

Fundamentals
Perhaps you have noticed a subtle shift, a quiet diminishment of your usual vigor. Maybe the morning light does not bring the same sense of readiness, or your physical resilience feels less robust than it once did.
Many individuals experience a gradual decline in energy, changes in body composition, or a lessening of their overall zest for life, often attributing these shifts to the inevitable march of time. Yet, these sensations, these alterations in how you feel and function, frequently signal deeper physiological adjustments within your body’s intricate messaging network. Understanding these internal communications, particularly those orchestrated by your endocrine system, represents a significant step toward reclaiming your vitality.
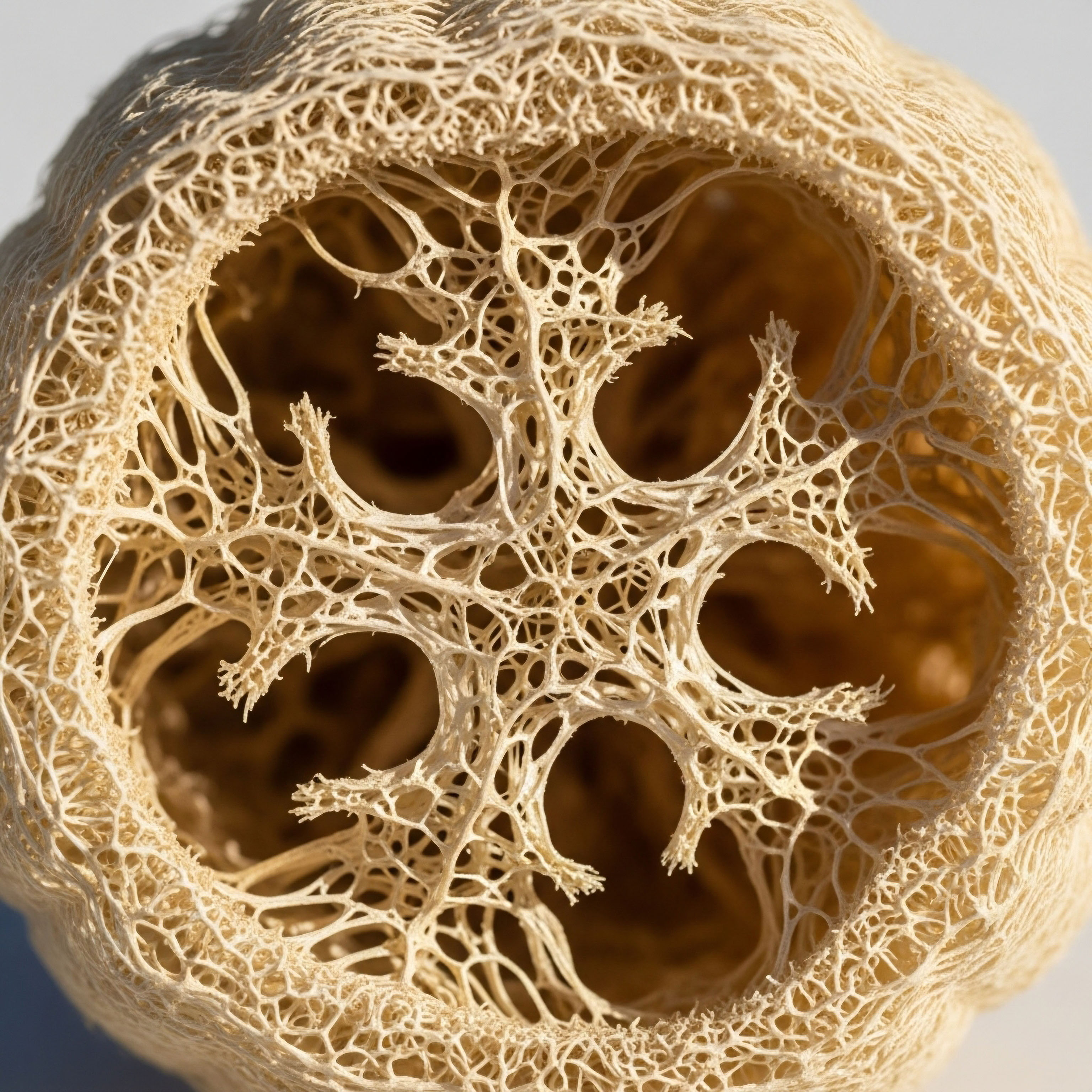
Your body operates through a sophisticated system of chemical messengers known as hormones. These substances, produced by various glands, travel through your bloodstream to influence nearly every cell and process. Think of them as the precise instructions that dictate how your internal systems operate, from your metabolism and mood to your strength and cognitive clarity.
When these instructions become muddled or insufficient, the effects can ripple across your entire being, manifesting as the very symptoms that prompt a search for answers.
Testosterone, a steroid hormone, plays a central role in both male and female physiology, extending far beyond its well-known associations with reproductive health. In men, it contributes to muscle mass, bone density, red blood cell production, mood regulation, and cognitive function.
For women, even in much smaller concentrations, testosterone is crucial for libido, bone health, energy levels, and overall well-being. A reduction in its optimal levels can therefore affect a wide array of bodily systems, leading to a constellation of symptoms that can feel isolating and perplexing.
Recognizing subtle shifts in energy, body composition, or mood can indicate underlying hormonal changes, prompting a deeper look into the body’s internal messaging systems.
When considering whether hormonal support, such as testosterone therapy, might be appropriate, clinicians begin by listening intently to your lived experience. They seek to understand the specific changes you have observed and the impact these changes have had on your daily life.
This initial conversation is paramount, establishing a foundation of trust and providing critical subjective data that complements objective laboratory findings. A comprehensive evaluation always starts with your personal narrative, validating the sensations you feel and the concerns you hold.
What Are the Initial Indicators for Testosterone Evaluation?
The decision to investigate testosterone levels typically arises from a collection of persistent symptoms that suggest a potential hormonal imbalance. These indicators are diverse and can vary significantly between individuals, reflecting the widespread influence of testosterone throughout the body.
For men, common complaints include a noticeable decrease in libido, a reduction in spontaneous erections, and a general decline in energy levels. Many also report a loss of muscle strength and endurance, an increase in body fat, particularly around the abdomen, and a diminished sense of well-being.
Women, too, experience distinct signs that may point to a need for testosterone assessment. These often involve a persistent lack of sexual desire, unexplained fatigue, and a feeling of mental fogginess or difficulty concentrating. Changes in body composition, such as an increase in fat mass despite consistent exercise, can also be a contributing factor. The symptoms are rarely isolated; instead, they often present as a pattern that disrupts daily function and diminishes life quality.
Beyond these primary indicators, clinicians also consider other, less obvious signs. These might include persistent low mood, irritability, or even symptoms that mimic depression, which can sometimes be linked to hormonal fluctuations. Sleep disturbances, reduced exercise tolerance, and a general lack of motivation are additional elements that contribute to the clinical picture.
The presence of several of these symptoms, especially when they persist over time and cannot be readily explained by other factors, signals the importance of a thorough hormonal investigation.
The initial consultation involves a detailed medical history, exploring past health conditions, medications, and lifestyle factors that could influence hormonal status. This includes a review of sleep patterns, nutritional habits, stress levels, and physical activity. Understanding your overall health context provides a holistic view, allowing for a more precise interpretation of subsequent diagnostic steps. This initial phase is about gathering all relevant pieces of your health puzzle.


Intermediate
Once a comprehensive symptom profile has been established, clinicians proceed with a series of diagnostic evaluations to objectively assess hormonal status. This process moves beyond subjective feelings to gather concrete data, providing a clear picture of your internal biochemical environment. The cornerstone of this evaluation involves specific laboratory tests designed to measure circulating hormone levels and related markers. These tests are not merely snapshots; they are windows into the dynamic interplay of your endocrine system.
A standard initial blood panel for assessing testosterone suitability typically includes several key measurements. These provide a foundational understanding of your hormonal landscape ∞
- Total Testosterone ∞ This measurement reflects the total amount of testosterone circulating in your bloodstream, both bound and unbound.
- Free Testosterone ∞ This represents the biologically active form of testosterone, the portion readily available to your tissues and cells. This measurement often correlates more closely with symptoms than total testosterone.
- Sex Hormone Binding Globulin (SHBG) ∞ This protein binds to testosterone, making it unavailable for cellular use. Levels of SHBG can significantly influence the amount of free testosterone, even if total testosterone appears within range.
- Luteinizing Hormone (LH) and Follicle-Stimulating Hormone (FSH) ∞ These pituitary hormones regulate testosterone production in the testes (men) and ovaries (women). Their levels help determine if a low testosterone reading originates from the gonads (primary hypogonadism) or the pituitary/hypothalamus (secondary hypogonadism).
- Estradiol (E2) ∞ Testosterone can convert into estrogen (estradiol) in the body. Monitoring estradiol levels is important, particularly in men, to manage potential side effects of testosterone therapy.
- Prolactin ∞ Elevated prolactin levels can sometimes suppress testosterone production, warranting investigation.
The timing of blood draws is also important, particularly for testosterone, which exhibits a diurnal rhythm. Levels are typically highest in the morning, so samples are often collected between 7:00 AM and 10:00 AM to capture peak concentrations and ensure consistent comparisons. Interpreting these results requires clinical expertise, as reference ranges can vary between laboratories, and optimal levels for an individual may differ from population averages.
Laboratory tests, including total and free testosterone, SHBG, LH, FSH, estradiol, and prolactin, provide objective data essential for evaluating hormonal status and guiding clinical decisions.

How Do Clinicians Interpret Laboratory Results?
Interpreting laboratory results extends beyond simply noting whether a number falls within a “normal” range. A clinician considers the full spectrum of your symptoms, your age, your overall health status, and the interplay between various hormone levels. For instance, a total testosterone level that appears borderline low might be clinically significant if accompanied by consistently low free testosterone and a high SHBG, especially when severe symptoms are present. The context of your individual physiology is always paramount.
The diagnostic process also involves ruling out other potential causes for your symptoms. Conditions such as thyroid dysfunction, vitamin deficiencies, sleep apnea, chronic stress, or certain medications can mimic the signs of low testosterone. A thorough clinician will investigate these possibilities to ensure that any prescribed therapy addresses the root cause of your concerns. This comprehensive approach ensures that treatment is targeted and appropriate for your unique situation.
For men, if a diagnosis of low testosterone (hypogonadism) is confirmed, the discussion often turns to Testosterone Replacement Therapy (TRT). A common protocol involves weekly intramuscular injections of Testosterone Cypionate, typically at a concentration of 200mg/ml. This method provides a steady release of the hormone, aiming to restore physiological levels. To mitigate potential side effects and preserve natural function, adjunctive medications are frequently incorporated.
One such addition is Gonadorelin, administered via subcutaneous injections, often twice weekly. This peptide stimulates the pituitary gland to release LH and FSH, thereby helping to maintain the body’s own testosterone production and supporting testicular function, which is particularly relevant for men concerned about fertility.
Another common component is Anastrozole, an oral tablet taken twice weekly, which acts as an aromatase inhibitor. Its purpose is to reduce the conversion of testosterone into estrogen, preventing potential estrogen-related side effects such as gynecomastia or fluid retention. In some cases, Enclomiphene may be included to specifically support LH and FSH levels, offering another pathway to maintain endogenous hormone production.
For women experiencing symptoms related to hormonal changes, including those in pre-menopausal, peri-menopausal, or post-menopausal stages, testosterone therapy protocols are carefully tailored. The dosage of Testosterone Cypionate is significantly lower than for men, typically 10 ∞ 20 units (0.1 ∞ 0.2ml) weekly via subcutaneous injection. This precise dosing aims to restore optimal levels without causing virilizing side effects.
Progesterone is often prescribed alongside testosterone for women, particularly those who are peri- or post-menopausal, to ensure hormonal balance and protect the uterine lining. The specific regimen depends on individual needs and menopausal status. Another option for women is Pellet Therapy, which involves the subcutaneous insertion of long-acting testosterone pellets.
This method provides a consistent release of the hormone over several months, reducing the frequency of administration. When appropriate, Anastrozole may also be used with pellet therapy to manage estrogen conversion, though this is less common in women due to their lower testosterone dosages.
Clinicians also consider specific protocols for men who have discontinued TRT or are actively trying to conceive. These protocols focus on stimulating natural hormone production and restoring fertility. A combination of medications is typically employed ∞
- Gonadorelin ∞ Continues to stimulate LH and FSH release.
- Tamoxifen ∞ A selective estrogen receptor modulator (SERM) that can block estrogen’s negative feedback on the pituitary, thereby increasing LH and FSH.
- Clomid (Clomiphene Citrate) ∞ Another SERM that works similarly to Tamoxifen, promoting endogenous testosterone production.
- Anastrozole ∞ Optionally included to manage estrogen levels during the recovery phase.
These detailed protocols reflect a commitment to personalized care, recognizing that each individual’s physiological response to hormonal interventions is unique. The goal is always to restore balance and function with precision, minimizing unwanted effects while maximizing therapeutic benefits.


Academic
The determination of testosterone therapy suitability extends into a sophisticated understanding of the human endocrine system, particularly the Hypothalamic-Pituitary-Gonadal (HPG) axis. This intricate feedback loop serves as the central regulatory mechanism for sex hormone production. The hypothalamus releases Gonadotropin-Releasing Hormone (GnRH), which stimulates the pituitary gland to secrete Luteinizing Hormone (LH) and Follicle-Stimulating Hormone (FSH).
LH then acts on the Leydig cells in the testes (men) or the theca cells in the ovaries (women) to produce testosterone. FSH, conversely, supports spermatogenesis in men and follicular development in women. Elevated levels of testosterone, and its conversion product estradiol, provide negative feedback to the hypothalamus and pituitary, thereby modulating GnRH, LH, and FSH release. This precise regulation ensures hormonal homeostasis.
When exogenous testosterone is introduced, this delicate feedback system is directly impacted. The body perceives the presence of sufficient testosterone, leading to a suppression of GnRH, LH, and FSH production. This suppression, if prolonged, can result in testicular atrophy in men and a cessation of endogenous testosterone production. Understanding this physiological response is paramount for clinicians, guiding the decision to incorporate agents like Gonadorelin or selective estrogen receptor modulators (SERMs) to preserve aspects of the HPG axis.
The metabolic implications of testosterone status are also a significant area of clinical consideration. Testosterone receptors are widely distributed throughout various tissues, including adipose tissue, muscle, and bone. Low testosterone levels are frequently associated with adverse metabolic profiles, including increased insulin resistance, dyslipidemia, and central adiposity.
Research indicates a reciprocal relationship ∞ metabolic dysfunction can contribute to lower testosterone, and restoring testosterone to optimal levels can improve metabolic markers. For instance, a study published in the Journal of Clinical Endocrinology & Metabolism demonstrated that testosterone therapy in hypogonadal men improved insulin sensitivity and reduced fat mass. This connection underscores the systemic impact of hormonal balance on overall metabolic health.
The HPG axis, a complex feedback loop, governs sex hormone production, and its intricate regulation is a primary consideration when evaluating testosterone therapy.

How Does Testosterone Influence Metabolic Pathways?
Testosterone exerts its influence on metabolic pathways through several mechanisms. It promotes lean muscle mass accretion, which is metabolically active tissue, thereby increasing basal metabolic rate. It also appears to directly influence adipocyte differentiation and lipid metabolism, potentially reducing fat storage.
Furthermore, testosterone has been shown to improve glucose uptake in muscle cells and enhance insulin signaling, contributing to better glycemic control. The interplay between testosterone and metabolic health is a complex area of ongoing research, but the clinical evidence increasingly supports the notion that optimal testosterone levels are integral to maintaining metabolic resilience.
The role of peptides in hormonal optimization represents an advanced therapeutic strategy. Growth Hormone Releasing Peptides (GHRPs), such as Sermorelin, Ipamorelin / CJC-1295, Tesamorelin, and Hexarelin, stimulate the pituitary gland to release growth hormone (GH) in a pulsatile, physiological manner. Unlike exogenous GH administration, which can suppress natural production, these peptides work with the body’s inherent mechanisms.
MK-677, an oral secretagogue, also increases GH and IGF-1 levels. These peptides are often considered for active adults and athletes seeking benefits such as improved body composition, enhanced recovery, better sleep quality, and anti-aging effects. Their application requires a deep understanding of their pharmacodynamics and the individual’s physiological needs.
Beyond growth hormone secretagogues, other targeted peptides offer specific therapeutic applications. PT-141 (Bremelanotide), for example, acts on melanocortin receptors in the brain to address sexual dysfunction, particularly low libido, in both men and women. Its mechanism of action is distinct from traditional phosphodiesterase-5 inhibitors, operating centrally to influence sexual desire.
Pentadeca Arginate (PDA), a synthetic peptide, is gaining attention for its potential in tissue repair, wound healing, and modulating inflammatory responses. These peptides represent a frontier in personalized wellness protocols, offering precise interventions for specific physiological challenges.
The decision to initiate testosterone therapy, or any hormonal optimization protocol, is never made in isolation. It involves a continuous dialogue between the clinician and the individual, adapting the protocol based on ongoing symptom assessment, regular laboratory monitoring, and a deep understanding of the body’s adaptive responses. This dynamic process ensures that the therapy remains aligned with the individual’s evolving needs and health objectives.

How Do Clinicians Monitor Therapy Progress?
Ongoing monitoring is a cornerstone of responsible testosterone therapy. Regular blood tests are conducted to assess the effectiveness of the protocol and to identify any potential side effects. These typically include repeat measurements of total and free testosterone, estradiol, and complete blood count (CBC) to monitor red blood cell production, as testosterone can sometimes increase hematocrit. Liver function tests and prostate-specific antigen (PSA) in men are also routinely checked.
| Parameter | Clinical Rationale | Frequency (Initial Phase) |
|---|---|---|
| Total & Free Testosterone | Assess therapeutic efficacy and ensure levels are within optimal physiological range. | Every 6-8 weeks |
| Estradiol (E2) | Monitor for excessive conversion of testosterone to estrogen, which can cause side effects. | Every 6-8 weeks |
| Hematocrit/Hemoglobin (CBC) | Check for polycythemia (excessive red blood cell production), a potential side effect. | Every 3-6 months |
| PSA (Men) | Screen for prostate health, particularly in older men. | Annually or as indicated |
| Lipid Panel | Assess cardiovascular risk factors, as testosterone can influence lipid profiles. | Annually |
Beyond laboratory values, the clinician continuously evaluates the individual’s subjective experience. Are symptoms improving? Is energy returning? Is mood stabilizing? This qualitative feedback is just as important as the quantitative data, providing a holistic view of the therapy’s impact.
Adjustments to dosage or the inclusion of adjunctive medications are made based on this combined assessment, ensuring the protocol remains precisely calibrated to the individual’s unique biological response. The goal is not merely to normalize a number, but to restore a sense of well-being and optimal function.

References
- Saad, F. et al. “Testosterone therapy in men with hypogonadism and metabolic syndrome ∞ a systematic review and meta-analysis of randomized controlled trials.” Journal of Clinical Endocrinology & Metabolism, vol. 99, no. 10, 2014, pp. 3537-3545.
- Bhasin, S. et al. “Testosterone therapy in men with androgen deficiency syndromes ∞ an Endocrine Society clinical practice guideline.” Journal of Clinical Endocrinology & Metabolism, vol. 95, no. 6, 2010, pp. 2536-2559.
- Davis, S. R. et al. “Androgen therapy in women ∞ a systematic review.” Journal of Clinical Endocrinology & Metabolism, vol. 99, no. 10, 2014, pp. 3489-3503.
- Guyton, A. C. & Hall, J. E. Textbook of Medical Physiology. 13th ed. Elsevier, 2016.
- Boron, W. F. & Boulpaep, E. L. Medical Physiology. 3rd ed. Elsevier, 2017.
- Veldhuis, J. D. et al. “Physiological regulation of the human growth hormone (GH)-insulin-like growth factor I (IGF-I) axis ∞ evidence for complex pulsatile and feedback control.” Endocrine Reviews, vol. 13, no. 6, 1992, pp. 769-791.
- Shabsigh, R. et al. “The role of testosterone in the treatment of erectile dysfunction.” Journal of Sexual Medicine, vol. 1, no. 1, 2004, pp. 26-32.
- Handelsman, D. J. & Yeap, B. B. “Testosterone and men’s health ∞ the clinical and research challenges.” Journal of Clinical Endocrinology & Metabolism, vol. 101, no. 3, 2016, pp. 835-844.
- Traish, A. M. et al. “The dark side of testosterone deficiency ∞ II. Type 2 diabetes and insulin resistance.” Journal of Andrology, vol. 33, no. 3, 2012, pp. 321-332.
- Miller, D. W. et al. “Growth hormone-releasing peptides ∞ a review of their current and potential clinical applications.” Clinical Interventions in Aging, vol. 10, 2015, pp. 1699-1709.

Reflection
Your personal health journey is a continuous exploration, a dynamic process of understanding and recalibrating your body’s systems. The knowledge you have gained about how clinicians assess testosterone therapy suitability is not merely information; it is a tool for self-advocacy and informed decision-making. Recognizing the interconnectedness of your endocrine system, metabolic function, and overall well-being allows you to approach your health with a renewed sense of agency.
Consider this understanding as the initial step on a path toward greater vitality. Your body possesses an innate intelligence, and by aligning with its needs through precise, evidence-based interventions, you can restore balance and function. This journey is deeply personal, requiring a partnership with clinicians who respect your lived experience while applying rigorous scientific principles. The aim is always to optimize your unique biological systems, allowing you to reclaim your full potential without compromise.

What Does Personalized Wellness Mean for You?
The concept of personalized wellness extends beyond a single hormone or a single protocol. It encompasses a holistic view of your health, considering how lifestyle, nutrition, stress management, and targeted therapies collectively influence your physiological state. This integrated approach recognizes that true well-being arises from a harmonious interplay of all bodily systems. Your commitment to understanding these intricate connections is a powerful act of self-care.
As you move forward, allow this deeper understanding to guide your conversations with healthcare providers. Ask questions, seek clarity, and remain an active participant in your care. The goal is not simply to alleviate symptoms, but to achieve a state of optimal function and sustained vitality. Your body holds the capacity for remarkable resilience, and with the right guidance, you can unlock its inherent ability to perform at its best.



