

Fundamentals
The experience of your body sending distress signals, perhaps through persistent skin itching or a disquieting change in the color of your urine, is a profound personal event. These sensations are your physiology communicating a disruption.
When anabolic-androgenic steroids (AAS) are introduced into your system, they initiate a cascade of biochemical events, with the liver positioned at the very center of this metabolic storm. Your liver’s role extends far beyond simple filtration; it is a sophisticated chemical processing facility, responsible for synthesizing, regulating, and clearing countless substances. A primary function within this facility is the production and movement of bile.
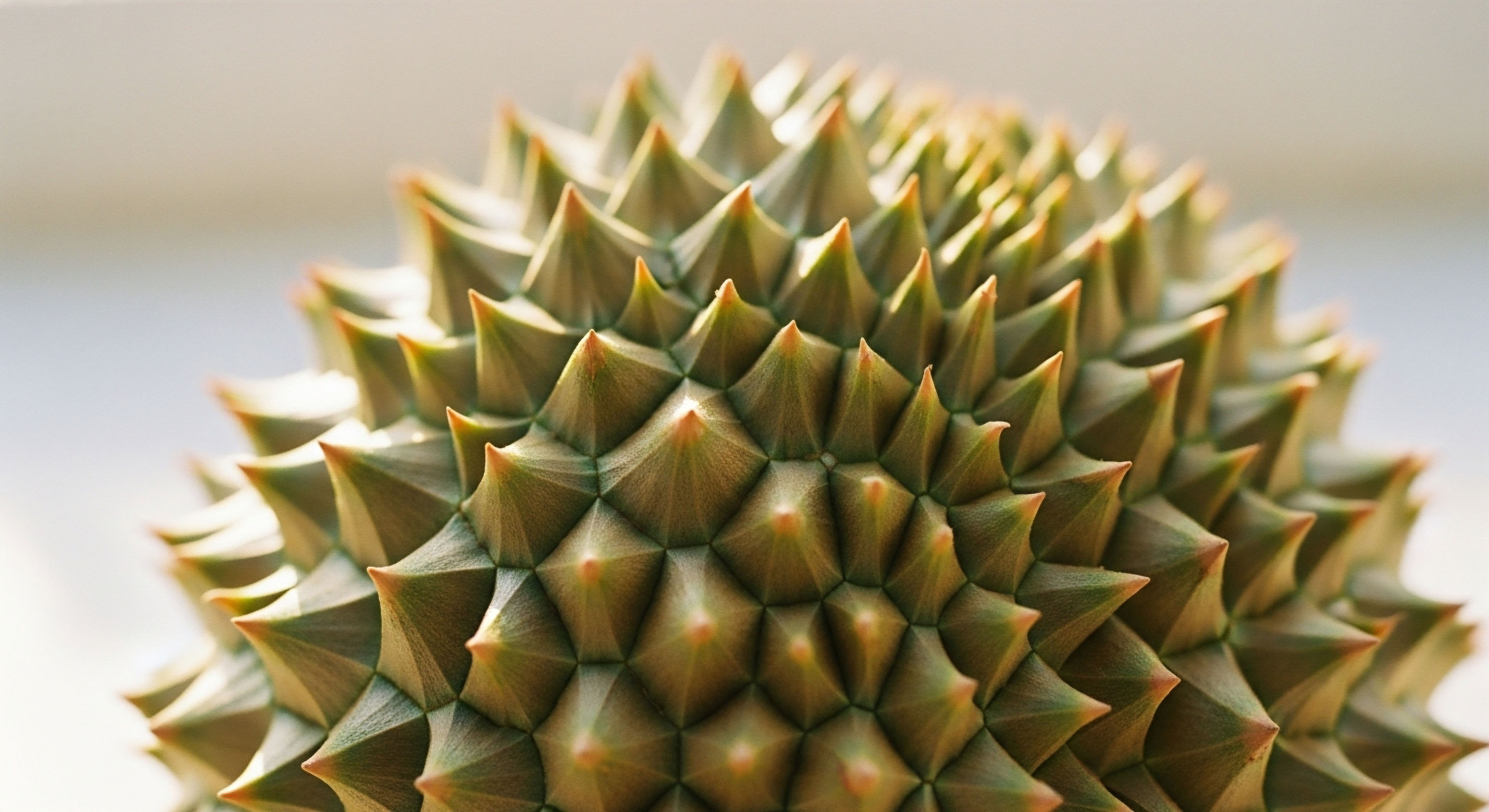
Bile is a complex fluid essential for digesting fats and eliminating waste products from the body. Think of the liver’s bile duct network as an intricate, one-way drainage system, meticulously designed to carry bile from the liver cells where it is made, through progressively larger channels, and ultimately to the gallbladder and small intestine.
This flow is constant, precisely regulated, and vital for systemic health. Certain types of anabolic steroids, particularly those modified for oral consumption, introduce a powerful disruptive force to this delicate system. They can directly interfere with the microscopic pumps and structural components within liver cells that are responsible for moving bile out.
The introduction of specific anabolic steroids can obstruct the liver’s natural bile drainage pathways, leading to an internal backup.
This interference causes a condition known as cholestasis, which is the medical term for a reduction or stoppage of bile flow. When bile cannot exit the liver cells efficiently, it accumulates. This backup is akin to a blockage in a sophisticated plumbing network.
The pressure builds, and the constituents of bile, including bilirubin (a yellow pigment) and bile acids, begin to seep back into the bloodstream. The accumulation of bilirubin in the blood leads to jaundice, which manifests as a yellowing of the skin and eyes. The deposition of bile salts in the skin is what triggers the intense and often maddening itching, known as pruritus. These are direct, physical manifestations of a biochemical traffic jam occurring deep within your liver.

The Architecture of Bile Transport
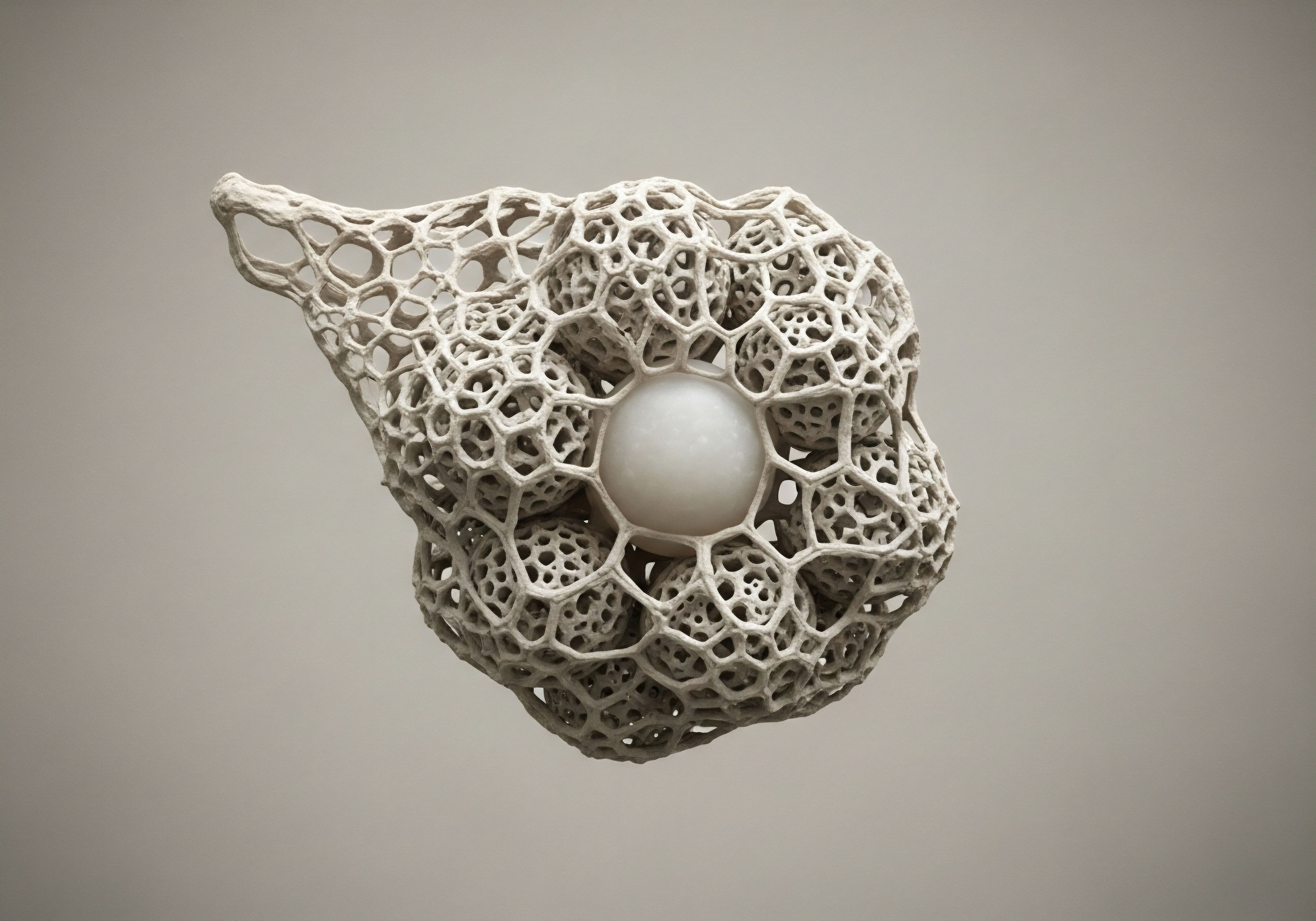
To appreciate the specificity of this disruption, one must visualize the liver at a microscopic scale. Each liver cell, or hepatocyte, is a powerhouse of activity. On one side, it absorbs compounds from the blood; on the other, it secretes bile into a tiny, sealed channel called a bile canaliculus.
This is the very beginning of the bile duct system. The integrity of the hepatocyte’s internal scaffolding, made of microfilaments, is essential for maintaining the cell’s shape and the proper function of these channels. Anabolic steroids Meaning ∞ Anabolic steroids, formally known as anabolic-androgenic steroids (AAS), are synthetic derivatives of the natural male hormone testosterone. can destabilize this internal architecture, impairing the cell’s ability to contract and propel bile forward. This structural impairment is one of the foundational ways these compounds initiate cholestasis, compromising the very mechanics of bile movement from its point of origin.

Intermediate
The hepatotoxicity Meaning ∞ Hepatotoxicity refers to the occurrence of liver injury or dysfunction caused by exposure to a drug, chemical, or other non-infectious agent. associated with anabolic-androgenic steroids is not uniform across all compounds. A critical distinction exists between oral and injectable formulations, which relates directly to their molecular structure and metabolic fate. Many oral AAS are chemically modified by adding an alkyl group at the 17th carbon position, creating what are known as C-17 alpha-alkylated (C17aa) steroids.
This modification is designed to protect the molecule from being broken down by the liver on its first pass through the system, thereby increasing its oral bioavailability. This structural alteration, however, is the primary reason for their pronounced effect on bile flow. Compounds like stanozolol, oxymetholone, and methandienone fall into this category.
The resulting liver condition is often described as a “bland cholestasis.” This term signifies that the primary event is the functional obstruction of bile flow at the cellular level, with less of the overt inflammation and damage to the bile ducts themselves that characterize other liver diseases.
The injury is more functional than structural in its initial stages. The symptoms of this condition, such as jaundice Meaning ∞ Jaundice is a clinical sign characterized by the yellowish discoloration of the skin, mucous membranes, and the whites of the eyes, medically termed scleral icterus. and pruritus, can be prolonged and severe, even after the offending steroid is discontinued. Recovery depends on the liver’s ability to restore its normal transport functions and clear the accumulated bile acids.

What Is the Clinical Signature of AAS Induced Cholestasis?
The diagnosis of AAS-induced cholestasis Meaning ∞ Cholestasis describes the impaired or complete cessation of bile flow from the liver into the duodenum, leading to bile component retention within hepatocytes and systemic circulation. is guided by a characteristic pattern of blood test abnormalities that reflects the underlying pathophysiology. Liver function tests Meaning ∞ Liver Function Tests (LFTs) are blood assays assessing the liver’s health and operational status. (LFTs) will typically show a disproportionate elevation in markers of cholestasis compared to markers of hepatocellular injury.
- Alkaline Phosphatase (ALP) ∞ This enzyme is concentrated in the cells lining the bile ducts. When bile flow is obstructed, ALP levels in the blood rise significantly.
- Bilirubin ∞ A high total and direct bilirubin level is the hallmark of cholestasis, confirming that the liver is processing bilirubin but failing to excrete it into the bile. This is what causes jaundice.
- Gamma-Glutamyl Transferase (GGT) ∞ Similar to ALP, GGT is another enzyme that becomes elevated in cholestatic conditions.
- Aspartate Aminotransferase (AST) and Alanine Aminotransferase (ALT) ∞ These enzymes are markers of direct liver cell damage. In bland cholestasis, AST and ALT levels may be only mildly elevated, or sometimes even within the normal range, which helps distinguish it from conditions like viral hepatitis where these markers are typically very high.
The following table outlines the common clinical signs of AAS-induced cholestasis and their direct biological causes.
| Clinical Sign | Underlying Biological Mechanism |
|---|---|
| Jaundice (Yellow Skin/Eyes) | Accumulation of bilirubin in the bloodstream due to impaired excretion from liver cells into the bile ducts. |
| Pruritus (Itching) | Deposition of bile acids and salts into the skin, which irritates nerve endings. |
| Dark Urine | Excretion of excess conjugated bilirubin by the kidneys, as the primary liver excretion route is blocked. |
| Pale Stools | Lack of bilirubin metabolites (stercobilin) reaching the intestine, which normally gives stool its characteristic color. |

The Role of Specific Transporter Proteins
At the heart of AAS-induced cholestasis is the impairment of specific protein pumps on the surface of the liver cell. The most important of these is the Bile Salt Export Pump Meaning ∞ The Bile Salt Export Pump, or BSEP (ABCB11), is a pivotal ATP-dependent transporter protein situated on the canalicular membrane of hepatocytes. (BSEP). This protein is responsible for actively transporting bile acids out of the hepatocyte and into the canaliculus.
C17aa steroids appear to directly inhibit the function of BSEP and other key transporters. This inhibition stops the bile acid “assembly line” at its most critical step. When bile acids Meaning ∞ Bile acids are steroid molecules synthesized in the liver from cholesterol, primarily serving as detergents to facilitate the digestion and absorption of dietary fats and fat-soluble vitamins within the small intestine. are trapped inside the cell, they exert a direct toxic effect, disrupting mitochondrial function and generating oxidative stress, which can lead to hepatocyte necrosis over time.
The treatment with agents like ursodeoxycholic acid (UDCA) is sometimes employed to help promote bile flow through alternative pathways and protect liver cells from the toxicity of the accumulated bile acids.

Academic
The molecular pathogenesis of anabolic-androgenic steroid-induced cholestasis is a sophisticated process involving the genomic and non-genomic actions of these compounds within the hepatocyte. The central event is the disruption of bile acid homeostasis, which is maintained by a complex network of nuclear receptors and membrane transport proteins.
Supraphysiological concentrations of C-17 alpha-alkylated steroids Meaning ∞ C-17 alpha-alkylated steroids are synthetic compounds modified at the 17th carbon position with an alkyl group. appear to commandeer this regulatory network, leading to a profound failure of bile secretion. This process transcends simple mechanical obstruction; it is a fundamental reprogramming of the cell’s genetic machinery responsible for bile acid transport.
Androgen receptors (ARs) are expressed in liver cells, and their activation by AAS is a key initiating event. The binding of an AAS molecule to an AR can modulate the transcription of a host of genes, including those that code for the very proteins that transport bile acids in and out of the cell.
Research suggests that AAS can downregulate the expression of critical efflux transporters like BSEP (ABCB11) and the Multidrug Resistance-Associated Protein 2 (MRP2/ABCC2), which is responsible for exporting conjugated bilirubin and other organic anions. This transcriptional repression effectively removes the “exit doors” for bile components from the hepatocyte.
The cholestatic effect of certain anabolic steroids is rooted in their ability to alter gene expression within liver cells, shutting down the primary pathways for bile acid removal.
Simultaneously, AAS can affect influx transporters on the blood-facing side of the hepatocyte, further compounding the problem. This dual action of inhibiting efflux and potentially altering influx creates a rapid and severe intracellular accumulation of bile acids. These bile acids, particularly hydrophobic species, are potent detergents that disrupt cellular membranes.
Their accumulation within the hepatocyte leads to mitochondrial dysfunction, the generation of reactive oxygen species (ROS), and the initiation of apoptotic and necrotic cell death pathways. This direct cytotoxicity is a defining feature of the injury.

How Does Genetic Variation Influence Susceptibility?
The observation that not all individuals who use AAS develop severe cholestasis points toward the influence of underlying genetic predispositions. Polymorphisms in the genes encoding for bile acid transporters like BSEP and MRP2 can affect their baseline expression or function.
An individual with a pre-existing, genetically determined lower transport capacity may be significantly more vulnerable to the inhibitory effects of AAS. When exposed to the drug, their already-limited transport system is pushed below the critical threshold required to maintain bile flow, precipitating a cholestatic event. This concept helps explain the idiosyncratic nature of the toxicity, where some individuals can experience severe liver injury after relatively short courses of the drug.
The table below details some of the key molecular transporters involved in hepatobiliary transport and how they are affected by cholestatic agents.
| Transporter Protein | Location on Hepatocyte | Normal Function | Effect of C17aa Steroids |
|---|---|---|---|
| BSEP (ABCB11) | Canalicular Membrane | Primary transporter for bile salts out of the hepatocyte. | Function is inhibited and gene expression is downregulated. |
| MRP2 (ABCC2) | Canalicular Membrane | Transports conjugated bilirubin and other organic anions. | Function is inhibited, contributing to jaundice. |
| MDR3 (ABCB4) | Canalicular Membrane | Flips phosphatidylcholine into the bile, protecting duct cells. | Impairment can lead to more toxic bile composition. |
| NTCP | Basolateral Membrane | Primary transporter for bile salts from the blood into the hepatocyte. | Dysregulation can contribute to intracellular accumulation. |

Beyond Bland Cholestasis the Path to Chronic Injury
While AAS-induced cholestasis is often reversible, chronic, high-dose use can lead to more permanent and severe forms of liver pathology. One such condition is peliosis hepatis, a rare disorder characterized by the formation of blood-filled cysts throughout the liver.
The mechanism is thought to involve damage to the sinusoidal endothelial cells that line the liver’s blood channels, leading to vascular leakage and the formation of these cavities. Another long-term consequence is the development of hepatic tumors, including benign adenomas and malignant hepatocellular carcinoma.
The proliferative signals sent by the constant activation of androgen receptors, combined with a state of chronic cellular injury and regeneration, can create an environment conducive to neoplastic transformation. These severe outcomes underscore the progressive nature of the liver damage, which begins with a functional disruption of bile flow and can evolve into irreversible structural and malignant disease.

References
- Petrovic, A. Vukadin, S. Sikora, R. Bojanic, K. Smolic, R. Plavec, D. Wu, G. Y. & Smolic, M. “Anabolic androgenic steroid-induced liver injury ∞ An update.” World Journal of Gastroenterology, vol. 28, no. 26, 2022, pp. 3063-3078.
- “Androgenic Steroids.” LiverTox ∞ Clinical and Research Information on Drug-Induced Liver Injury, National Institute of Diabetes and Digestive and Kidney Diseases, 30 May 2020.
- Al-Zuhair, A. et al. “Anabolic Steroid-Induced Cholestasis.” Cureus, vol. 13, no. 9, 2021, e17869.
- Robles-Diaz, M. et al. “Research Day ∞ Delayed Severe Drug Induced Cholestasis After Anabolic Steroids Exposure.” American Journal of Gastroenterology, vol. 111, 2016, S25.
- Korkmaz, H. and S. A. U. Ayşegül. “(PDF) Anabolic Steroid-Induced Cholestatic Liver Injury ∞ A Case Report – ResearchGate.” Journal of Health Sciences and Medicine, vol. 5, no. 4, 2022, pp. 1121-1124.

Reflection
Understanding the intricate pathways by which anabolic steroids disrupt hepatic function moves us toward a more profound appreciation for the body’s elegant biological systems. The knowledge of how a single molecular modification can precipitate a cascade of events, from genetic transcription to the physical manifestation of jaundice, provides a powerful lens.
It allows you to see your physiology as a responsive, interconnected network. This understanding is the foundational step. Your personal health is a dynamic state, governed by a unique interplay of genetics, environment, and choice. The path forward involves using this detailed knowledge not as a final answer, but as a catalyst for informed dialogue and deliberate action in the stewardship of your own well-being.










