

Fundamentals
You know the feeling. It is a quiet exhaustion that settles deep in your bones, a sense of running on a low battery that no amount of sleep seems to fully recharge.
It can manifest as a subtle fogginess that clouds your thoughts, a frustrating inability to lose weight despite your best efforts, or a general feeling that your body’s internal engine is idling instead of running smoothly. This lived experience, this deeply personal sense of diminished vitality, is a valid and important signal from your body.
It is the starting point of a crucial investigation into your own biological systems. Understanding the intricate communication network within your endocrine system provides the map for this investigation, showing how two of its most powerful players ∞ the thyroid and growth hormone axes ∞ are in constant dialogue, shaping your daily energy, clarity, and overall well-being.
Your body’s metabolic rate, the speed at which it performs the chemical processes necessary for life, is governed by a small, butterfly-shaped gland at the base of your neck ∞ the thyroid. Think of it as the control center for your body’s energy economy.
This gland produces hormones that travel to nearly every cell, instructing them on how much energy to burn. The entire operation is managed by a precise feedback loop known as the Hypothalamic-Pituitary-Thyroid (HPT) axis. It begins in the brain, where the hypothalamus releases Thyrotropin-Releasing Hormone (TRH).
This signals the pituitary gland to release Thyroid-Stimulating Hormone (TSH). TSH then travels to the thyroid gland and instructs it to produce its hormones, primarily Thyroxine (T4) and, to a lesser extent, Triiodothyronine (T3).
T4 is the primary output of the thyroid gland. It is a prohormone, a stable, abundant storage molecule that circulates throughout your bloodstream. On its own, T4 has very little biological activity. Its purpose is to be a readily available reservoir, waiting for the signal to become active.
The real metabolic powerhouse is T3. This is the active form of thyroid hormone, the molecule that binds to receptors inside your cells and directly stimulates your metabolism, influencing everything from your heart rate and body temperature to your ability to synthesize proteins and break down fats.
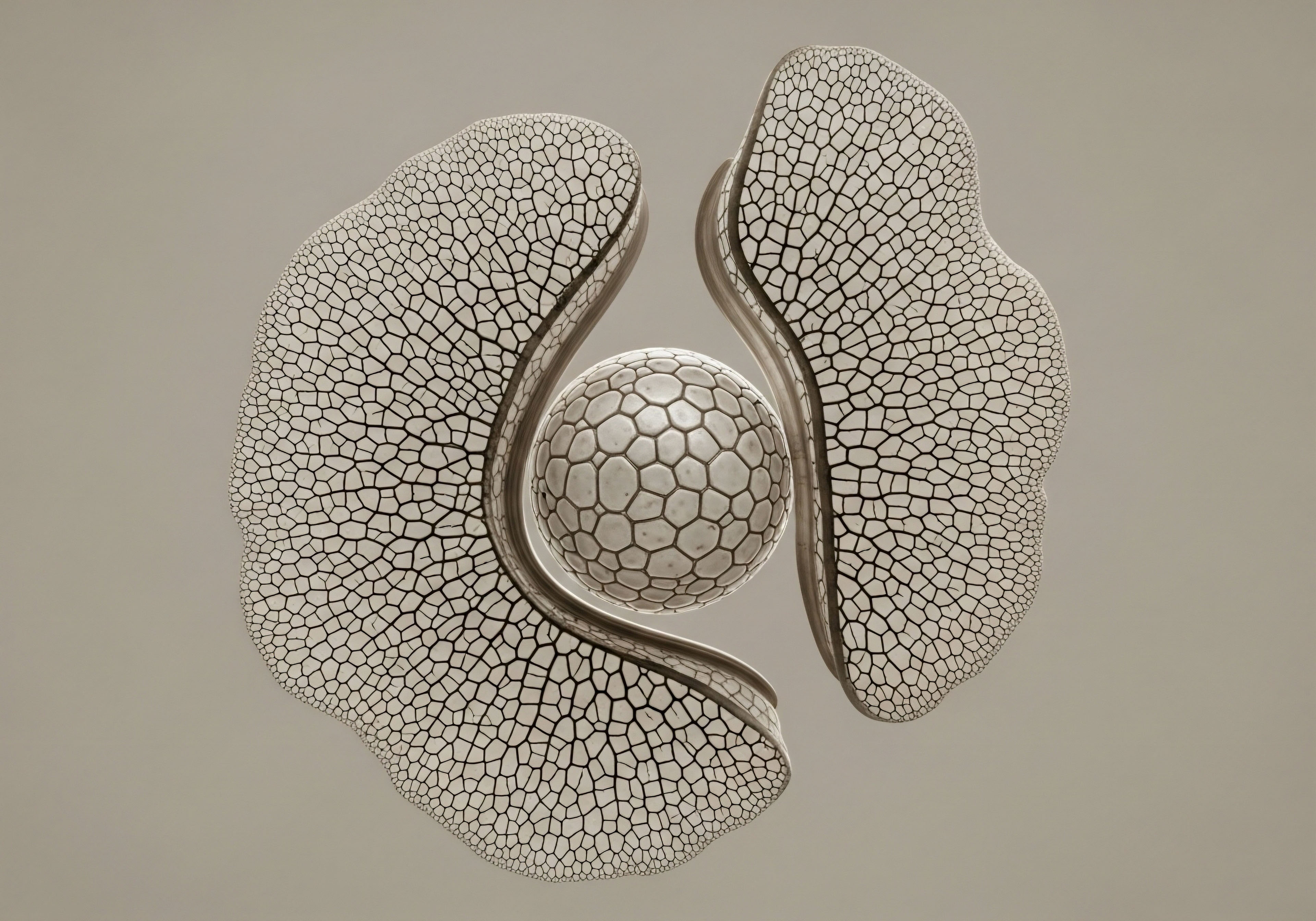
The conversion from the inactive T4 to the active T3 is perhaps the most critical, and often overlooked, step in this entire process. This activation does not happen randomly; it is a highly regulated process carried out by a specific family of enzymes called deiodinases.
The conversion of the storage thyroid hormone T4 into the active thyroid hormone T3 is a critical metabolic event controlled by specialized deiodinase enzymes.

The Deiodinase Enzymes the Body’s Metabolic Gatekeepers
The deiodinase enzymes are the unsung heroes of thyroid function. They are responsible for the precise, tissue-specific activation and deactivation of thyroid hormone, ensuring that each part of your body gets the exact amount of metabolic stimulation it needs. There are three main types, each with a distinct role.
- Type 1 Deiodinase (D1) ∞ Found primarily in the liver, kidneys, and thyroid gland, D1 is responsible for converting T4 to T3 and releasing it into the general circulation. It acts as a major contributor to the pool of active T3 available to your entire body. It also plays a housekeeping role by clearing out used or unwanted thyroid hormone metabolites.
- Type 2 Deiodinase (D2) ∞ This is arguably the most important enzyme for local thyroid regulation. D2 is found in the brain, the pituitary gland, brown adipose tissue, and skeletal muscle. Its primary job is to convert T4 to T3 for immediate use within that specific cell or tissue. When your brain cells need more energy for focus, D2 provides it. When your pituitary needs to sense thyroid levels to adjust TSH production, D2 makes that possible. It is the key to cellular-level metabolic fine-tuning.
- Type 3 Deiodinase (D3) ∞ This enzyme performs the opposite function. D3 is the primary inactivator of thyroid hormone. It converts T4 into an inactive metabolite called reverse T3 (rT3), and it also breaks down the active T3 into an inactive form. This is a protective mechanism, preventing tissues from becoming overstimulated, particularly during times of stress or illness. High levels of rT3 can act as a brake on the system, competing with T3 for receptor binding sites without activating them.
Understanding this conversion process is fundamental. You can have a lab report showing a perfectly normal TSH and T4 level, yet still experience all the symptoms of low thyroid function. This is often because the conversion of T4 to T3 is being impaired, or too much T3 is being inactivated into rT3. The system appears fine on the surface, but at the cellular level, the active hormone is simply not available where it is needed most.

The Axis of Repair and Rejuvenation
Running parallel to the HPT axis is another critical endocrine pathway ∞ the Hypothalamic-Pituitary-Growth Hormone (HPGH) axis. This system is centered on Growth Hormone (GH), a powerful peptide hormone produced by the pituitary gland. While its name suggests a primary role in childhood growth, its functions in adulthood are profoundly important for maintaining metabolic health, body composition, and tissue repair.
Similar to the thyroid axis, it operates on a feedback loop. The hypothalamus releases Growth Hormone-Releasing Hormone (GHRH), which stimulates the pituitary to release GH. GH then travels through the body, exerting some effects directly and others by stimulating the liver to produce Insulin-Like Growth Factor 1 (IGF-1), which is responsible for many of GH’s anabolic, or tissue-building, effects.
In adults, a healthy level of GH is associated with:
- Improved Body Composition ∞ GH helps to stimulate the breakdown of fat (lipolysis) and promote the synthesis of protein in muscle tissue.
- Enhanced Tissue Repair ∞ It plays a vital role in healing and regeneration of connective tissues, bones, and muscles.
- Metabolic Regulation ∞ GH has complex effects on blood sugar and insulin sensitivity, contributing to overall metabolic balance.
- Better Sleep Quality ∞ The largest pulse of GH is released during deep, slow-wave sleep, and it is integral to the restorative processes that occur during rest.
As we age, the natural production of GH declines. This decline is linked to many of the signs we associate with aging, such as increased body fat, decreased muscle mass, slower recovery from injury, and diminished energy.
This is why therapies designed to support or restore the body’s natural GH pulse, such as those using peptides like Sermorelin or Ipamorelin, are a cornerstone of personalized wellness and longevity protocols. These two powerful axes, one governing moment-to-moment metabolic rate and the other overseeing long-term repair and composition, do not operate in isolation. They are deeply interconnected, and the nature of their interaction holds a key to understanding how we can reclaim our vitality.


Intermediate
The connection between the growth hormone and thyroid axes is a beautiful example of the body’s integrated physiology. The relationship is centered on the critical process of thyroid hormone activation. Clinical observations and research have consistently shown that administering growth hormone can alter the balance of thyroid hormones in the body.
Specifically, GH therapy often leads to a decrease in circulating T4 levels while simultaneously increasing the levels of the active T3 hormone. This points directly to an influence on the deiodinase enzymes. The evidence strongly suggests that growth hormone acts as a potent stimulator of the Type 2 Deiodinase (D2) enzyme. By enhancing D2 activity, GH effectively accelerates the conversion of the inactive T4 prohormone into the metabolically powerful T3 hormone, primarily within peripheral tissues like the liver and muscle.
This interaction has profound clinical significance. For an individual whose lab results show adequate T4 but low T3, a condition that often leaves them symptomatic despite “normal” thyroid panels, supporting the GH axis could be a missing piece of the puzzle.
By upregulating D2, the body becomes more efficient at activating the thyroid hormone it already has, potentially alleviating symptoms of fatigue, brain fog, and a sluggish metabolism. This mechanism explains why individuals starting on a growth hormone peptide protocol often report an increase in energy and an improved sense of well-being that feels distinct from the direct effects of GH itself; they are experiencing the downstream benefit of enhanced cellular thyroid function.

What Is the Clinical Impact on Thyroid Health?
The stimulation of T4 to T3 conversion by growth hormone is a double-edged sword, and its impact depends entirely on the individual’s underlying thyroid health. This is where a nuanced, personalized approach becomes essential. One of the most important clinical phenomena to be aware of is the potential for GH therapy to “unmask” a pre-existing, undiagnosed case of central hypothyroidism.
Central hypothyroidism is a condition where the pituitary gland fails to produce enough TSH to properly stimulate the thyroid. In someone with a concurrent growth hormone deficiency, the entire metabolic system is slowed down, including the clearance of T4. Their T4 levels might therefore appear to be in the low-normal range, masking the underlying pituitary issue.
When this person begins GH peptide therapy, the sudden increase in D2 activity accelerates the conversion of their limited T4 into T3. This increased conversion rate, combined with a faster clearance of T4, can cause their T4 levels to drop significantly, revealing the previously hidden deficiency. This is why careful monitoring of thyroid labs ∞ including TSH, free T4, and free T3 ∞ is a mandatory part of any responsible hormone optimization protocol that includes GH peptides.
Growth hormone peptide therapy can reveal a hidden thyroid inefficiency by accelerating the use of available T4, making comprehensive lab monitoring essential.

Growth Hormone Peptides a Comparative Overview
Modern protocols rarely use direct recombinant human growth hormone (rhGH) due to its cost, side effects, and disruption of the body’s natural feedback loops. Instead, they utilize specific peptides that work by stimulating the body’s own pituitary gland to produce and release GH in a manner that respects the natural pulsatile rhythm. This approach is generally safer and more sustainable. The most common peptides used have distinct mechanisms and characteristics.
| Peptide Protocol | Mechanism of Action | Primary Clinical Application | Potential Influence on Thyroid Conversion |
|---|---|---|---|
| Sermorelin | A GHRH analogue. It directly stimulates the GHRH receptor on the pituitary to produce and release growth hormone. It is a foundational and well-studied peptide. | General anti-aging, improved sleep quality, and enhanced recovery. Often used as a starting point for GH optimization. | By increasing the natural pulse of GH, it is expected to gently upregulate D2 activity, potentially improving T4 to T3 conversion over time. |
| Ipamorelin / CJC-1295 | A powerful combination. CJC-1295 is a GHRH analogue that provides a steady signal, while Ipamorelin is a GH secretagogue that also blocks somatostatin (the hormone that inhibits GH release). | Potent effects on muscle gain, fat loss, and deep sleep. Considered a more advanced protocol for significant changes in body composition. | This combination produces a strong and sustained GH pulse, which would likely lead to a more pronounced stimulation of D2 and a more noticeable shift in the T4/T3 ratio. |
| Tesamorelin | A highly stable and potent GHRH analogue. It is specifically studied and approved for the reduction of visceral adipose tissue (VAT), the dangerous fat around the organs. | Targeted fat loss, particularly visceral fat. Often used for individuals with metabolic syndrome or lipodystrophy. | Its powerful effect on GH release suggests a strong corresponding effect on D2-mediated T4 to T3 conversion, contributing to its metabolic benefits. |
| MK-677 (Ibutamoren) | An oral ghrelin mimetic. It stimulates GH release by activating the ghrelin receptor in the brain, leading to significant and sustained increases in both GH and IGF-1. | Convenient oral administration for increasing GH/IGF-1 levels, muscle building, and improving sleep. | Due to its sustained, non-pulsatile stimulation, it can cause a very significant increase in D2 activity. This can also lead to side effects like insulin resistance and water retention, requiring careful monitoring. |
The choice of peptide depends on the individual’s specific goals, health status, and lab results. For someone primarily concerned with sleep and general wellness, Sermorelin might be appropriate. For an athlete seeking performance and body composition changes, the Ipamorelin/CJC-1295 combination is often preferred.
Regardless of the choice, the underlying principle remains the same ∞ by stimulating the body’s own GH production, these peptides initiate a cascade of effects that includes the enhanced conversion of T4 to T3. This makes the integration of thyroid and growth hormone optimization a powerful strategy for achieving a higher level of metabolic function and overall vitality.


Academic
The modulatory effect of growth hormone on thyroid hormone homeostasis is a sophisticated biological process rooted in the transcriptional regulation of iodothyronine deiodinase genes. The observed decrease in serum thyroxine (T4) and concomitant increase in triiodothyronine (T3) following GH administration is not a passive event but an active, targeted upregulation of enzymatic machinery.
The central mechanism involves the direct influence of GH on the expression and activity of Type 2 Deiodinase (DIO2), the enzyme responsible for the intracellular conversion of T4 to the biologically active T3.
In vitro studies using human cell lines, such as hepatoblastoma-derived HepG2 and thyroid carcinoma-derived HTC/C3, have demonstrated that recombinant human growth hormone (rhGH) administration significantly increases the messenger RNA (mRNA) expression of the DIO2 gene. This increase in gene transcription is followed by a corresponding increase in D2 protein synthesis and enzymatic activity, providing a clear molecular basis for the observed shifts in circulating thyroid hormone levels.
This regulation appears to be a direct effect of GH on its target cells. The GH receptor, a member of the cytokine receptor superfamily, does not possess intrinsic kinase activity. Upon GH binding, it dimerizes and recruits Janus Kinase 2 (JAK2), which then autophosphorylates and phosphorylates the intracellular domain of the GH receptor.
This creates docking sites for Signal Transducer and Activator of Transcription (STAT) proteins, particularly STAT5. The phosphorylated STAT proteins then translocate to the nucleus, where they bind to specific DNA sequences in the promoter regions of target genes.
It is through this JAK/STAT pathway that GH is believed to exert its transcriptional control over the DIO2 gene, effectively instructing the cell to produce more of the T4-to-T3 converting enzyme. While Insulin-Like Growth Factor 1 (IGF-1) mediates many of GH’s anabolic effects, the stimulation of deiodinase activity appears to be a more direct GH action, particularly in hepatocytes, which express abundant GH receptors but have few functional IGF-1 receptors.

How Does Tissue Specificity Affect This Interaction?
The physiological impact of this regulatory relationship is highly dependent on its tissue-specific nature. The deiodinase enzymes are not uniformly distributed throughout the body; their expression is compartmentalized to allow for precise local control of thyroid hormone signaling. This is a critical concept in endocrinology, moving beyond simple measurements of circulating hormones to understand their action at the point of impact. GH’s ability to influence this local control system has significant metabolic implications.
| Deiodinase Enzyme | Primary Location(s) | Primary Function | Regulation by Growth Hormone Axis |
|---|---|---|---|
| Type 1 (D1) | Liver, Kidneys, Thyroid | Contributes to circulating T3 pool; clears rT3. | Activity appears to be less directly affected by GH compared to D2. Some studies suggest minor upregulation, but D2 is the primary driver of the T4/T3 shift. |
| Type 2 (D2) | Brain, Pituitary, Skeletal Muscle, Brown Adipose Tissue | Intracellular conversion of T4 to T3 for local use. Critical for negative feedback in the HPT axis. | Strongly upregulated by GH at the transcriptional level via the JAK/STAT pathway. This is the core mechanism of GH’s effect on thyroid conversion. |
| Type 3 (D3) | Placenta, Fetal Tissues, Skin, Brain | Inactivates T4 to rT3 and T3 to T2, acting as a protective brake on thyroid signaling. | GH appears to downregulate or have minimal effect on D3. By upregulating D2 and not D3, GH creates a strong net shift towards T3 activation rather than inactivation. |
The upregulation of D2 in skeletal muscle, for instance, means that GH can directly enhance the metabolic rate and protein synthesis capacity of muscle tissue by increasing local T3 availability. In the pituitary gland, increased D2 activity is essential for the thyrotroph cells to accurately sense circulating T4 levels and adjust TSH secretion accordingly, forming a key part of the negative feedback loop.
The reduction in reverse T3 (rT3) often seen with GH therapy is also a direct consequence of this enzymatic shift. By preferentially shunting T4 down the D2 activation pathway, less substrate is available for the D3 pathway to produce the inactive rT3. This dual action ∞ increasing active T3 while decreasing the inhibitory rT3 ∞ results in a powerful amplification of thyroid hormone signaling at the cellular level.
Growth hormone’s primary influence is the transcriptional upregulation of the DIO2 gene, leading to greater local T3 availability in key metabolic tissues.

What Are the Implications for Advanced Protocols?
This detailed understanding informs the strategic application of advanced hormonal optimization protocols. The choice of a GH-stimulating peptide can be tailored based on the desired magnitude of effect on thyroid conversion.
For example, the potent and sustained GH release from a peptide like MK-677 would be expected to produce a more dramatic and sustained increase in D2 activity compared to the more physiological, pulsatile release from Sermorelin. This could be advantageous for an individual with significant T4-to-T3 conversion issues but would require vigilant monitoring for potential side effects, including the possibility of inducing subclinical hyperthyroidism at the tissue level if not carefully managed.
Furthermore, the interplay between these axes highlights the limitations of assessing thyroid status with TSH alone. A patient on a GH peptide protocol might exhibit a suppressed TSH. A conventional interpretation might view this as a sign of impending hyperthyroidism. However, in this context, it could represent an appropriate physiological response.
The enhanced D2 activity in the pituitary, driven by GH, increases local T3 production, which then signals to the hypothalamus and pituitary to downregulate TRH and TSH release. The system is simply recalibrating to a new, more efficient state of thyroid hormone conversion.
Therefore, a comprehensive panel that includes free T4, free T3, and reverse T3 is indispensable for accurately interpreting the metabolic status of an individual undergoing such a protocol. The goal of these integrated therapies is to restore a dynamic and responsive endocrine network, and that requires looking beyond single markers to appreciate the system’s interconnected biology.
References
- Yamauchi, I. et al. “Effects of growth hormone on thyroid function are mediated by type 2 iodothyronine deiodinase in humans.” Endocrine, vol. 59, no. 2, 2018, pp. 353-363.
- Stochmal, E. et al. “Thyroid Hormone Changes Related to Growth Hormone Therapy in Growth Hormone Deficient Patients.” Journal of Clinical Medicine, vol. 10, no. 22, 2021, p. 5434.
- Gereben, B. et al. “Cellular and molecular basis of deiodinase-regulated thyroid hormone signaling.” Endocrine Reviews, vol. 29, no. 7, 2008, pp. 898-938.
- Jørgensen, J. O. et al. “Growth hormone-dependent changes in serum thyroxine and 3,5,3′-triiodothyronine in patients with growth hormone deficiency.” The Journal of Clinical Endocrinology & Metabolism, vol. 69, no. 3, 1989, pp. 675-678.
- Porazzi, E. et al. “Growth hormone regulates deiodinase type 2 and 3 expression in the developing chicken.” The Journal of Endocrinology, vol. 202, no. 3, 2009, pp. 385-392.

Reflection
You have now seen the elegant biological machinery that connects the systems of repair with the systems of energy. You understand that the fatigue or mental fog you may feel is not a personal failing but a potential signal from a complex, interconnected network.
The science shows how a peptide that stimulates one hormone can awaken the function of another, illustrating a fundamental principle of your body’s physiology ∞ no system works in isolation. This knowledge is the first, most critical step. It transforms you from a passive passenger to an informed pilot of your own health.
The path forward involves looking at your own unique biology, your specific lab markers, and your personal experience. The ultimate goal is a protocol tailored not to a textbook but to you, recalibrating your systems to restore the vitality and function that is your birthright.

Glossary

growth hormone

pituitary gland

thyroid hormone

deiodinase enzymes

thyroid function

type 2 deiodinase

reverse t3

body composition

hpt axis

metabolic regulation

ipamorelin

sermorelin

peptide protocol

central hypothyroidism

t4 to t3 conversion

recombinant human growth hormone

thyroid hormone signaling

thyroid conversion




