

Fundamentals

Your Biology Is Your Story
You have followed the protocol. You have been consistent with your weekly testosterone cypionate injections, managed your ancillaries like anastrozole and gonadorelin, and tracked your numbers. Yet, the results are not what you anticipated. Perhaps the fatigue lingers, the mental fog has not cleared, or the physical changes are less pronounced than expected.
This experience can be profoundly disheartening. It often leads to a cycle of questioning the treatment, the protocol, or even your own commitment. Your body’s response, or lack thereof, is a critical data point. It is the beginning of a deeper inquiry into your unique biological landscape. The source of this variability often lies within your genetic code, the fundamental instruction manual that dictates how your body utilizes hormones.
Understanding this biological individuality is the first step toward reclaiming your vitality. Hormonal optimization is a process of recalibrating a complex system. Your genetic makeup is a primary determinant of how that system is wired. The efficacy of any hormonal protocol is deeply personal, written in the language of your DNA.
When a standard approach yields a suboptimal outcome, it presents an opportunity to look more closely at the underlying mechanics of your personal endocrine system. This exploration moves you from a passive recipient of a protocol to an active participant in your own health restoration.

The Genetic Blueprint for Hormonal Health
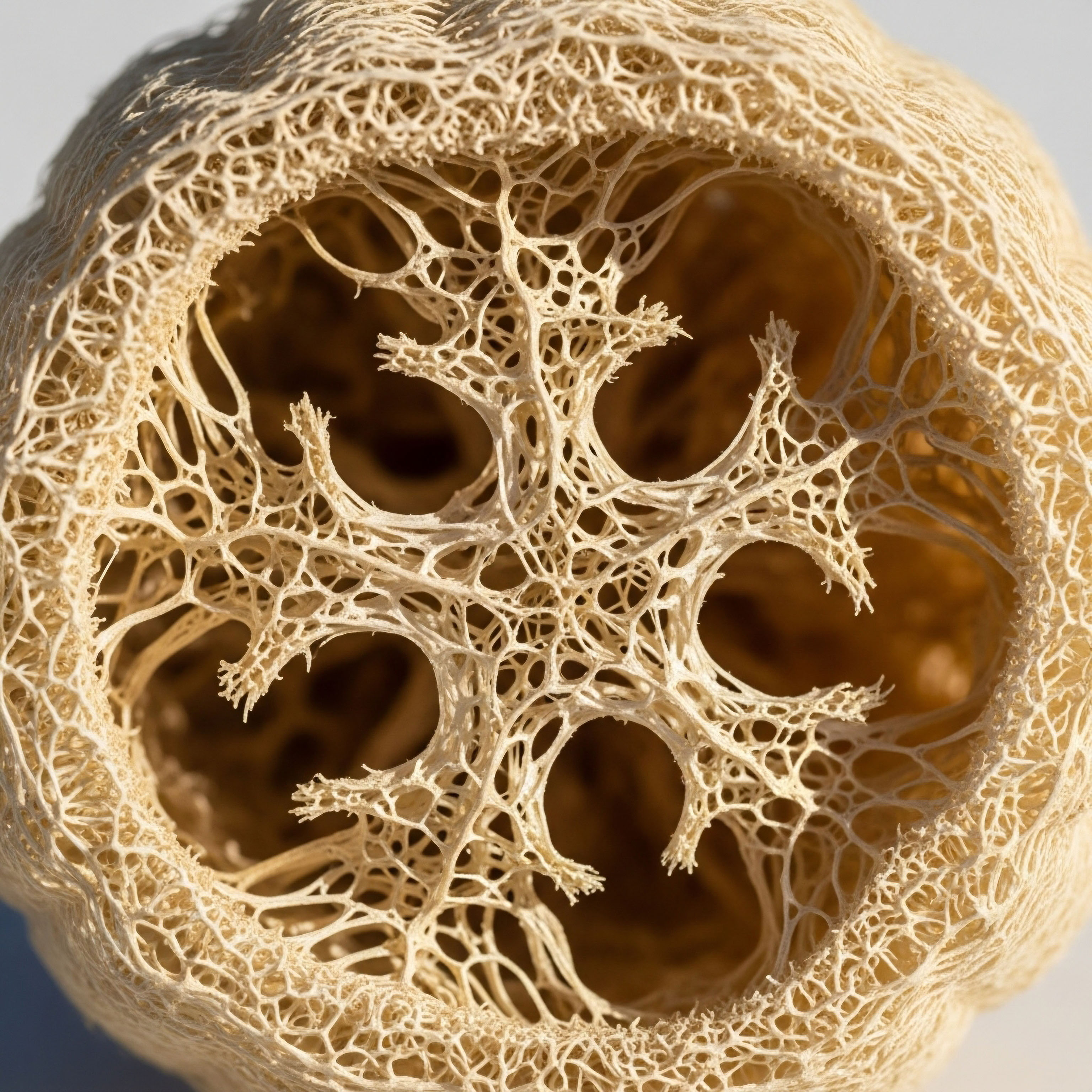
At the heart of your body’s response to testosterone replacement therapy (TRT) is a field of study called pharmacogenomics. This discipline examines how your specific genetic variations influence your reaction to medications and hormones. Your DNA contains genes that act as blueprints for creating proteins. These proteins are the functional machinery of your cells.
They include receptors that hormones bind to, enzymes that convert hormones from one form to another, and carrier molecules that transport hormones through your bloodstream. Small, common variations in these genes, known as single nucleotide polymorphisms (SNPs), can significantly alter the structure and function of these crucial proteins.
Think of your endocrine system as a highly sophisticated communication network. Testosterone is a key messenger molecule. For its message to be received and acted upon, several components must work in concert:
- The Messenger Molecule ∞ This is the testosterone administered through your TRT protocol. Its dosage and delivery method are the inputs into the system.
- The Transport System ∞ Once in the bloodstream, testosterone must be transported to target tissues. A protein called Sex Hormone-Binding Globulin (SHBG) is the primary transport vehicle. Your genetics determine how much SHBG you produce and how tightly it binds to testosterone.
- The Receiving Dock ∞ At the target cell, testosterone must bind to a specific receiving dock, the Androgen Receptor (AR). The sensitivity of this receptor is genetically determined and dictates how strong a signal the cell receives from a given amount of testosterone.
- The Metabolic Converters ∞ Your body converts testosterone into other important hormones. The enzyme aromatase converts testosterone into estrogen, while the enzyme 5-alpha reductase converts it into dihydrotestosterone (DHT). Genetic variations in the genes for these enzymes dictate the rate of these conversions, profoundly affecting your hormonal balance and potential side effects.
A variation in any one of these genetic components can change the outcome of the entire protocol. This is why a “one-size-fits-all” approach to hormonal optimization is often insufficient. Your lived experience of symptoms and your response to therapy are direct reflections of this intricate, genetically-guided biological reality.
Your genetic code provides the underlying reason why a standardized TRT protocol may require significant personalization to achieve optimal results.

Why Standard Lab Values Are Only Part of the Picture
A common point of frustration is seeing “normal” or even “optimal” testosterone levels on a lab report while still experiencing symptoms of hormonal imbalance. This is where understanding your genetic predispositions becomes invaluable. Your total testosterone level is a measure of the messenger molecules in your bloodstream, but it does not tell the whole story. The critical information lies in how your body is ableto use that testosterone.
For instance, you might have genetically elevated levels of SHBG. This protein will bind a larger portion of your circulating testosterone, leaving less “free” or bioavailable testosterone to interact with your cells. Your total testosterone may appear robust, but your tissues are effectively starved of the hormone.
Conversely, someone with genetically low SHBG might have lower total testosterone but feel excellent because a larger percentage is free and active. Similarly, your androgen receptor sensitivity plays a decisive role. If your receptors are genetically less sensitive, you will require higher levels of free testosterone to achieve the same physiological effect as someone with highly sensitive receptors.
Your body is not a simple container for hormones; it is an active, dynamic system that processes them according to a unique genetic script. This is why a truly personalized wellness protocol must look beyond standard lab ranges and consider the functional context provided by your genetic makeup.


Intermediate

The Key Genetic Players in TRT Protocols
When we move from the conceptual to the clinical, we can identify specific genes whose variations are known to have a direct and measurable impact on the outcomes of testosterone replacement therapy. Understanding these genetic modulators allows for a more refined approach to protocol design, moving beyond simple dose adjustments to a more sophisticated biochemical recalibration.
For men undergoing TRT with testosterone cypionate, and for women on low-dose testosterone protocols, these genetic factors can explain the wide variance in individual responses and side effect profiles.
The primary genes of interest form a core panel for understanding an individual’s androgenic system. These are not rare mutations but common polymorphisms that exist across the population. Their influence is a matter of degree, creating a spectrum of responses.
A clinician informed by this genetic data can better anticipate a patient’s needs, whether it involves adjusting the dose of testosterone, modifying the frequency of anastrozole to manage estrogen conversion, or simply understanding why a patient’s subjective feedback differs from their lab results.
Genetic variations in the Androgen Receptor, Aromatase, and SHBG genes are the principal drivers of individualized responses to testosterone therapy.

The Androgen Receptor (AR) Gene and Testosterone Sensitivity
The Androgen Receptor (AR) is the direct target for testosterone and DHT. The gene that codes for this receptor contains a specific repeating DNA sequence known as the CAG repeat. The number of these repeats varies among individuals and directly influences the receptor’s sensitivity. This genetic feature is one of the most significant determinants of how your body experiences the effects of androgens.
- Shorter CAG Repeats (e.g. less than 21) ∞ These are associated with a more sensitive androgen receptor. The receptor is more efficient at initiating a cellular response when testosterone binds to it. Individuals with shorter repeats may experience more significant effects from a given dose of testosterone. They might see more substantial increases in muscle mass, libido, and erythropoiesis (red blood cell production). This heightened sensitivity can also mean a greater risk for androgenic side effects like acne, hair loss, and an exaggerated increase in hematocrit, requiring careful monitoring.
- Longer CAG Repeats (e.g. more than 24) ∞ These are linked to a less sensitive or more resistant androgen receptor. The receptor requires a stronger signal, meaning higher levels of free testosterone, to produce the same cellular response. A person with longer CAG repeats might find that standard TRT doses are insufficient to resolve their symptoms of low testosterone. They may report feeling little to no benefit despite having lab values in the optimal range. For these individuals, achieving a therapeutic effect may require targeting higher-than-average free testosterone levels.
This genetic variation explains why two men with identical free testosterone levels can have vastly different clinical outcomes. The man with 20 CAG repeats may feel fantastic, while the man with 26 repeats may still feel hypogonadal. Knowledge of the AR-CAG repeat length provides critical context for interpreting both lab results and patient-reported outcomes, allowing for more precise therapeutic targeting.

How Does AR CAG Repeat Length Affect TRT Management?
The clinical implications of AR-CAG repeat length are significant for tailoring hormonal optimization protocols. For a man on a standard TRT protocol (e.g. weekly testosterone cypionate injections), this genetic information can guide dosing and monitoring strategies.
For example, a patient with a short CAG repeat length may be more susceptible to polycythemia (an overproduction of red blood cells), a known side effect of TRT. A clinician aware of this predisposition would monitor hematocrit levels more frequently and might opt for a more conservative starting dose.
Conversely, for a patient with a long CAG repeat length who is not responding to a standard dose, this genetic data provides a clear biological rationale for carefully titrating the dose upwards to achieve a therapeutic effect, rather than dismissing the patient’s subjective experience.

The Aromatase (CYP19A1) Gene and Estrogen Conversion
Testosterone does not act in isolation. A portion of it is converted into estradiol, a potent form of estrogen, by the enzyme aromatase. The gene that codes for this enzyme is CYP19A1. Genetic polymorphisms in CYP19A1 can significantly alter the activity of the aromatase enzyme, leading to either increased or decreased conversion of testosterone to estrogen. This balance is critical for both men and women, and its genetic regulation is a key factor in managing the side effects of TRT.
On a typical male TRT protocol, anastrozole is often prescribed to inhibit the aromatase enzyme and prevent excessive estrogen levels. However, the need for and dosage of anastrozole are highly dependent on an individual’s genetic predisposition for aromatization.
The following table outlines how different CYP19A1 variations can impact TRT protocols:
| CYP19A1 Genetic Profile | Enzyme Activity | Impact on TRT | Clinical Considerations |
|---|---|---|---|
| High-Activity Variants | Increased conversion of testosterone to estradiol. | Patients are more likely to experience high-estrogen side effects like water retention, gynecomastia, mood swings, and decreased libido, even on moderate TRT doses. | These individuals may require more aggressive aromatase inhibition with anastrozole. Prophylactic use of anastrozole from the start of therapy may be warranted. |
| Low-Activity Variants | Decreased conversion of testosterone to estradiol. | Patients are less likely to develop high estrogen levels and may be at risk for symptoms of low estrogen if an aromatase inhibitor is used inappropriately. | These individuals may not need anastrozole at all, or may only require a very small dose. Over-suppression of estrogen can lead to joint pain, low libido, and poor lipid profiles. |

The SHBG Gene and Bioavailable Testosterone
Sex Hormone-Binding Globulin (SHBG) is the primary protein responsible for transporting testosterone in the blood. Only testosterone that is not bound to SHBG (or weakly bound to albumin) is considered “free” or bioavailable and can exert its effects on target tissues. The gene that codes for SHBG has several well-documented polymorphisms that influence the circulating levels of the SHBG protein. These genetic variations are a major determinant of your free testosterone percentage.
The table below details the influence of common SHBG gene variants:
| SHBG Gene Variant (SNP) | Effect on SHBG Levels | Impact on Free Testosterone | Clinical Implications for TRT |
|---|---|---|---|
| rs1799941 (A-allele) | Increased SHBG production. | Lower percentage of free testosterone for a given total testosterone level. | Patients may require higher total testosterone levels to achieve a therapeutic free testosterone concentration. Lab results showing high-normal total T may be misleading if free T is low. |
| rs6258 (G-allele) | Decreased SHBG production. | Higher percentage of free testosterone for a given total testosterone level. | Patients may feel the effects of TRT at lower total testosterone levels. They may also be more sensitive to dose changes. |
| rs6259 (A-allele) | Increased SHBG production and binding affinity. | Lower percentage of free testosterone. | Similar to rs1799941, these individuals often need their protocols optimized based on free testosterone levels rather than total testosterone. |
Understanding a patient’s genetic predisposition for SHBG production is fundamental to interpreting their lab work correctly. It explains why some individuals can have a total testosterone of 600 ng/dL and feel symptomatic, while others feel optimal at the same level. The genetic data provides a framework for personalizing therapy to achieve an optimal level of bioavailable hormone, which is the ultimate therapeutic goal.


Academic

A Systems Biology View of Androgen Pharmacogenomics
The clinical response to testosterone replacement therapy is a complex polygenic trait. A reductionist view focusing on a single gene polymorphism is insufficient to predict the full spectrum of therapeutic outcomes and adverse effects. A more sophisticated, systems-biology approach is required, one that integrates the distinct yet interconnected pathways of androgen transport, metabolism, and signaling.
The individual genetic variations within the AR, CYP19A1, and SHBG genes do not operate in isolation. They create a combinatorial genetic landscape that defines an individual’s unique “androgen network.” The net effect of TRT is the emergent property of the interactions within this network.
For example, an individual with a long AR-CAG repeat (low receptor sensitivity) who also possesses a high-activity CYP19A1 variant (rapid estrogen conversion) presents a particularly challenging clinical scenario. The administered testosterone is less effective at the receptor site and is simultaneously being shunted away from the androgenic pathway towards the estrogenic pathway.
This patient is likely to experience minimal therapeutic benefit from testosterone while being highly susceptible to estrogenic side effects. A standard protocol for such an individual would likely fail, highlighting the necessity of a multi-gene analytical approach to truly personalize therapy.
The interplay between genetic polymorphisms in androgen transport, metabolism, and receptor sensitivity creates a combinatorial matrix that dictates the ultimate clinical phenotype of a TRT patient.

The Molecular Basis of Androgen Receptor Polymorphism
The polymorphism in exon 1 of the androgen receptor gene, specifically the variable length of the polyglutamine tract encoded by the CAG trinucleotide repeat, has profound implications for protein function. The polyglutamine tract is located in the N-terminal transactivation domain (NTD) of the receptor.
This domain is critical for the initiation of gene transcription after the receptor has bound to an androgen and translocated to the nucleus. The length of the polyglutamine tract modulates the transcriptional activity of the receptor through several proposed mechanisms.
Research suggests that a longer polyglutamine tract may create a conformational change in the NTD that hinders its interaction with co-activator proteins and the basal transcription machinery. This results in a less efficient initiation of target gene expression. The inverse relationship between CAG repeat length and transcriptional activity has been demonstrated in vitro.
Clinically, this translates to a dose-response curve that is shifted to the right for individuals with longer repeats. They require a higher concentration of ligand (free testosterone) to achieve the same level of transcriptional activation and subsequent physiological effect. This molecular mechanism provides a robust scientific foundation for the clinical observation that patients with longer CAG repeats often require supraphysiological total testosterone levels to achieve symptomatic relief.

What Is the Clinical Utility of a Polygenic Score in TRT?
While individual gene testing is informative, the future of personalized hormonal medicine lies in the development of a polygenic risk score (PRS) for TRT response. A PRS would integrate the weighted effects of multiple relevant SNPs, including those in AR, CYP19A1, SHBG, and other genes like SRD5A2 (5-alpha reductase), into a single, quantitative score.
This score could predict an individual’s likely response to a standard TRT protocol, their risk for specific side effects (e.g. erythrocytosis, estrogenic symptoms), and their optimal therapeutic window for free testosterone. For instance, a PRS could stratify patients into categories such as “High Responder, High Estrogen Risk” or “Low Responder, Low Side Effect Risk,” allowing clinicians to proactively tailor protocols from the outset. This approach moves beyond reactive adjustments to a truly predictive and preventative model of care.

Interplay of Genetics in Ancillary Medication Efficacy
The pharmacogenomics of TRT extends beyond testosterone itself to the ancillary medications used in standard protocols, such as anastrozole and gonadorelin. The efficacy and side effect profile of these drugs are also subject to genetic modulation.
- Anastrozole and CYP Genes ∞ Anastrozole is an aromatase inhibitor, but its metabolism and clearance from the body are handled by cytochrome P450 enzymes in the liver, primarily CYP3A4. Genetic variations in CYP3A4 can alter the rate at which anastrozole is metabolized. Individuals who are “rapid metabolizers” may clear the drug more quickly, leading to a shorter duration of action and potentially requiring more frequent dosing (e.g. three times a week instead of two) to maintain effective aromatase inhibition. Conversely, “poor metabolizers” may experience a more profound and prolonged effect from a standard dose, increasing their risk of excessive estrogen suppression.
- Gonadorelin and GnRH Receptor ∞ Gonadorelin is a synthetic analog of Gonadotropin-Releasing Hormone (GnRH). It acts on the GnRH receptors in the pituitary gland to stimulate the release of Luteinizing Hormone (LH) and Follicle-Stimulating Hormone (FSH), thereby maintaining testicular function and endogenous testosterone production during TRT. Polymorphisms in the GnRH receptor gene (GNRHR) can affect the receptor’s binding affinity for gonadorelin and its downstream signaling capacity. While less studied in the context of TRT, variations in this receptor could theoretically influence the effectiveness of gonadorelin in preventing testicular atrophy and preserving fertility.
A comprehensive pharmacogenomic profile would therefore inform not only the testosterone dosage but the entire therapeutic regimen. It allows for a level of precision that is unattainable through traditional trial-and-error methods. By understanding the genetic blueprint of the patient’s entire hypothalamic-pituitary-gonadal-adrenal (HPGA) axis and the relevant metabolic pathways, clinicians can construct a protocol that is truly synergistic with the individual’s unique biology.
References
- Zitzmann, M. “Effects of testosterone replacement and its pharmacogenetics on physical performance and metabolism.” Asian Journal of Andrology, vol. 10, no. 3, 2008, pp. 366-73.
- Panizzon, M. S. et al. “Genetic Variation in the Androgen Receptor Modifies the Association between Testosterone and Vitality in Middle-Aged Men.” The Journal of Sexual Medicine, vol. 18, no. 12, 2021, pp. 1995-2004.
- Hsing, A. W. et al. “Polymorphisms in the
Androgen Receptor, Aromatase (CYP19), and Endogenous Sex Hormones in Young Men.” Cancer Epidemiology, Biomarkers & Prevention, vol. 16, no. 1, 2007, pp. 152-57. - Vermeulen, A. et al. “A critical evaluation of simple methods for the estimation of free testosterone in serum.” The Journal of Clinical Endocrinology & Metabolism, vol. 84, no. 10, 1999, pp. 3666-72.
- Ding, E. L. et al. “Sex hormone-binding globulin and risk of type 2 diabetes in women and men.” The New England Journal of Medicine, vol. 361, no. 12, 2009, pp. 1152-63.
- Grishkovskaya, I. et al. “Crystal structure of human sex hormone-binding globulin ∞ steroid binding and dimerization.” The EMBO Journal, vol. 19, no. 4, 2000, pp. 504-12.
- Canale, D. et al. “The androgen receptor CAG repeat ∞ a modifier of the relationship between testosterone and sexual function in aging men.” The Journal of Clinical Endocrinology & Metabolism, vol. 90, no. 10, 2005, pp. 5687-92.
- Eriksson, J. et al. “The G261V polymorphism in the aromatase gene is associated with higher bone mineral density in elderly men.” The Journal of Clinical Endocrinology & Metabolism, vol. 90, no. 9, 2005, pp. 5293-98.
- Yarrow, J. F. et al. “Testosterone and bone ∞ basis of evidence-based androgen therapy for osteoporosis in men.” Current Opinion in Supportive and Palliative Care, vol. 5, no. 3, 2011, pp. 234-41.
- Antonio, L. et al. “SHBG Gene Polymorphisms and Their Influence on Serum SHBG, Total and Free Testosterone Concentrations in Men.” The Journal of Clinical Endocrinology & Metabolism, vol. 109, no. 7, 2024, pp. e2585-e2593.

Reflection

The Dialogue between Your Genes and Your Life
The information presented here provides a map, but you are the territory. This knowledge is designed to be a tool for a more informed and collaborative conversation with your healthcare provider. Your body is constantly communicating its status through the symptoms you feel and the way it responds to therapy.
The science of pharmacogenomics gives us a way to translate that communication, to understand the biological dialect that is uniquely yours. This process is one of discovery. It is about connecting the subjective feelings of your lived experience with the objective data of your genetic code.
This deeper understanding is the foundation of true hormonal optimization. It shifts the goal from simply achieving a number on a lab report to restoring function and vitality to the entire system. Your personal health journey is an ongoing dialogue between your innate biological predispositions and the choices you make every day.
The path forward involves listening to that dialogue with greater clarity and using this knowledge to make more precise, effective, and personalized decisions for your long-term well-being.



