

Fundamentals
The moment a treatment plan involving a Gonadotropin-Releasing Hormone (GnRH) analog is presented, the world can seem to shrink to a single point of focus. Your primary health concern, whether it is endometriosis, uterine fibroids, or prostate cancer, requires a powerful intervention. You feel a sense of resolve in taking a definitive step.
Yet, alongside this, a cascade of new questions and quiet anxieties begins. You may have heard stories or read pamphlets that speak of side effects in clinical terms, but the lived reality of this therapeutic path is what concerns you most.
You are not just a diagnosis; you are a person whose daily vitality, energy, and sense of self are paramount. The question of how to protect your body’s intricate metabolic machinery during this process is a profound one. It is an inquiry that moves past the immediate goal of treatment toward the preservation of your long-term wellness.
This feeling of being at a biological crossroads is entirely valid. The therapy you are undertaking works by quieting a fundamental communication system within your body ∞ the dialogue between the brain and the gonads. This system, the Hypothalamic-Pituitary-Gonadal (HPG) axis, is the master regulator of reproductive hormones.
GnRH analogs function by binding to receptors in the pituitary gland, a small, powerful organ at the base of the brain. This action leads to a profound reduction in the production of sex hormones like estrogen and testosterone. This hormonal silence is the therapeutic goal. It starves hormone-sensitive tissues, providing relief and control.
The experience of this internal quiet, however, extends throughout your entire physiology. These hormones are messengers with system-wide responsibilities, and their absence is felt far beyond the reproductive system. They are deeply involved in regulating how your body uses and stores energy, maintains muscle, and manages lipids.
The fatigue, the subtle shifts in your body composition, the changes in your mood ∞ these are not isolated inconveniences. They are the downstream effects of a systemic hormonal recalibration. Understanding this connection is the first step toward actively supporting your body through this transition.

The Body’s Internal Economy
Think of your metabolism as a complex and finely tuned internal economy. It governs energy production, resource allocation, and waste management. The sex hormones, estrogen and testosterone, act as key regulators within this economy. They influence insulin sensitivity, which is how efficiently your cells take up glucose from the blood for energy.
They direct the body to build and maintain lean muscle mass, which is a metabolically active tissue that burns calories even at rest. They also play a direct role in how your liver processes fats, affecting the levels of cholesterol and triglycerides in your bloodstream. When GnRH analog treatment significantly lowers the levels of these hormones, it is like removing a major economic regulator. The system must adapt, and this adaptation can manifest as a collection of metabolic shifts.
Your body, in its inherent wisdom, seeks a new equilibrium. Without the strong signal from estrogen or testosterone to maintain muscle, it may begin to favor fat storage, particularly in the abdominal area. This is a common experience and a source of significant distress for many.
The way your cells respond to insulin can also change. They may become less sensitive, requiring your pancreas to work harder to produce more insulin to keep blood sugar levels stable. This condition, known as insulin resistance, is a central feature of metabolic disruption.
Simultaneously, your liver’s handling of lipids can be altered, potentially leading to changes in your cholesterol profile. These are not signs of failure on your part. They are the predictable physiological responses to a low-hormone state. Your body is operating according to a new set of rules. The objective, therefore, is to learn these new rules and provide targeted support that helps your internal economy function as smoothly as possible under these new circumstances.
The metabolic changes experienced during GnRH analog therapy are direct physiological responses to a medically induced low-hormone state.

What Are the Primary Metabolic Adjustments?
The adjustments your body makes during GnRH analog treatment are multifaceted and interconnected. While the specifics can vary from person to person, several core patterns of metabolic change are consistently observed. Recognizing these patterns allows for a more focused and effective support strategy. The journey begins with acknowledging the biological reality of what is occurring within your cells and systems.
These shifts are not your fault; they are a direct consequence of the therapy’s mechanism of action. Each one represents a point of intervention, an opportunity to provide your body with the resources it needs to navigate this period of change with resilience.
- Body Composition Changes ∞ There is a distinct tendency for the body to lose lean muscle mass and gain adipose tissue, or fat. This occurs because both estrogen and testosterone send anabolic signals to muscle tissue, promoting its growth and maintenance. When these signals are withdrawn, the balance tips toward a catabolic state, where muscle is more easily broken down. Concurrently, the hormonal environment becomes more conducive to fat storage.
- Insulin Sensitivity Reduction ∞ The body’s cells, particularly muscle and fat cells, can become less responsive to the hormone insulin. Insulin’s job is to unlock the door to cells so they can absorb glucose from the blood. When cells become resistant, glucose remains in the bloodstream longer, prompting the pancreas to release even more insulin. This state of high insulin and potential for elevated blood sugar is a key metabolic concern.
- Altered Lipid Profiles ∞ The liver’s processing of fats is influenced by sex hormones. GnRH analog treatment can lead to an increase in triglycerides and changes in cholesterol levels. Specifically, low-density lipoprotein (LDL) cholesterol may rise, while high-density lipoprotein (HDL) cholesterol, which is protective, may also see changes. Monitoring these markers is a standard part of managing care during this therapy.
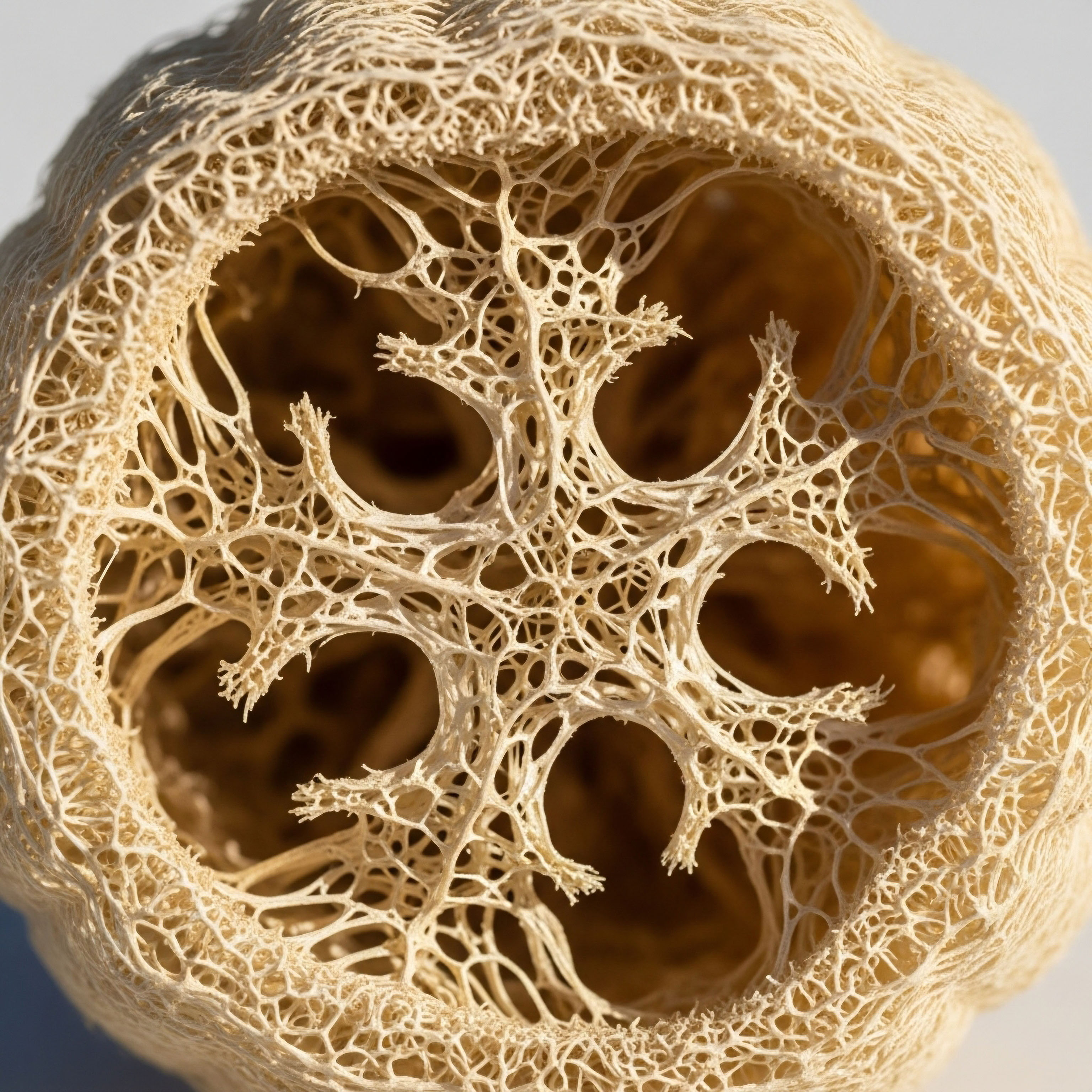
- Bone Metabolism Disruption ∞ Estrogen is a powerful protector of bone density. By suppressing the activity of cells that break down bone (osteoclasts), it maintains skeletal strength. The profound hypoestrogenism induced by GnRH analogs removes this protective brake, increasing the risk of bone mineral loss over time. This is a critical consideration, especially for long-term treatment protocols.
Each of these points represents a piece of a larger puzzle. They are not separate issues but rather interconnected aspects of a single, system-wide adaptation to a low-hormone environment. By understanding them individually, you can begin to see the logic behind the supportive strategies that will be discussed, from nutritional adjustments to specific types of physical activity. Your path forward is one of conscious, informed action designed to work with your body’s new operational reality.


Intermediate
Navigating the metabolic landscape during GnRH analog treatment requires a proactive and informed stance. It involves moving beyond a simple acknowledgment of the side effects toward a strategic implementation of countermeasures. The core principle guiding this approach is the recognition that while the therapy-induced hormonal deficiency is the catalyst for metabolic changes, it does not leave the body without recourse.
We can introduce targeted inputs ∞ through nutrition, specific forms of exercise, and, in many cases, a judicious use of hormonal support ∞ to mitigate these effects. This is about actively managing your internal environment to preserve function and well-being.
The central strategy often involves a concept known as “add-back therapy” (ABT). This approach is elegant in its logic ∞ while the GnRH analog powerfully suppresses the body’s own production of high levels of sex hormones to treat the underlying condition, ABT provides just enough hormonal support to protect other systems, like bones and metabolism, from the most severe consequences of that suppression.
It is a balancing act. The goal is to administer a dose of estrogen (with a progestin in women with a uterus) or testosterone that is high enough to alleviate side effects like hot flashes and prevent bone loss, yet low enough that it does not reactivate the condition being treated.
This method allows for the extension of GnRH analog therapy beyond the typical six-month limitation often imposed due to concerns like osteoporosis. It represents a sophisticated clinical approach that separates the therapeutic effect of hormonal suppression from its unwanted systemic consequences.

Implementing Add-Back Therapy a Clinical Overview
The decision to initiate add-back therapy is a collaborative one, made between you and your healthcare provider. It is based on the duration of your GnRH analog treatment, the severity of your symptoms, and your individual health profile. The protocols are well-established and aim to replicate a more balanced, albeit low-level, hormonal state. This intervention directly addresses the root cause of the metabolic disturbances ∞ the absence of hormonal signaling.
The selection of the specific add-back regimen is tailored to the individual. For women, this typically involves a combination of a low-dose estrogen and a progestin. For men undergoing treatment for prostate cancer, a low dose of testosterone may be considered in specific clinical contexts, though this is a more complex decision. The table below outlines some common add-back approaches, highlighting their components and primary metabolic targets.
| Add-Back Protocol | Hormonal Components | Primary Metabolic Goals | Key Considerations |
|---|---|---|---|
| Estrogen-Progestin Therapy (Women) | Low-dose estradiol (oral, transdermal); Norethindrone acetate or other progestin. | Preserve bone mineral density; Mitigate vasomotor symptoms (hot flashes); Support lipid profile stability. | The progestin component is essential for protecting the uterine lining from stimulation by estrogen. |
| Tibolone (Women) | A synthetic steroid with estrogenic, progestogenic, and androgenic properties. | Addresses hypoestrogenic symptoms; May have a favorable effect on libido due to its androgenic properties; Protects bone. | Its tissue-specific activity provides a broad spectrum of symptom relief. |
| Testosterone Add-Back (Men) | Low-dose testosterone (injection or gel). | Preserve lean muscle mass; Counteract fat gain; Support insulin sensitivity; Improve energy and mood. | This is carefully considered in the context of prostate cancer treatment to ensure it does not compromise therapeutic outcomes. |
| Selective Estrogen Receptor Modulators (SERMs) | Agents like Raloxifene. | Primarily focused on preserving bone density. | SERMs have estrogen-like effects on bone but can block estrogen’s effects in other tissues like the breast and uterus. |
The implementation of ABT transforms the experience of GnRH analog treatment. It provides a buffer against the most disruptive metabolic effects, allowing you to maintain a higher quality of life and physiological function throughout the therapeutic course. It is a clear example of how modern endocrinology seeks to create highly targeted treatments that maximize benefits while actively managing and minimizing systemic costs.

Nutritional Protocols for Metabolic Resilience
While add-back therapy addresses the hormonal signaling deficit, nutritional strategy provides the raw materials your body needs to maintain metabolic balance. The dietary approach during GnRH analog treatment is one of precision and intention. It aims to directly counteract the known metabolic shifts ∞ insulin resistance, muscle loss, and altered lipid profiles. This is not about restrictive dieting; it is about strategic fueling.
The architecture of your diet should be built around three pillars ∞ protein adequacy, fiber richness, and smart fat selection. Each pillar supports a specific aspect of your metabolic health, creating a synergistic effect that enhances your body’s resilience.

The Primacy of Protein
In a low-hormone environment, the body’s signal to maintain muscle is weakened. Providing a consistent and sufficient supply of high-quality protein is the most effective way to counteract this catabolic tendency. Protein provides the amino acids, the building blocks, necessary for muscle repair and synthesis.
Aiming for a higher protein intake sends a strong anabolic (building) signal to your muscles, helping to preserve lean mass. This is critically important because muscle is a primary site of glucose disposal. The more muscle you have, the more efficiently your body can manage blood sugar, which directly combats insulin resistance.
- Target Intake ∞ A general guideline is to consume 1.2 to 1.6 grams of protein per kilogram of your body weight. Distributing this intake evenly throughout the day, with 25-30 grams per meal, is an effective strategy for stimulating muscle protein synthesis continuously.
- Quality Sources ∞ Focus on complete proteins that contain all essential amino acids. These include lean meats, poultry, fish, eggs, and dairy products. For those following plant-based diets, combining sources like lentils and rice, or utilizing high-quality protein powders from soy, pea, or a blend, is essential.

Fiber the Unsung Metabolic Hero
Fiber is a powerful tool for managing both blood sugar and lipid levels. Soluble fiber, found in oats, barley, nuts, seeds, beans, and some fruits like apples and citrus, forms a gel-like substance in the digestive tract. This gel slows down the absorption of sugar, preventing sharp spikes in blood glucose and reducing the burden on the pancreas.
It also binds to bile acids in the gut, which are made from cholesterol, and helps excrete them from the body. This process prompts the liver to pull more cholesterol from the bloodstream to make new bile acids, thereby helping to lower LDL cholesterol levels.
Insoluble fiber, found in whole grains and vegetables, adds bulk to the stool and promotes regular bowel movements, which is important for overall gut health and detoxification. A high-fiber diet contributes to satiety, helping you feel full and satisfied, which can aid in managing body weight.
A diet rich in protein and fiber provides the foundational support needed to maintain muscle mass and stabilize blood sugar during treatment.

Why Must Exercise Be Non-Negotiable?
If nutrition provides the building blocks, exercise provides the stimulus. Physical activity is an indispensable component of any plan to support metabolic health during GnRH analog therapy. Its benefits are systemic and directly counter the primary adverse effects of treatment. The right kind of exercise can improve insulin sensitivity, drive the maintenance of lean body mass, strengthen bones, and improve mental well-being. The key is a combination of resistance training and cardiovascular work.

Resistance Training the Anabolic Signal
Resistance training is the most potent non-hormonal stimulus for muscle maintenance and growth. When you lift weights, use resistance bands, or perform bodyweight exercises, you create microscopic tears in your muscle fibers. The body’s repair process not only fixes these tears but also adapts by making the muscles stronger and more resilient. This process is inherently anabolic and provides a powerful counterbalance to the catabolic environment created by GnRH analog therapy.
Furthermore, the act of muscle contraction during exercise has an insulin-like effect. It can stimulate glucose uptake from the blood into the muscles through pathways that do not require insulin. This means that every session of resistance training makes your body better at managing blood sugar, directly improving insulin sensitivity. A typical plan would involve 2-3 full-body sessions per week, focusing on compound movements like squats, deadlifts, presses, and rows that engage multiple large muscle groups.

Cardiovascular Exercise for Systemic Health
Cardiovascular exercise complements resistance training by improving the health of your heart and blood vessels and further enhancing insulin sensitivity. There are different modalities to consider:
- Zone 2 Training ∞ This involves sustained, low-to-moderate intensity activity (like brisk walking, jogging, or cycling) where you can still hold a conversation. It is particularly effective at improving mitochondrial function ∞ the energy factories within your cells ∞ and enhancing your body’s ability to burn fat for fuel.
- High-Intensity Interval Training (HIIT) ∞ HIIT involves short bursts of all-out effort followed by brief recovery periods. It is exceptionally time-efficient and has been shown to provide significant improvements in insulin sensitivity and cardiovascular fitness. A HIIT session might be added once a week to a well-established fitness base.
The combination of resistance training to preserve the body’s metabolic engine (muscle) and cardiovascular exercise to improve the efficiency of the fuel delivery system creates a robust defense against the metabolic consequences of a low-hormone state. This integrated approach of add-back therapy, targeted nutrition, and a structured exercise plan offers a comprehensive strategy for reclaiming a sense of control and vitality during your treatment.

Academic
The administration of a Gonadotropin-Releasing Hormone (GnRH) analog initiates a cascade of predictable and profound endocrinological changes, culminating in a state of iatrogenic hypogonadism. From a systems-biology perspective, this intervention represents a targeted disruption of the Hypothalamic-Pituitary-Gonadal (HPG) axis, the consequences of which propagate throughout numerous interconnected physiological networks.
While the primary therapeutic benefit is derived from the suppression of gonadal steroids, the secondary metabolic sequelae are of significant clinical importance. A sophisticated understanding of these effects requires an examination of the molecular mechanisms that govern energy homeostasis and how they are perturbed by the withdrawal of sex hormones.
The metabolic phenotype induced by GnRH analogs shares characteristics with, yet is distinct from, the classic metabolic syndrome. Both states involve increased adiposity and impaired insulin sensitivity. The changes driven by GnRH analogs, however, present a unique biochemical signature.
For instance, in men treated for prostate cancer, studies have shown that while fat mass increases, it is predominantly an expansion of subcutaneous adipose tissue (SAT) rather than visceral adipose tissue (VAT). This is a critical distinction, as VAT is more strongly associated with cardiometabolic risk.
Concurrently, and somewhat paradoxically, levels of adiponectin, an adipokine known for its insulin-sensitizing and anti-inflammatory properties, have been observed to increase. This finding stands in contrast to the low adiponectin levels typically seen in obesity-related insulin resistance. These nuances suggest that the metabolic dysregulation from chemically induced hypogonadism follows a different pathophysiological trajectory, necessitating a tailored and mechanistically informed approach to management.

Molecular Underpinnings of Insulin Resistance
The decrease in insulin sensitivity observed during GnRH analog therapy is a central node in the network of metabolic disruption. At the cellular level, both estrogen and testosterone potentiate the insulin signaling cascade. Testosterone, for example, is known to enhance the expression and translocation of the GLUT4 glucose transporter in skeletal muscle, the primary tissue responsible for postprandial glucose disposal. The withdrawal of testosterone attenuates this process, leading to a reduction in glucose uptake capacity.
Estrogen receptors are also present in key metabolic tissues, including the pancreas, liver, adipose tissue, and skeletal muscle. Estrogen’s role is complex, influencing beta-cell function in the pancreas and hepatic glucose output. Its absence can lead to a less efficient insulin response and an increase in gluconeogenesis by the liver.
The resulting hyperinsulinemia is a compensatory mechanism that, over time, can lead to beta-cell fatigue and a further worsening of glycemic control. The HOMA-IR (Homeostatic Model Assessment for Insulin Resistance) index, a calculation based on fasting glucose and insulin, often shows a significant increase during GnRH analog treatment, providing a quantitative measure of this decline in insulin sensitivity.
Supporting these pathways through interventions that bypass the need for hormonal signaling, such as exercise-induced GLUT4 translocation, becomes a rational and evidence-based strategy.

Dyslipidemia and Adipose Tissue Remodeling
The lipid profile alterations seen with GnRH analog therapy are a direct result of changes in hepatic lipid metabolism and adipose tissue function. Estrogen, for instance, generally promotes a favorable lipid profile by increasing HDL cholesterol and lowering LDL cholesterol. Its withdrawal reverses these effects. The increase in triglycerides is often linked to increased de novo lipogenesis in the liver, driven by the state of insulin resistance.
The following table details findings from select studies investigating the metabolic impact of GnRH analog therapy, providing a granular view of the specific changes observed across different patient populations and treatment contexts. This data underscores the consistency of the metabolic phenotype while also highlighting the subtle variations that inform a more precise clinical approach.
| Study Population | GnRH Analog Used | Key Metabolic Findings | Reference |
|---|---|---|---|
| Men with Prostate Cancer | Leuprolide | Significant increase in fat mass, waist circumference, and serum triglycerides. Decrease in insulin sensitivity. Increase in HDL cholesterol and adiponectin. No change in blood pressure or C-reactive protein. | Basaria et al. |
| Children with Central Precocious Puberty | Triptorelin | Increase in BMI-SDS and HOMA index during treatment. Deterioration in LDL/HDL ratio. These effects were observed to be reversible after treatment discontinuation. | Iughetti et al. |
| Women with Uterine Fibroids | Goserelin | Significant bone mineral loss without add-back therapy. Increased incidence of hypoestrogenic side effects (hot flashes) impacting quality of life. | Sankaran et al. |
| General Gynaecological Use | Prostap / Zoladex | Alterations in blood sugar levels, potentially affecting control in diabetic patients. Changes in blood lipids (cholesterol). | Manchester University NHS Foundation Trust |

Can We Modulate These Effects with Advanced Therapies?
Beyond conventional add-back therapy and lifestyle modifications, there is a growing interest in the potential role of other therapeutic agents, such as growth hormone secretagogues (GHS), in mitigating the adverse body composition changes associated with GnRH analog treatment.
Peptides like Sermorelin or the combination of Ipamorelin and CJC-1295 stimulate the patient’s own pituitary gland to release pulses of growth hormone. Growth hormone has powerful effects on body composition, promoting lipolysis (fat breakdown) and the synthesis of lean muscle mass. Its effects are, in many ways, directly antagonistic to the changes induced by sex hormone deficiency.
The clinical rationale is compelling. By providing a separate anabolic signal through the GH/IGF-1 axis, it may be possible to preserve muscle mass and prevent the accumulation of fat mass more effectively than with lifestyle measures alone. This could be particularly beneficial for patients on long-term GnRH analog therapy who are at higher risk for sarcopenia and functional decline.
This represents a forward-thinking, systems-based approach. It acknowledges the primary hormonal deficit created by the treatment and introduces a targeted, secondary intervention to support a different, yet complementary, anabolic pathway. Such an approach moves clinical practice toward a more holistic model of managing the consequences of powerful endocrine therapies, aiming to preserve not just life, but function and vitality.

References
- Sankaran, S. & Manyonda, I. T. (2008). Current approaches to overcome the side effects of GnRH analogs in the treatment of patients with uterine fibroids. Obstetrics and Gynecology International, 2008, 196134.
- Manchester University NHS Foundation Trust. (2019). GnRH analogue injections. Patient Information Leaflet.
- Basaria, S. Muller, D. C. Carducci, M. A. Egan, J. & Dobs, A. S. (2006). Metabolic changes during gonadotropin-releasing hormone agonist therapy for prostate cancer ∞ differences from the classic metabolic syndrome. Cancer, 107(12), 2793 ∞ 2800.
- Iughetti, L. Bruzzi, P. Bigi, E. Valeri, L. Manzotti, E. & Predieri, B. (2016). The Metabolic Negative Effect of Gonadotropin-Releasing Hormone Agonist Therapy in Childhood ∞ Is it Short-Term and Reversible?. Endocrine Abstracts, 41, P1-P36.
- Society for Assisted Reproductive Technology. (n.d.). GnRH Agonist Therapy. SART.

Reflection
You have now seen the biological logic that connects your treatment to the changes you may be feeling in your body. You understand that the fatigue, the shifts in your physical form, and the altered sense of metabolic wellness are not random occurrences but predictable consequences of a powerful and necessary therapy.
This knowledge itself is a form of power. It moves you from a position of passive experience to one of active partnership in your own care. The path you are on is a temporary state, a deliberate recalibration of your internal environment for a specific therapeutic purpose.
Consider for a moment the resilience of your own physiology. It is a system that constantly adapts, seeking balance under changing conditions. The strategies outlined here ∞ the nutritional adjustments, the specific forms of movement, the potential for hormonal support ∞ are not just items on a checklist.
They are tools you can use to guide that adaptation. They are ways of communicating with your body in a language it understands ∞ the language of amino acids, of glucose uptake, of muscular contraction, of hormonal signals.
What does vitality mean to you, and how can you actively cultivate it, even now? The journey through GnRH analog treatment is a finite one. The insights you gain about your own body, however, will last a lifetime.
This period can be an opportunity for a deeper education in your own biology, a chance to learn how to support your systems with precision and care. The ultimate goal is to emerge from this treatment not just having addressed a primary health concern, but with a new level of understanding and a renewed commitment to the stewardship of your own well-being.

Glossary

gonadotropin-releasing hormone

prostate cancer

side effects

gnrh analogs

sex hormones

body composition

insulin sensitivity

gnrh analog treatment

lean muscle mass

insulin resistance

blood sugar

during gnrh analog treatment

adipose tissue

lean muscle

gnrh analog

hypoestrogenism

during gnrh analog

add-back therapy

gnrh analog therapy

metabolic health

during gnrh analog therapy

resistance training

lipid profile

muscle mass




