
Fundamentals
You may feel a persistent, unexplained fatigue, or notice that your body composition is changing in ways that feel disconnected from your diet and exercise habits. These experiences are valid and important signals from your body. They are data points, and understanding their origin is the first step toward reclaiming your vitality.
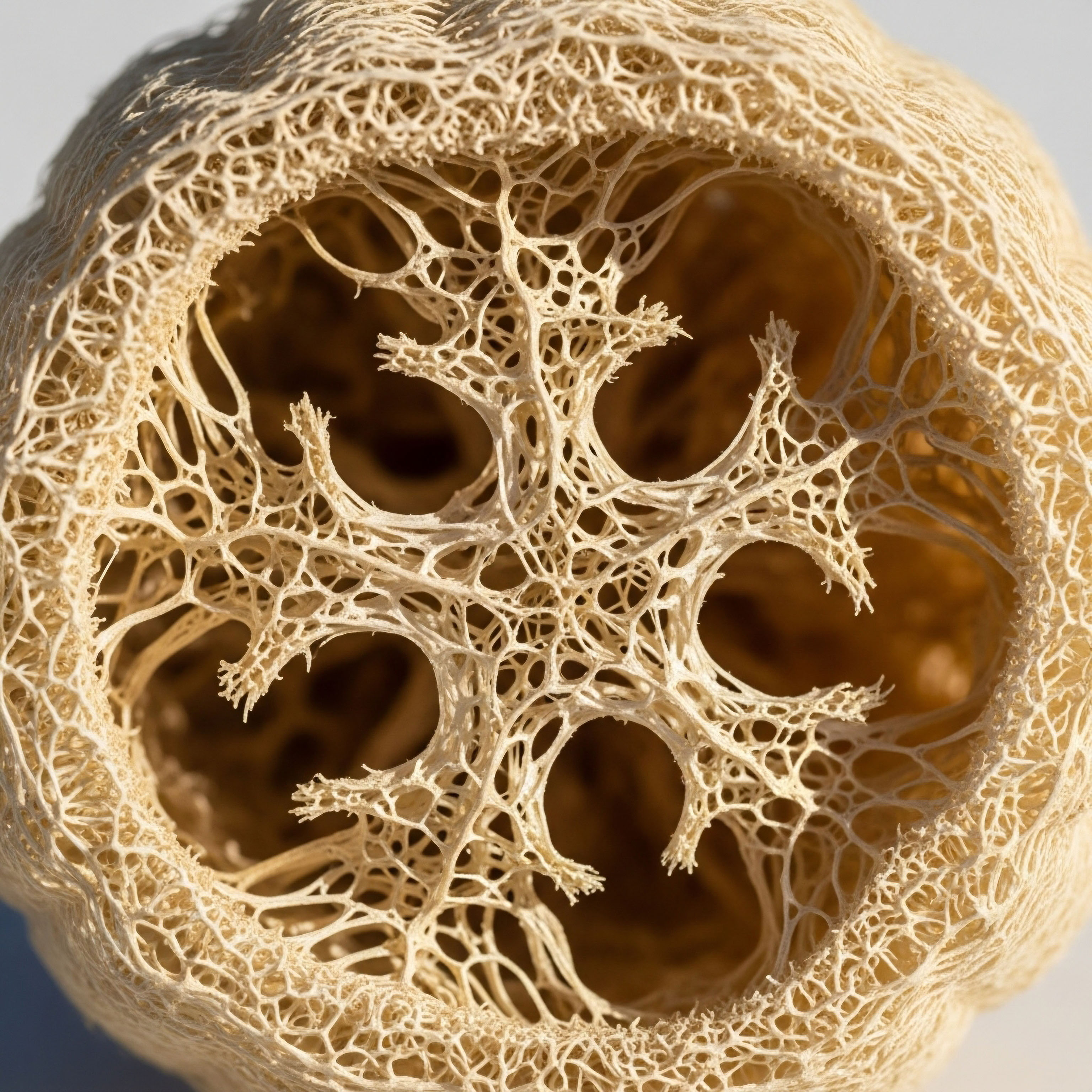
The conversation about health often revolves around diet and exercise, yet the subtle, powerful language of your body’s internal communication systems is frequently overlooked. At the center of this dialogue is your adipose tissue, which functions as a sophisticated and active endocrine organ. Its role extends far beyond simple energy storage; it is a primary regulator of your metabolic health, constantly sending and receiving messages that influence how every other cell in your body uses energy.
The core of this communication system relates to insulin sensitivity. Insulin is a hormone that acts like a key, unlocking your cells to allow glucose (sugar) to enter and be used for energy. When your cells are sensitive to insulin, this process is efficient.
A small amount of insulin produces a large effect, keeping your blood sugar stable and your energy levels consistent. Your adipose tissue produces and secretes a host of peptide hormones, collectively known as adipokines, that directly modulate how sensitive your cells are to insulin’s message. Think of these adipokines as molecular text messages sent from your fat cells to your muscles, liver, and brain, either amplifying or muffling the signal of insulin.

The Dual Nature of Adipose Communication
Your body’s adipose tissue is not a single, uniform entity. Its health and function determine the types of messages it sends. Healthy, functional adipose tissue releases peptides that promote metabolic flexibility and high insulin sensitivity. These beneficial adipokines act as allies to your metabolic system.
They help your liver and muscles respond appropriately to insulin, ensuring glucose is efficiently cleared from your bloodstream and used for immediate energy or stored properly for later use. This healthy state is characterized by lean adipose tissue that can grow by creating new fat cells (a process called hyperplasia) when needed, without becoming dysfunctional.
Conversely, when adipose tissue becomes stressed or overburdened, its communication style changes dramatically. This often happens when existing fat cells are forced to expand beyond their healthy capacity, a state known as hypertrophy. These enlarged, stressed fat cells begin to secrete a different class of adipokines.
These molecules are often pro-inflammatory and actively interfere with insulin signaling. They create a state of systemic, low-grade inflammation that contributes to insulin resistance, where your cells become deaf to insulin’s call. Your pancreas must then produce more and more insulin to achieve the same effect, a condition that can lead to a cascade of metabolic disturbances, including type 2 diabetes and cardiovascular issues.
Adipose tissue actively directs your body’s response to insulin by secreting powerful peptide messengers called adipokines.

Understanding Your Body’s Internal Dialogue
The journey to understanding your metabolic health begins with appreciating this internal dialogue. The symptoms you may be experiencing ∞ the stubborn weight gain, the energy slumps, the mental fog ∞ can be interpreted as the downstream consequences of this communication breakdown. Your adipose tissue is speaking a language, and its peptides are the words.
Learning to interpret this language is essential. The balance of these peptides provides a clear window into your metabolic state. It reflects the health of your adipose tissue and predicts your body’s ability to manage energy effectively. By focusing on the source of these signals, you can begin to influence the conversation, shifting the balance from messages of resistance and inflammation to those of sensitivity and metabolic harmony.
The glucose transporter protein GLUT4 is a critical component in this system. It is the primary gateway for glucose to enter muscle and fat cells, and its activity is directly commanded by insulin. When beneficial adipokines are abundant, they help ensure that GLUT4 is readily available at the cell surface to do its job.
When detrimental, inflammatory adipokines dominate, they disrupt the signaling chain that tells GLUT4 to move to the cell surface, leaving glucose trapped in the bloodstream. Therefore, the peptides released by your adipose tissue are not just passive bystanders; they are active participants in the fundamental mechanics of your daily energy regulation.


Intermediate
To truly grasp how adipose tissue peptides govern insulin sensitivity, we must categorize these molecular signals based on their function. The health of your metabolic system depends on the delicate balance between two opposing teams of adipokines. One team works to enhance insulin action and maintain metabolic order, while the other promotes inflammation and disrupts insulin signaling. The dominant team determines whether your body resides in a state of insulin sensitivity or resistance.

The Messengers of Metabolic Health
These are the adipokines that support and improve your body’s response to insulin. They are typically secreted by lean, healthy adipose tissue and are crucial for maintaining systemic energy balance.
- Adiponectin ∞ This is arguably the most important insulin-sensitizing peptide. Higher levels of adiponectin are strongly correlated with greater insulin sensitivity. It works directly on the liver to decrease glucose production and on skeletal muscle to increase glucose uptake and fatty acid oxidation. Adiponectin levels are paradoxically lower in individuals with obesity, a key factor in the development of insulin resistance.
- Leptin ∞ While primarily known as a satiety hormone that signals fullness to the brain, leptin also has significant effects on insulin sensitivity. By regulating appetite and energy expenditure, leptin helps prevent the excess calorie storage that leads to adipose tissue dysfunction. In a healthy system, leptin helps maintain a stable metabolic environment. However, in many cases of obesity, the brain becomes resistant to leptin’s signals, disrupting this regulatory function.
- Palmitoleic Acid (a Lipokine) ∞ While not a peptide, this fatty acid is synthesized and released by adipocytes and functions like a hormone. It has been shown to improve insulin sensitivity in both muscle and liver, and it suppresses inflammation within adipose tissue itself.
- Branched Fatty Acid Esters of Hydroxy Fatty Acids (FAHFAs) ∞ Discovered more recently, these lipid molecules are released from adipose tissue and have potent anti-inflammatory and insulin-sensitizing effects. Levels of FAHFAs are reduced in people with insulin resistance, and administering them to animal models improves glucose tolerance.

The Instigators of Insulin Resistance
When adipose tissue becomes hypertrophic and inflamed, it shifts its production toward peptides that antagonize insulin action. These adipokines create a self-perpetuating cycle of inflammation and metabolic dysfunction.
- Tumor Necrosis Factor-alpha (TNF-α) ∞ One of the first adipokines discovered to link obesity with insulin resistance. TNF-α is a pro-inflammatory cytokine that directly interferes with the insulin signaling pathway inside cells. It can disrupt the function of key signaling proteins, effectively blocking insulin’s message from being received.
- Interleukin-6 (IL-6) ∞ Another pro-inflammatory cytokine, IL-6 has complex roles. While it can have some beneficial effects during exercise, chronic elevation from dysfunctional adipose tissue contributes to systemic inflammation and insulin resistance, particularly in the liver.
- Resistin ∞ The role of resistin in humans is still being fully elucidated, but studies suggest it contributes to insulin resistance. Its name reflects its proposed action ∞ to resist insulin.
- Retinol Binding Protein 4 (RBP4) ∞ Elevated levels of RBP4 are associated with insulin resistance. It is thought to contribute to the problem by promoting inflammation and impairing insulin signaling in muscle and liver.
The ratio of insulin-sensitizing to insulin-resisting adipokines released from fat cells is a primary determinant of whole-body metabolic health.

Adipose Tissue Remodeling the Source of the Signal Shift
What causes adipose tissue to switch from secreting helpful peptides to harmful ones? The answer lies in how it responds to chronic energy surplus. Healthy adipose tissue expands through hyperplasia, which is the recruitment and differentiation of new, small, insulin-sensitive fat cells (preadipocytes). This process allows for safe lipid storage without stressing the existing cellular machinery.
In individuals prone to insulin resistance, this process is often impaired. Instead of creating new fat cells, the existing adipocytes are forced to enlarge, a process called hypertrophy. These bloated, hypertrophic cells become dysfunctional. They experience mechanical stress, oxygen deprivation (hypoxia), and cellular stress, which triggers an inflammatory response.
This inflamed state is what causes the shift in adipokine secretion, turning the adipose organ from a metabolic ally into an antagonist. This localized inflammation does not stay contained; it spills over into the systemic circulation, affecting the liver, muscles, and even the brain.

Comparative Profile of Adipose Peptides
The table below summarizes the primary function and metabolic impact of key peptides and lipids secreted by adipose tissue.
| Adipokine/Lipokine | Primary Function | Impact on Insulin Sensitivity | Typical Level in Obesity |
|---|---|---|---|
| Adiponectin | Enhances glucose uptake and fatty acid oxidation | Increases | Decreased |
| Leptin | Regulates satiety and energy expenditure | Increases (in sensitive states) | Increased (with resistance) |
| TNF-α | Promotes inflammation | Decreases | Increased |
| IL-6 | Promotes inflammation (when chronically elevated) | Decreases | Increased |
| RBP4 | Transports retinol, promotes inflammation | Decreases | Increased |
| FAHFAs | Reduces inflammation, improves glucose homeostasis | Increases | Decreased |

How Do Clinical Protocols Address This Imbalance?
Understanding this peptide-driven system opens new therapeutic avenues. For instance, therapies involving Testosterone Replacement Therapy (TRT) in men can improve body composition by reducing fat mass and increasing muscle mass. This change can lead to healthier adipose tissue that secretes a more favorable profile of adipokines, thereby improving insulin sensitivity.
Similarly, peptide therapies using agents like Sermorelin or Ipamorelin/CJC-1295 aim to optimize growth hormone levels. Growth hormone has a significant impact on lipolysis (the breakdown of fat), which can help reduce the burden on hypertrophic adipocytes and improve their function. The goal of these protocols is to recalibrate the body’s internal environment, fostering a state where the messages of metabolic health can once again be heard clearly.


Academic
A sophisticated analysis of how adipose-derived peptides regulate insulin sensitivity requires a deep examination of the molecular signaling cascades within target tissues, primarily skeletal muscle and the liver. The systemic metabolic phenotype is a direct reflection of the molecular crosstalk between the adipocyte and the hepatocyte or myocyte. This dialogue is governed by the activation and inhibition of specific intracellular pathways that converge on the insulin receptor signaling complex.

The Adiponectin-AMPK-PPARα Axis a Master Regulator of Insulin Sensitivity
Adiponectin stands out as a uniquely potent insulin-sensitizing adipokine. Its biological effects are mediated through its interaction with two principal receptors, AdipoR1 and AdipoR2, which are expressed abundantly in skeletal muscle and the liver, respectively. The binding of adiponectin to these receptors initiates a cascade of intracellular events, the most critical of which is the activation of AMP-activated protein kinase (AMPK).
AMPK functions as a cellular energy sensor. Its activation signals a low-energy state, triggering a switch from anabolic (energy-storing) to catabolic (energy-producing) processes. In skeletal muscle, AMPK activation by adiponectin stimulates two crucial metabolic events:
- GLUT4 Translocation ∞ Activated AMPK promotes the movement of GLUT4 glucose transporters from intracellular vesicles to the plasma membrane. This process is independent of the canonical insulin signaling pathway (PI3K-Akt), providing an alternative mechanism for glucose uptake into muscle cells. This is why adiponectin can enhance glucose clearance even in states of insulin resistance.
- Fatty Acid Oxidation ∞ AMPK phosphorylates and inactivates Acetyl-CoA Carboxylase (ACC), the rate-limiting enzyme in fatty acid synthesis. This action reduces the cellular concentration of malonyl-CoA, a potent inhibitor of carnitine palmitoyltransferase 1 (CPT1). With CPT1 uninhibited, long-chain fatty acids can be transported into the mitochondria for β-oxidation, thereby reducing intracellular lipid accumulation (lipotoxicity) which is a known contributor to insulin resistance.
In the liver, adiponectin’s activation of AMPK leads to the suppression of gluconeogenesis. It achieves this by inhibiting the expression of key gluconeogenic enzymes, such as phosphoenolpyruvate carboxykinase (PEPCK) and glucose-6-phosphatase (G6Pase). Concurrently, adiponectin signaling through AdipoR2 also activates the peroxisome proliferator-activated receptor-alpha (PPARα) pathway, which further enhances fatty acid oxidation and improves hepatic insulin sensitivity.

Inflammatory Adipokines the Molecular Sabotage of Insulin Signaling
Pro-inflammatory adipokines, such as TNF-α, secreted from hypertrophic, hypoxic adipocytes, directly antagonize insulin action at the molecular level. The primary mechanism of this interference is the disruption of the Insulin Receptor Substrate (IRS) proteins, particularly IRS-1. The canonical insulin signaling pathway proceeds as follows ∞ insulin binds to its receptor, leading to the receptor’s autophosphorylation on tyrosine residues. This activated receptor then phosphorylates IRS-1, also on tyrosine residues, creating docking sites for downstream signaling molecules like Phosphoinositide 3-kinase (PI3K).
TNF-α sabotages this process through the activation of inflammatory kinases, such as c-Jun N-terminal kinase (JNK) and IκB kinase (IKK). These kinases phosphorylate IRS-1 on serine residues instead of tyrosine residues. This serine phosphorylation of IRS-1 has two detrimental consequences:
- It acts as a steric hindrance, preventing the insulin receptor from properly docking with and phosphorylating IRS-1 on its tyrosine sites.
- It can target the IRS-1 protein for proteasomal degradation, effectively reducing the amount of this critical signaling molecule available in the cell.
The net result is a severe attenuation of the insulin signal. The PI3K-Akt pathway is not sufficiently activated, leading to failed GLUT4 translocation in muscle and a failure to suppress gluconeogenesis in the liver. This molecular mechanism is a central cause of the insulin resistance observed in obesity and type 2 diabetes.
Inflammatory adipokines induce insulin resistance by promoting serine phosphorylation of IRS-1, which effectively blocks the transmission of the insulin signal.

What Is the Role of Genetic Predisposition in Adipose Signaling?
Genetic factors play a significant role in determining an individual’s adipose tissue function and subsequent risk for insulin resistance. Variants in genes like Transcription Factor 7-Like 2 (TCF7L2) and Peroxisome Proliferator-Activated Receptor-Gamma (PPAR-γ) are strongly associated with type 2 diabetes risk. TCF7L2 is highly expressed in adipose tissue and is involved in adipogenesis.
Certain variants of TCF7L2 are linked to impaired preadipocyte differentiation, predisposing an individual to adipocyte hypertrophy and the subsequent inflammatory state. PPAR-γ is a master regulator of adipogenesis. While its activation generally promotes the formation of new, healthy fat cells, certain genetic variants can alter its function, influencing fat storage capacity and insulin sensitivity. These genetic predispositions highlight that the response of adipose tissue to caloric excess is not uniform across all individuals.

Molecular Actions of Key Adipose-Derived Factors
The following table provides a detailed overview of the molecular mechanisms of action for selected adipokines and lipokines.
| Factor | Receptor/Target | Key Downstream Mediator | Net Effect on Insulin Signaling |
|---|---|---|---|
| Adiponectin | AdipoR1/AdipoR2 | AMPK, PPARα | Potentiates (via PI3K-independent and dependent pathways) |
| TNF-α | TNFR1 | JNK, IKK | Inhibits (via serine phosphorylation of IRS-1) |
| IL-6 | IL-6R/gp130 | STAT3, SOCS3 | Inhibits (via SOCS3-mediated degradation of IRS-1) |
| RBP4 | STRA6 | JNK | Inhibits (via inflammatory pathway activation) |
| PAHSAs | GPR120 | Anti-inflammatory pathways | Potentiates (by reducing background inflammation) |
This intricate network of signaling pathways underscores the profound influence of adipose tissue on systemic homeostasis. The peptide and lipid messengers it releases are not merely biomarkers; they are bioactive modulators that dictate the efficiency of insulin action throughout the body.
Therapeutic interventions, including hormonal optimization with testosterone or growth hormone secretagogues, can be viewed as strategies to fundamentally alter the secretome of the adipocyte, shifting the balance from a pro-inflammatory, insulin-resistant state to an anti-inflammatory, insulin-sensitive one. This represents a shift from treating the symptoms of metabolic disease to addressing its root cause at the level of intercellular communication.

References
- Smith, U. & Kahn, B. B. (2016). Adipose tissue regulates insulin sensitivity ∞ role of adipogenesis, de novo lipogenesis and novel lipids. Diabetologia, 59(12), 2637 ∞ 2649.
- Czech, M. P. (2017). Insulin action in adipocytes, adipose remodeling, and systemic effects. Cell, 171(1), 113-126.
- Trakakis, E. & Karkalousos, P. (2023). Lipid Hormones at the Intersection of Metabolic Imbalances and Endocrine Disorders. Metabolites, 13(5), 659.
- Grippo, C. & D’Abbondanza, M. (2022). The Complex Gene ∞ Carbohydrate Interaction in Type 2 Diabetes ∞ Between Current Knowledge and Future Perspectives. Nutrients, 14(21), 4692.
- Reaven, G. M. (2008). Adipose Tissue Response to Overfeeding in Insulin Resistance-Prone vs. Insulin Sensitive Humans. Stanford University.
- Yore, M. M. Syed, I. Moraes-Vieira, P. M. Zhang, T. Herman, M. A. Homan, E. A. & Kahn, B. B. (2014). Discovery of a class of endogenous mammalian lipids with anti-diabetic and anti-inflammatory effects. Cell, 159(2), 318-332.
- Abel, E. D. Peroni, O. Kim, J. K. Kim, Y. B. Boss, O. Hadro, E. & Kahn, B. B. (2001). Adipose-selective targeting of the GLUT4 gene impairs insulin action in muscle and liver. Nature, 409(6821), 729-733.
- Gustafson, B. Hedjazifar, S. Gogg, S. Hammarstedt, A. & Smith, U. (2015). Insulin resistance and impaired adipogenesis. Trends in Endocrinology & Metabolism, 26(4), 193-200.

Reflection
You have now seen the intricate biological blueprint that connects your adipose tissue to your overall sense of well-being. The science provides a powerful framework, translating feelings of fatigue or frustration into a clear language of cellular communication. This knowledge is the starting point.
It shifts the perspective from one of fighting against your body to one of listening to it and understanding its needs. Your body is not your adversary; it is a complex, responsive system striving for balance.

What Is Your Body’s Next Message?
Consider the information presented here as a map. It shows the territory of your metabolic health, detailing the pathways and messengers involved. A map, however, only shows the landscape. It does not dictate your specific path. Your personal health journey is unique, shaped by your genetics, your history, and your life.
The next step involves using this map to ask more personalized questions. How does your own internal dialogue sound? Are the signals of sensitivity and efficiency being broadcast clearly, or are they being drowned out by the noise of inflammation and resistance? This process of introspection, guided by an understanding of the underlying biology, is where true empowerment begins. It is the moment you move from being a passenger to being the pilot of your own health.



