

Fundamentals
You feel it as a subtle shift in your body’s internal landscape. It might be a persistent fatigue that sleep doesn’t resolve, a new difficulty in managing your weight, or a sense of fogginess that clouds your thoughts after a meal.
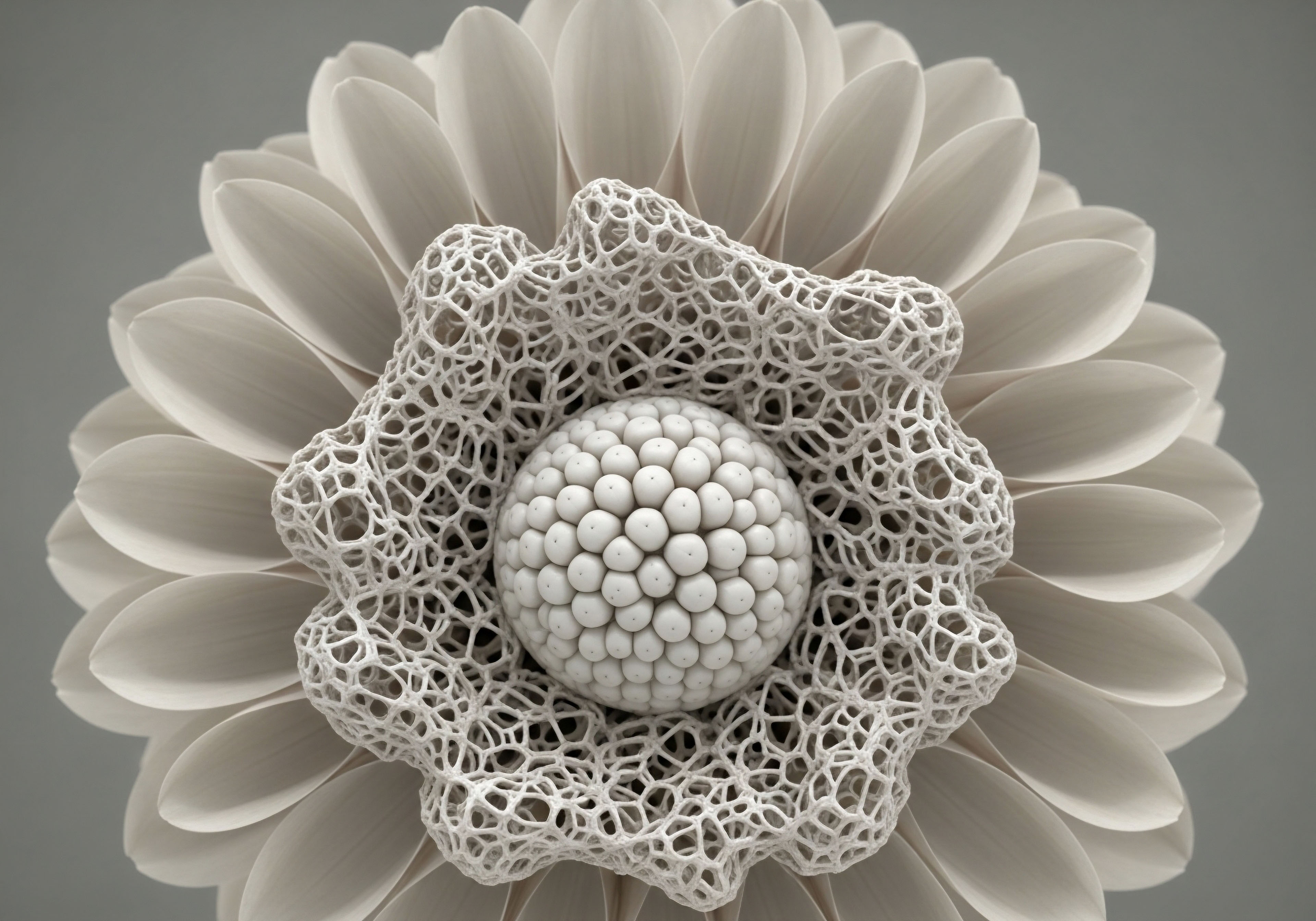
These experiences are valid and real signals from your body, whispers of a deeper conversation happening within your metabolic systems. At the center of this dialogue is a collection of microscopic powerhouses, the pancreatic beta cells. Your lived experience of energy, clarity, and vitality is profoundly connected to the health and function of these remarkable cells. Understanding their role is the first step toward reclaiming control over your biological journey.
Imagine your pancreatic beta cells as a highly specialized, intelligent manufacturing hub. Their sole purpose is to produce and secrete insulin, the hormone that acts as a key, unlocking your body’s cells to allow glucose ∞ your primary fuel source ∞ to enter and provide energy. This process is one of exquisite biological precision.
The beta cells constantly monitor your bloodstream, releasing just enough insulin to manage the glucose from your food. When this system is functioning optimally, you experience stable energy, mental sharpness, and metabolic equilibrium. The vitality you feel is a direct reflection of this seamless, internal choreography.
The health of your pancreatic beta cells is the foundation of your body’s ability to manage energy and maintain metabolic balance.
The challenge arises when this system is placed under chronic stress. A diet high in processed carbohydrates, a sedentary lifestyle, persistent stress, and age-related hormonal changes can all contribute to a state of insulin resistance. In this scenario, your body’s cells become less responsive to insulin’s message.
The key no longer fits the lock as easily. Your beta cells, in their dedication to maintaining balance, respond by working harder, producing more and more insulin to overcome this resistance. This sustained overproduction leads to what is known as beta-cell exhaustion. They become fatigued, their functional capacity diminishes, and some may eventually cease to function altogether. The symptoms you experience are the external manifestation of this internal struggle.
This is where the concept of peptide therapies enters the conversation, offering a way to support and potentially restore the function of these vital cells. Peptides are small chains of amino acids, which are the fundamental building blocks of proteins. They act as signaling molecules, carrying specific messages between cells and tissues.
Your body naturally produces thousands of different peptides to regulate a vast array of biological functions, from digestion to immune response to hormone production. Peptide therapies utilize specific, often bioidentical, peptides to re-establish clear communication within these systems. They represent a method of working with the body’s own language to promote healing and restore optimal function, speaking directly to the cells involved and reminding them of their inherent roles.

What Is the Core Function of Pancreatic Beta Cells?
The primary and most critical function of pancreatic beta cells is the synthesis and secretion of insulin in response to blood glucose levels. These cells are located in clusters within the pancreas called the islets of Langerhans. Following a meal, as glucose is absorbed into the bloodstream, the beta cells detect this rise and release stored insulin.
This hormonal signal is essential for glucose homeostasis, as it instructs cells in the muscles, liver, and fat tissue to absorb glucose from the blood for energy or storage. This elegant feedback loop is central to metabolic health, preventing the damaging effects of prolonged high blood sugar. A secondary function of these cells is the co-secretion of other molecules, like C-peptide and amylin, which also play roles in glucose regulation and satiety.

Understanding Cellular Stress and Its Impact
When beta cells are subjected to chronic high demand due to insulin resistance, they enter a state of significant physiological stress. This stress manifests in several ways at the cellular level. One key aspect is endoplasmic reticulum (ER) stress. The ER is the cellular machinery responsible for folding proteins, including insulin.
When insulin production is in overdrive, the ER can become overwhelmed, leading to an accumulation of misfolded proteins. This triggers a cellular stress response that, if prolonged, can activate pathways leading to apoptosis, or programmed cell death. Concurrently, high glucose levels themselves can be toxic to beta cells, a phenomenon known as glucotoxicity, which further impairs their function and promotes their demise. This cascade of events creates a self-perpetuating cycle of declining beta-cell mass and worsening metabolic control.


Intermediate
Moving beyond the foundational understanding of beta cell function, we can examine the specific mechanisms through which certain peptide therapies can exert a positive influence. The most well-researched and clinically significant class of peptides in this domain are the Glucagon-Like Peptide-1 (GLP-1) receptor agonists.
These therapies are based on a naturally occurring incretin hormone, GLP-1, which your intestines release after you eat. It is a key player in a sophisticated gut-brain communication axis that orchestrates your body’s response to incoming nutrients. By mimicking and amplifying the action of this natural hormone, GLP-1 receptor agonists provide a multi-pronged approach to supporting beta cell health and improving metabolic regulation.
The primary action of GLP-1 agonists is to stimulate insulin secretion in a glucose-dependent manner. This is a crucial distinction. They only prompt the beta cells to release insulin when blood glucose levels are elevated, such as after a meal.
This “smart” signaling prevents the excessive insulin release that can occur in states of insulin resistance and reduces the risk of hypoglycemia (low blood sugar). This intelligent action alleviates a significant portion of the chronic workload placed on the beta cells, giving them a much-needed respite.
Furthermore, these peptides simultaneously suppress the release of glucagon, a hormone that signals the liver to produce more glucose. By quieting this opposing signal, they contribute to a more stable and controlled blood sugar environment, further reducing the demand on the beta cells.
GLP-1 based peptide therapies work by mimicking the body’s natural post-meal signals to intelligently regulate insulin release and protect beta cells from exhaustion.

Direct Protective Effects on Beta Cells
The influence of GLP-1 receptor agonists extends far beyond simply managing glucose levels. Clinical and preclinical studies have demonstrated that these peptides have direct protective and potentially restorative effects on the beta cells themselves. They appear to interact with cellular pathways that promote beta cell proliferation, which is the process of creating new beta cells from existing ones.
Concurrently, they have been shown to inhibit apoptosis, or programmed cell death. This dual action shifts the balance within the pancreas from one of net beta cell loss to one of preservation and potential expansion of the functional beta cell pool. This is a fundamental shift in managing metabolic health, moving from solely addressing symptoms to actively supporting the underlying cellular machinery.
Another important peptide class to consider are the Growth Hormone Releasing Hormone (GHRH) analogs, such as Sermorelin, and Growth Hormone Releasing Peptides (GHRPs), like Ipamorelin. While their primary function is to stimulate the body’s own production of growth hormone, their downstream effects on metabolism are significant.
Improved growth hormone signaling can lead to better body composition, including an increase in lean muscle mass and a decrease in visceral fat. Since visceral fat is a major contributor to systemic inflammation and insulin resistance, reducing it can have a profound impact on metabolic health.
By improving the body’s overall insulin sensitivity, these peptides decrease the chronic demand for insulin production. This reduction in workload is intrinsically protective for the pancreas, preserving long-term beta cell function by mitigating the primary driver of their exhaustion.
| Peptide Class | Primary Metabolic Action | Direct Beta Cell Effect | Indirect Beta Cell Effect |
|---|---|---|---|
| GLP-1 Receptor Agonists | Glucose-dependent insulin secretion; Glucagon suppression | Promotes proliferation; Inhibits apoptosis | Reduces workload through improved glycemic control |
| GIP/GLP-1 Dual Agonists | Potent glucose-dependent insulin secretion; Enhanced glucagon suppression | Strongly promotes proliferation and survival pathways | Significant improvement in insulin sensitivity; Weight reduction |
| Growth Hormone Secretagogues (e.g. Sermorelin, Ipamorelin) | Stimulates natural growth hormone release | No primary direct effect | Improves systemic insulin sensitivity by reducing visceral fat and increasing lean mass |
| Amylin Analogues | Slows gastric emptying; Suppresses glucagon | Reduces post-meal glucose spikes | Decreases the acute workload on beta cells after meals |

How Do Peptides Improve Insulin Sensitivity?
Peptides like Sermorelin and Ipamorelin contribute to improved insulin sensitivity through several interconnected mechanisms, primarily driven by their ability to optimize growth hormone levels. Optimal growth hormone signaling is associated with a healthier body composition. Specifically, it promotes lipolysis, the breakdown of fat, particularly visceral adipose tissue.
This type of deep abdominal fat is metabolically active and releases inflammatory cytokines that directly interfere with insulin signaling in muscle and liver cells, causing insulin resistance. By reducing this source of inflammation, these peptides help restore the cells’ responsiveness to insulin. Additionally, the increase in lean muscle mass that can accompany this therapy creates more tissue that can effectively take up and utilize glucose from the bloodstream, further enhancing metabolic efficiency and reducing the burden on the pancreas.
- Reduced Glucotoxicity ∞ By improving glycemic control and lowering chronic high blood sugar levels, peptides protect beta cells from the damaging effects of glucose itself.
- Decreased Lipotoxicity ∞ Some peptides can help improve lipid profiles and reduce the accumulation of fat deposits within the pancreas, which can be toxic to beta cells.
- Alleviation of ER Stress ∞ By lessening the relentless demand for insulin synthesis, these therapies can ease the strain on the endoplasmic reticulum, preventing the activation of stress pathways that lead to cell death.
- Anti-inflammatory Signaling ∞ Certain peptides, particularly GLP-1 agonists, have been shown to have anti-inflammatory effects within the islets of Langerhans, creating a more favorable environment for beta cell survival and function.

Academic
A sophisticated analysis of peptide therapies on pancreatic beta cell function requires a deep exploration of the molecular pathways governing beta cell plasticity, survival, and regeneration. The conversation in endocrinology has evolved from viewing the beta cell population as static to recognizing its potential for dynamic change.
Peptide therapies, particularly those targeting the incretin system, are at the forefront of this research, providing tools to modulate these intricate cellular processes. The long-term influence of these therapies hinges on their ability to do more than just manage glycemia; it depends on their capacity to fundamentally alter the trajectory of beta cell health by promoting adaptive and regenerative responses.
The GLP-1 receptor, a G-protein coupled receptor expressed on the surface of beta cells, serves as the primary conduit for these effects. Upon binding by a GLP-1 agonist, the receptor initiates a cascade of intracellular signaling events, predominantly through the activation of adenylyl cyclase and the subsequent increase in cyclic AMP (cAMP).
This rise in cAMP activates Protein Kinase A (PKA) and Exchange Protein Activated by cAMP 2 (Epac2). These two pathways are central to the beneficial effects of GLP-1. The PKA pathway is instrumental in potentiating glucose-stimulated insulin secretion, but it also phosphorylates and activates a transcription factor called CREB (cAMP response element-binding protein), which in turn upregulates the expression of genes critical for beta cell survival and function, including the insulin gene itself and anti-apoptotic proteins like Bcl-2.
The sustained impact of incretin-based peptide therapies is rooted in their ability to activate key intracellular signaling cascades that shift the cellular environment from degenerative to regenerative.
Concurrently, the Epac2 pathway contributes to the mobilization and exocytosis of insulin granules. More importantly for long-term function, both PKA and Epac signaling converge on the activation of the MAP kinase pathway, specifically ERK1/2. Activation of the ERK pathway is strongly associated with cellular proliferation and differentiation.
This convergence of signaling provides a robust stimulus for beta cell proliferation, a phenomenon observed in numerous animal models and suggested by biomarker data in human studies. The discovery that combining GLP-1 receptor agonists with other compounds, such as DYRK1A inhibitors like harmine, can synergistically enhance human beta cell replication rates to unprecedented levels underscores the therapeutic potential of targeting these pathways.

Can Beta Cells Truly Regenerate in Adults?
The question of meaningful beta cell regeneration in adult humans is a central focus of modern diabetes research. While the adult human beta cell replication rate is exceptionally low under normal conditions, evidence suggests this is not an immutable state.
Studies involving lineage tracing in animal models have shown that under certain conditions of extreme beta cell injury, a degree of regeneration can occur through the transdifferentiation of other pancreatic cell types, most notably alpha cells, into functional beta cells. GLP-1 receptor agonists have been shown to promote this process in mice.
They appear to induce a state of cellular plasticity where alpha cells can co-express glucagon and insulin, eventually maturing into insulin-producing cells. While direct evidence in humans is challenging to obtain, the sustained improvement in C-peptide levels ∞ a marker of endogenous insulin production ∞ seen in some clinical trials with GLP-1 agonists and other novel compounds suggests that a degree of functional recovery or regeneration is occurring. These findings support the hypothesis that therapeutic intervention can unlock a latent regenerative capacity within the human pancreas.
| Peptide/Compound | Study Focus | Key Outcome Metric | Reported Result | Reference |
|---|---|---|---|---|
| GLP-1 Receptor Agonists | Chronic treatment in T2DM models | Beta cell mass, proliferation, apoptosis | Increased beta cell mass via increased proliferation and reduced apoptosis | |
| Icovamenib (covalent menin inhibitor) | Phase II trial in T2DM | C-peptide levels at 26 weeks | 55% increase in C-peptide, with over half the improvement occurring post-treatment | (Biomea Fusion Data) |
| Harmine + GLP-1 Agonist | In vitro/ex vivo human islets | Beta cell replication rate | Synergistic and dramatic increase in human beta cell proliferation rates | |
| Sermorelin | Long-term treatment in adults | Insulin Sensitivity | Significant improvement in insulin sensitivity and glucose control | (Sermorelin studies) |

The Interplay with Systemic Endocrine Health
A purely pancreatocentric view is insufficient. The health of the pancreatic beta cell is inextricably linked to the broader endocrine environment. The Hypothalamic-Pituitary-Adrenal (HPA) axis and the Hypothalamic-Pituitary-Gonadal (HPG) axis create the systemic milieu in which the beta cell must function.
Chronic stress, for instance, leads to elevated cortisol levels, which directly promotes insulin resistance and can be toxic to beta cells. Similarly, age-related declines in testosterone in men (andropause) or estrogen and progesterone in women (menopause) are associated with increased visceral adiposity and worsening insulin sensitivity.
Therefore, protocols aimed at optimizing the HPG axis, such as Testosterone Replacement Therapy (TRT) for men or carefully balanced hormonal optimization for women, can be viewed as foundational support for beta cell health.
By restoring systemic hormonal balance and reducing the inflammatory and insulin-resistant state associated with hormonal decline, these therapies create an environment where peptide-specific interventions on the beta cell can be more effective. This systems-biology perspective is essential for developing comprehensive, long-term strategies for metabolic wellness.
- Transcriptional Regulation ∞ GLP-1 agonists activate transcription factors like PDX-1, which is a master regulator of beta cell identity, function, and survival.
- Cellular Plasticity ∞ Evidence points toward the ability of these peptides to induce the conversion of pancreatic alpha cells and ductal cells into insulin-producing beta cells, a process known as neogenesis or transdifferentiation.
- Synergistic Combinations ∞ Emerging research shows that combining GLP-1 agonists with inhibitors of specific kinases, such as DYRK1A, can dramatically amplify human beta cell proliferation, opening new avenues for regenerative medicine.

References
- Thorens, Bernard, and Daniel J. Drucker. “Glucagon-like peptide-1, the L-cell, and the pancreas.” Molecular Metabolism, vol. 36, 2020, pp. 1-11.
- Wang, Peng, et al. “Harmine and GLP-1 Receptor Agonist Synergistically Promote Human Beta Cell Proliferation.” Cell Reports, vol. 30, no. 4, 2020, pp. 1095-1104.e4.
- Drucker, Daniel J. “The biology of incretin hormones.” Cell Metabolism, vol. 3, no. 3, 2006, pp. 153-65.
- Aslamy, A. et al. “Doc2b Protects β-Cells Against Inflammatory Damage and Enhances Function.” Diabetes, vol. 67, no. 7, 2018, pp. 1332-1344.
- Stewart, Andrew F. et al. “Human Beta Cell Regenerative Drug Therapy for Diabetes ∞ Past Achievements and Future Challenges.” Frontiers in Endocrinology, vol. 9, 2018, p. 744.
- Lam, Kevin, et al. “Pancreatic beta cell function persists in many with chronic T1D, but is not dramatically improved by prolonged immunosuppression and euglycemia from a beta cell allograft.” Diabetologia, vol. 54, no. 6, 2011, pp. 1423-8.
- Khorram, O. et al. “Effects of GHRH and a GHRH analog on GH and IGF-I in healthy older men and women.” The Journal of Clinical Endocrinology & Metabolism, vol. 82, no. 11, 1997, pp. 3593-9.
- Biomea Fusion, Inc. “Biomea Fusion Presents New Preclinical and Clinical Data on Icovamenib at the 85th Scientific Sessions of the American Diabetes Association (ADA).” Stock Titan, 23 June 2025.
- Shimada, M. et al. “Favorable Effects of GLP-1 Receptor Agonist against Pancreatic β-Cell Glucose Toxicity and the Development of Arteriosclerosis ∞ ‘The Earlier, the Better’ in Therapy with Incretin-Based Medicine.” International Journal of Molecular Sciences, vol. 19, no. 10, 2018, p. 3047.
- Merriam, G. R. et al. “Growth hormone-releasing hormone (GHRH) treatment in normal older men and women ∞ effects on body composition and functional status.” The Journal of Clinical Endocrinology & Metabolism, vol. 82, no. 11, 1997, pp. 3593-9.

Reflection
The information presented here offers a detailed map of the biological landscape surrounding your pancreatic health. It traces the pathways from the symptoms you may feel each day down to the intricate molecular signals that govern your cellular function. This knowledge is a powerful tool.
It transforms the abstract concept of “metabolic health” into a tangible system that you can understand and support. Consider for a moment the remarkable resilience of your body’s systems and their innate capacity for balance. The journey to sustained wellness begins with this deeper appreciation for your own biology.
How does understanding these mechanisms shift your perspective on your own health journey? Viewing your body as an interconnected system, where hormonal balance, cellular communication, and metabolic function are all part of the same conversation, opens up new possibilities. This knowledge empowers you to ask more precise questions and to become an active, informed participant in your own care.
The path forward is a personal one, built on a foundation of scientific understanding and guided by a commitment to restoring your body’s inherent vitality.

Glossary

pancreatic beta cells

your pancreatic beta cells

insulin resistance

peptide therapies

glucose levels

metabolic health

blood sugar

glucotoxicity

beta cell function

receptor agonists

glp-1 receptor agonists

beta cell health

insulin secretion

glp-1 agonists

beta cell proliferation

beta cells from

have been shown

growth hormone

ipamorelin

insulin sensitivity

sermorelin

protect beta cells from

pancreatic beta cell function

incretin system

glp-1 receptor

human beta cell replication

beta cell replication rate

beta cell regeneration

agonists have been shown

c-peptide

pancreatic beta cell




