and progesterone during this transition is a primary driver of sleep problems. The reduction of these hormones can lead to symptoms like hot flashes and night sweats, which directly fragment sleep. The loss of progesterone’s calming influence further contributes to insomnia.
- Andropause ∞ In men, the gradual decline of testosterone with age can also impact sleep. Lower testosterone levels are associated with decreased sleep efficiency, more frequent awakenings, and a reduction in restorative deep sleep.
Recognizing that these life stages bring predictable hormonal changes allows for a more informed and proactive approach to managing sleep. The symptoms you experience are not isolated incidents but are often rooted in these profound biological shifts. By understanding the specific hormonal context of your life stage, you can begin to connect your personal experience of poor sleep to its physiological source, transforming confusion into clarity and paving the way for targeted, effective solutions.


Intermediate
Moving beyond the foundational understanding of hormones and sleep, we can examine the precise mechanisms through which these biochemical messengers sculpt your nightly rest. The lived experience of waking at 3 a.m. with a racing mind or feeling perpetually exhausted despite a full night in bed is not an abstract complaint; it is a direct reflection of specific disruptions within your endocrine system.
A deeper analysis reveals how the shifting concentrations of key hormones at different life stages directly alter sleep architecture, and how targeted clinical protocols can work to restore balance and function.
The architecture of your sleep is a direct blueprint of your hormonal health, with specific imbalances creating predictable patterns of disruption.
The transition from healthy, consolidated sleep to fragmented, unrefreshing rest is often a gradual process, mirroring the slow drift of hormonal levels over time. In women, the journey through perimenopause provides a clear example of this connection. In men, the steady decline of testosterone during andropause creates a different, yet equally impactful, set of challenges. Understanding these gender-specific hormonal journeys is essential for identifying the root cause of sleep disturbances and designing effective interventions.

The Female Hormonal Axis and Sleep Fragmentation
For many women, sleep quality begins to change noticeably during perimenopause, the transitional period before menopause. This is primarily driven by the fluctuating and eventual decline of two key ovarian hormones ∞ estrogen and progesterone. Their influence on sleep is both direct and indirect.

Estrogen’s Role in Sleep Stability
Estrogen plays a significant role in regulating body temperature, mood, and neurotransmitter function, all of which are connected to sleep. Its decline can disrupt the body’s thermoregulatory system, leading to the characteristic vasomotor symptoms of hot flashes and night sweats.
These sudden episodes of intense heat and perspiration can cause abrupt awakenings, shattering sleep continuity and preventing the brain from cycling through its necessary restorative stages. Furthermore, estrogen helps support the function of serotonin and dopamine, neurotransmitters that contribute to a stable mood and feelings of well-being. As estrogen levels fall, this support diminishes, which can contribute to the anxiety and depressive symptoms that often accompany this life stage and further interfere with sleep.

Progesterone the Calming Agent
Progesterone’s impact on sleep is perhaps more direct. It functions as a calming agent in the central nervous system, partly through its metabolite, allopregnanolone, which interacts with GABA-A receptors ∞ the same receptors targeted by many sedative medications. This produces a natural anxiolytic and sleep-promoting effect.
Progesterone also acts as a respiratory stimulant. As progesterone levels decline during perimenopause and post-menopause, women lose this natural calming influence, which can manifest as increased anxiety, difficulty falling asleep, and a higher incidence of sleep-disordered breathing.
Hormonal optimization protocols are designed to re-establish the physiological signaling that supports deep, restorative sleep cycles.
Addressing these deficiencies requires a personalized approach. For women experiencing significant sleep disruption related to perimenopause or menopause, hormonal optimization protocols can be highly effective. These are not one-size-fits-all solutions but are carefully tailored based on an individual’s symptoms and lab results.
| Protocol Component | Mechanism of Action | Targeted Sleep Benefit |
|---|---|---|
| Progesterone Therapy | Acts on GABA-A receptors in the brain, producing a calming, sedative-like effect. It also helps stabilize the uterine lining. | Reduces sleep latency (time to fall asleep), decreases nighttime awakenings, and can alleviate anxiety. |
| Estrogen Therapy | Stabilizes thermoregulation in the hypothalamus, reducing the frequency and intensity of hot flashes and night sweats. | Improves sleep continuity by minimizing vasomotor-related awakenings. |
| Low-Dose Testosterone | Can improve energy levels, mood, and libido. Its direct impact on sleep architecture is still being studied, but it contributes to overall well-being, which indirectly supports better sleep. | Enhances overall vitality and mood, reducing the psychological distress that can interfere with sleep. |

The Male Hormonal Axis and Declining Sleep Quality
In men, the age-related decline in testosterone production, a condition known as andropause or late-onset hypogonadism, is a primary driver of changes in sleep quality. Testosterone levels peak in early adulthood and then gradually decrease by approximately 1-2% per year after the age of 30. This slow decline can lead to a constellation of symptoms, including fatigue, reduced muscle mass, mood changes, and significantly, disrupted sleep.

Testosterone’s Influence on Sleep Architecture
Testosterone appears to play a role in maintaining deep, restorative slow-wave sleep. Studies have shown that men with lower testosterone levels often experience less time in this critical sleep stage, along with increased nighttime awakenings and overall lower sleep efficiency.
The relationship is bidirectional ∞ low testosterone can impair sleep, and poor sleep (particularly fragmented sleep) can further suppress testosterone production, creating a self-perpetuating cycle of fatigue and hormonal imbalance. Additionally, low testosterone is often associated with an increase in body fat and a decrease in muscle tone, particularly in the upper airway, which can increase the risk or severity of obstructive sleep apnea (OSA), a condition characterized by repeated interruptions in breathing during sleep.

Clinical Interventions for Men
For men with clinically low testosterone levels and associated symptoms, Testosterone Replacement Therapy (TRT) can be a powerful tool for restoring vitality and improving sleep. The goal of TRT is to return testosterone levels to a healthy, youthful range, thereby alleviating the symptoms of deficiency.
- Testosterone Cypionate Injections ∞ A common protocol involves weekly intramuscular or subcutaneous injections of Testosterone Cypionate. This method provides stable, predictable hormone levels, helping to restore the physiological environment that supports healthy sleep architecture.
- Ancillary Medications ∞ To manage potential side effects and support the body’s natural hormonal balance, TRT protocols for men often include other medications. Anastrozole, an aromatase inhibitor, is used to control the conversion of testosterone to estrogen, preventing potential side effects like water retention. Gonadorelin or hCG may be used to stimulate the testes directly, maintaining their function and size during therapy.
- Monitoring and Adjustment ∞ Effective TRT requires careful monitoring of blood levels of testosterone, estrogen, and other relevant markers. Dosages are adjusted based on lab results and the patient’s subjective response to treatment, ensuring a personalized approach that maximizes benefits while minimizing risks.
By addressing the root hormonal deficiency, these protocols can lead to significant improvements in sleep quality, including more consolidated sleep, increased deep sleep, and a reduction in the daytime fatigue that plagues so many men experiencing andropause.


Academic
A sophisticated examination of hormonal influence on sleep transcends the individual actions of sex steroids and delves into the complex, interconnected neuroendocrine systems that govern consciousness, metabolism, and cellular restoration. The deterioration of sleep quality across life stages is a manifestation of systemic dysregulation, particularly within the Hypothalamic-Pituitary-Adrenal (HPA) and Hypothalamic-Pituitary-Gonadal (HPG) axes.
Furthermore, the therapeutic application of peptides that modulate the Growth Hormone (GH) axis offers a targeted intervention point for restoring sleep architecture, highlighting the intricate relationship between somatotropic function and neurophysiological rest.

Interplay of the HPA and HPG Axes in Sleep Regulation
The HPA axis, the body’s central stress response system, and the HPG axis, which governs reproductive function, are deeply intertwined, and their coordinated activity is fundamental to healthy sleep. The HPA axis is driven by the pulsatile release of corticotropin-releasing hormone (CRH) from the hypothalamus, which stimulates the pituitary to release adrenocorticotropic hormone (ACTH), in turn signaling the adrenal glands to produce cortisol.
A properly functioning HPA axis exhibits a distinct circadian rhythm, with cortisol levels peaking upon waking (the cortisol awakening response) and reaching a nadir in the late evening, facilitating sleep onset.
Chronic stress, aging, and the hormonal shifts of menopause and andropause can lead to HPA axis dysfunction, characterized by a flattening of the cortisol curve. This may involve elevated evening cortisol levels, which act as a powerful wakefulness signal, disrupting sleep initiation and maintenance.
Concurrently, the decline in gonadal hormones like estrogen and testosterone weakens the inhibitory feedback these hormones normally exert on the HPA axis. Estrogen, for example, helps to buffer the cortisol response. Its decline during menopause can lead to a state of relative HPA axis overactivity, contributing to the hyperarousal and anxiety that underpin many cases of menopausal insomnia. This creates a vicious cycle ∞ HPA axis hyperactivity fragments sleep, and fragmented sleep further dysregulates the HPA axis.

How Does Peptide Therapy Modulate Sleep Architecture?
Beyond the primary sex hormones, the somatotropic axis, which regulates growth hormone, presents a powerful and precise target for sleep modulation. The release of Growth Hormone-Releasing Hormone (GHRH) from the hypothalamus not only stimulates the pituitary to release GH but also appears to be a primary promoter of slow-wave sleep (SWS), the deepest and most physically restorative stage of sleep.
The majority of GH is secreted during these deep sleep periods. Age-related decline in GH production is paralleled by a decrease in SWS, leading to less restorative sleep and contributing to the symptoms of aging.
Growth Hormone Peptide Therapy utilizes specific, targeted peptides to stimulate the body’s own production of GH in a more physiological, pulsatile manner than direct GH administration. This approach can have profound effects on sleep architecture.
| Peptide | Mechanism of Action | Observed Effects on Sleep |
|---|---|---|
| Sermorelin | A GHRH analog that directly stimulates the pituitary gland to produce and release GH. It has a short half-life, mimicking the natural pulsatile release of GHRH. | Increases the amount of time spent in SWS, leading to more restorative sleep and improved daytime energy levels. |
| Ipamorelin / CJC-1295 | Ipamorelin is a Growth Hormone Secretagogue (GHS) that mimics ghrelin, stimulating GH release with high specificity and without significantly affecting cortisol. CJC-1295 is a GHRH analog with an extended half-life, providing a sustained signal for GH production. | This combination provides a strong, synergistic effect, leading to a significant increase in both the amplitude and duration of GH pulses. This robustly enhances SWS, improves sleep consolidation, and promotes cellular repair. |
| Tesamorelin | A potent GHRH analog specifically studied for its effects on visceral adipose tissue. Its primary mechanism is the stimulation of GH production. | While primarily used for metabolic benefits, its action on the GHRH receptor inherently supports the neurophysiological processes that initiate and maintain deep sleep. |
| MK-677 (Ibutamoren) | An orally active, non-peptide GHS that mimics the action of ghrelin. It stimulates the release of GH and IGF-1. | Studies have shown it can increase the duration of REM sleep and improve overall sleep quality, particularly in older adults. |
Targeted peptide therapies can recalibrate the somatotropic axis, directly enhancing the deep, slow-wave sleep that is essential for physical and neurological restoration.
The clinical application of these peptides represents a sophisticated approach to sleep medicine. By directly targeting the GHRH receptor and the ghrelin receptor, these therapies can bypass some of the complexities of HPA axis dysregulation and directly promote the deep sleep that is often most deficient in individuals with hormonal imbalances.
The resulting improvement in SWS not only enhances feelings of restfulness but also creates the optimal physiological environment for the body’s own repair and regeneration processes, leading to widespread benefits in metabolic health, cognitive function, and overall vitality. This demonstrates a paradigm where sleep is not merely a passive state of rest, but an active, hormone-driven process of restoration that can be precisely supported through advanced clinical interventions.
References
- Andersen, M. L. Tufik, S. (2006). The effects of testosterone on sleep and sleep-disordered breathing in men ∞ a review. Sleep Medicine Reviews, 10 (1), 29-40.
- Brandenberger, G. Weibel, L. (2004). The 24-h growth hormone rhythm in men ∞ sleep and circadian influences. Journal of Sleep Research, 13 (4), 251-255.
- Freedman, R. R. (2014). Menopausal hot flashes ∞ mechanisms, endocrinology, treatment. The Journal of Steroid Biochemistry and Molecular Biology, 142, 115-120.
- Caufriez, A. Leproult, R. L’Hermite-Balériaux, M. Kerkhofs, M. Copinschi, G. (2011). Progesterone and sleep ∞ a clinical review. Neuroendocrinology, 94 (1), 1-10.
- Copinschi, G. (2005). Hormones and sleep. Annales d’Endocrinologie, 66 (2), 137-142.
- Hale, G. E. Zhao, X. Hughes, C. L. Burger, H. G. Robertson, D. M. Fraser, I. S. (2010). Endocrine features of menstrual cycles in middle and late reproductive age and the menopausal transition. The Journal of Clinical Endocrinology & Metabolism, 95 (3), 1209-1217.
- Luboshitzky, R. Aviv, A. Hefetz, A. Herer, P. Shen-Orr, Z. Lavie, P. (2000). Decreased nocturnal melatonin secretion in English men with hypogonadism. The Journal of Clinical Endocrinology & Metabolism, 85 (5), 1833-1836.
- Pinto, O. C. Jr. Tufik, S. Andersen, M. L. (2016). The effects of testosterone on sleep and sleep-disordered breathing in men ∞ a systematic review and meta-analysis. Sleep Medicine Reviews, 27, 31-40.
- Schüssler, P. Kluge, M. Yassouridis, A. Dresler, M. Held, K. Zihl, J. Steiger, A. (2008). Growth hormone secretion is associated with slow-wave sleep in patients with major depression. Psychoneuroendocrinology, 33 (9), 1205-1214.
- Van Cauter, E. Leproult, R. Plat, L. (2000). Age-related and gender-related changes in 24-hour growth hormone secretion in healthy adults ∞ relationships with deep sleep and insulin-like growth factor I levels. Sleep, 23 Suppl 4, S201-S205.

Reflection

Charting Your Own Biological Course
The information presented here offers a map of the intricate biological terrain that connects your internal chemistry to your nightly rest. You have seen how the subtle shifts in hormones across your life can profoundly reshape your experience of sleep, turning what should be a period of restoration into a source of frustration.
This knowledge is a powerful tool, moving you from a position of passive suffering to one of active understanding. It provides a framework for interpreting your body’s signals, allowing you to see symptoms not as random failings but as logical consequences of physiological change.
Your personal health story is written in your unique biology. The way your body navigates the transitions of puberty, perimenopause, or andropause is specific to you. While the general principles of endocrinology apply to everyone, the expression of these principles is highly individual.
The next step in this process involves looking inward, armed with this new perspective. Consider the patterns of your own life. How has your sleep evolved over the years? Do the descriptions of these hormonal shifts resonate with your own lived experience? This self-reflection is the beginning of a more personalized approach to your well-being.
Ultimately, this understanding is designed to be a catalyst for conversation and action. The goal is to move beyond simply coping with poor sleep and toward proactively managing your health.
The path to reclaiming your vitality begins with this foundational knowledge, but its true power is realized when it is applied to your unique circumstances, ideally in partnership with a guide who can help you navigate the complexities of your own endocrine system. Your journey to better sleep and optimal function is yours to direct.



