
Fundamentals
You feel it as a subtle shift in stamina, a change in the way your body responds to exertion. It might be the recovery that takes a day longer than it used to, or a sense of vitality that seems just out of reach.
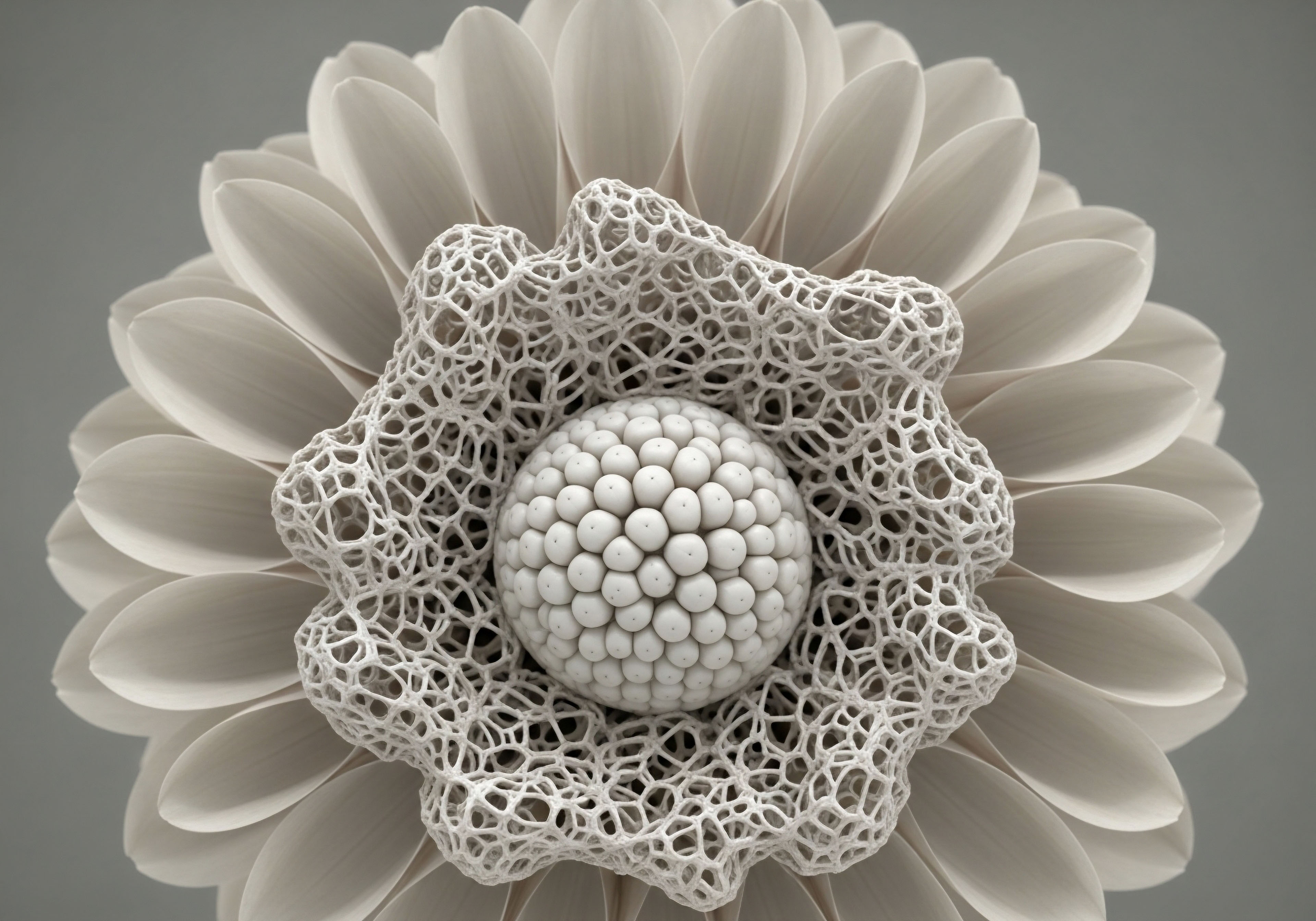
This lived experience is the starting point for a deeper inquiry into your own biology. Your cardiovascular system is an intricate communication network, a dynamic environment where messages are constantly sent and received. The quality of these messages dictates the system’s resilience, efficiency, and overall function. Hormones and peptides are the primary authors of these messages, directing cellular behavior with exquisite precision.
Understanding this biological dialogue is the first step toward reclaiming your functional capacity. The heart, blood vessels, and blood are all governed by the endocrine system’s vast signaling web. This perspective moves the conversation from one of simple mechanical failure to one of systemic imbalance.
We begin to see cardiovascular wellness as a reflection of the body’s total internal environment, where metabolic health, inflammatory status, and hormonal balance are deeply interconnected. It is within this complex interplay that peptide therapies find their purpose, acting as sophisticated tools to restore clarity and coherence to the body’s internal communication channels.

The Heart as a Dynamic System
The conventional view of the heart is often that of a tireless pump, a piece of mechanical brilliance. A more complete picture reveals it as a highly responsive endocrine organ, both sending and receiving a cascade of biochemical signals. Every heartbeat, every constriction and dilation of a blood vessel, happens in response to a precise molecular instruction.
Peptides, which are short chains of amino acids, function as a critical class of these instruction molecules. They are the body’s native language of healing, growth, and regulation.
When this signaling becomes disrupted through the natural process of aging, chronic stress, or metabolic dysfunction, the system’s efficiency declines. Inflammation may become chronic, the vascular lining may lose its flexibility, and the heart muscle itself may lose functional capacity. Peptide therapies are designed to reintroduce specific, targeted messages into this system.
They can encourage cellular repair, modulate inflammation, and support the intricate processes that maintain vascular health. This approach is about facilitating the body’s own powerful, innate mechanisms of self-regulation and healing.
Peptide therapies operate by restoring the body’s own sophisticated signaling language to improve systemic function.

What Is the True Role of Vascular Endothelium?
The inner lining of your blood vessels, the endothelium, is a vast and intelligent organ. Its health is a direct indicator of your overall cardiovascular wellness. A healthy endothelium is a flexible, smooth surface that actively manages blood flow, regulates clotting, and controls the passage of substances into and out of the bloodstream. It achieves this through the production of key signaling molecules, most notably nitric oxide.
When the endothelium becomes dysfunctional, this elegant control system breaks down. The vessels become stiff and inflamed, setting the stage for atherosclerosis and other cardiovascular complications. Many peptide therapies exert their benefits by directly supporting endothelial function.
They can reduce the oxidative stress and inflammation that damage this delicate lining, and some can promote the production of nitric oxide, restoring vascular flexibility and improving blood flow. By addressing the health of the endothelium, we are addressing a foundational element of cardiovascular vitality.


Intermediate
Moving from the conceptual to the clinical, we can examine the specific peptide protocols that offer tangible benefits to the cardiovascular system. These therapies are selected for their ability to interact with and modulate the precise biological pathways that govern vascular health and metabolic function.
The application of these peptides is grounded in a systems-biology approach, recognizing that cardiac function is inseparable from the body’s inflammatory state, glucose metabolism, and hormonal milieu. Each protocol represents a targeted intervention designed to restore a specific aspect of the body’s self-regulatory capacity.
The primary mechanisms through which these peptides operate include the reduction of systemic inflammation, the improvement of endothelial function, the optimization of metabolic markers, and the direct support of cardiac cell health. For instance, growth hormone secretagogues do more than just influence growth hormone levels; they have downstream effects on lipid metabolism and vascular compliance.
Other peptides, like BPC-157, possess powerful cytoprotective and anti-inflammatory properties that can protect vascular tissues from injury. Understanding these mechanisms allows for a logical and targeted application of peptide therapies within a personalized wellness protocol.

Growth Hormone Peptides and Vascular Health
The Growth Hormone (GH) axis plays a significant role in maintaining cardiovascular homeostasis. Peptides that stimulate the body’s own production of GH, known as secretagogues, have demonstrated benefits that extend far beyond simple muscle growth or fat loss. This class includes molecules like Ipamorelin, CJC-1295, and Tesamorelin. Their cardiovascular benefits are derived from the systemic effects of optimizing the GH/IGF-1 axis.
An optimized GH axis contributes to improved lipid profiles by promoting the breakdown of visceral fat, a key source of inflammatory cytokines. Furthermore, GH and IGF-1 have direct effects on the vascular endothelium, promoting the production of nitric oxide, which leads to vasodilation and improved blood flow. Tesamorelin, in particular, has been studied for its ability to reduce visceral adipose tissue in specific populations, a change that is strongly correlated with a reduction in cardiovascular risk factors.
Specific peptides are chosen for their capacity to modulate key pathways governing inflammation, metabolism, and cellular repair.

Key Peptides and Their Cardiovascular Mechanisms
A deeper examination reveals the distinct yet complementary roles of various therapeutic peptides. Each one offers a specific set of instructions to the body’s cellular machinery.
- Ipamorelin / CJC-1295 ∞ This combination provides a steady, biomimetic pulse of growth hormone release. Its action supports improved endothelial function, helps optimize cholesterol levels, and reduces systemic inflammation, all of which are foundational for cardiovascular health.
- Tesamorelin ∞ Clinically investigated for its potent effect on reducing visceral adipose tissue, Tesamorelin directly addresses a primary driver of metabolic syndrome and associated cardiovascular strain. By decreasing this metabolically active fat, it helps lower inflammatory markers and improve insulin sensitivity.
- BPC-157 ∞ This peptide, a sequence derived from a gastric protein, has demonstrated profound protective and healing properties. It promotes angiogenesis, the formation of new blood vessels, which is critical for repairing damaged tissue after an ischemic event. Its potent anti-inflammatory effects also protect the vascular system from ongoing damage.
- PT-141 (Bremelanotide) ∞ While primarily known for its effects on sexual function, PT-141 works through melanocortin receptors that are also involved in regulating inflammation and blood pressure. Its mechanism involves pathways that can influence vascular tone and endothelial health.
The following table provides a comparative overview of these peptides and their primary cardiovascular-related functions.
| Peptide | Primary Mechanism of Action | Key Cardiovascular Benefit |
|---|---|---|
| Ipamorelin / CJC-1295 | Stimulates natural Growth Hormone pulse | Improves endothelial function and lipid profiles |
| Tesamorelin | Reduces visceral adipose tissue | Lowers metabolic and inflammatory risk factors |
| BPC-157 | Promotes angiogenesis and reduces inflammation | Supports tissue repair and vascular protection |
| Thymosin Beta-4 (TB4) | Promotes cell migration, healing, and anti-inflammatory effects | Aids in cardiac repair and new blood vessel growth post-injury. |


Academic
An academic exploration of peptide therapeutics in cardiovascular medicine requires a shift in perspective toward the molecular interactions governing cellular function. The efficacy of these molecules is rooted in their ability to act as highly specific agonists or modulators of cellular receptors and signaling cascades that have become dysfunctional.
The central thesis is that peptides can restore homeostatic signaling, thereby ameliorating the pathophysiological processes that underpin cardiovascular disease, such as endothelial dysfunction, chronic inflammation, and adverse cardiac remodeling. This is a study of molecular communication and its restoration.
We will focus on a particularly elegant mechanism ∞ the role of certain peptides in enhancing the bioavailability of endothelial nitric oxide (NO). The health of the vascular endothelium is predicated on its capacity to produce NO, a potent vasodilator and signaling molecule that governs vascular tone, inhibits platelet aggregation, and suppresses inflammation.
A decline in NO bioavailability is a seminal event in the pathogenesis of atherosclerosis and hypertension. Growth hormone secretagogues (GHS) provide a compelling case study in how peptide therapy can directly and indirectly restore this critical function.

How Do Peptides Influence Endothelial Nitric Oxide Synthase?
The enzyme endothelial nitric oxide synthase (eNOS) is responsible for the synthesis of NO from the amino acid L-arginine. The activity of eNOS is tightly regulated by a complex interplay of factors, including shear stress from blood flow and, critically, hormonal signaling. The GH/IGF-1 axis is a powerful positive regulator of eNOS activity.
Both GH and IGF-1 have been shown to upregulate eNOS expression and activity in endothelial cells through the activation of the phosphoinositide 3-kinase (PI3K)/Akt signaling pathway.
Peptides such as Ipamorelin and CJC-1295, by stimulating endogenous GH and subsequent IGF-1 production, initiate this beneficial cascade. The activation of the Akt pathway leads to the phosphorylation of eNOS at serine residue 1177, a key step that “switches on” the enzyme, leading to a burst of NO production.
This enhanced NO bioavailability results in improved vasodilation, reduced vascular resistance, and a less inflammatory endothelial phenotype. This direct biochemical mechanism explains, in large part, the observed improvements in vascular function associated with the optimization of the GH/IGF-1 axis.
The molecular action of certain peptides can directly enhance the activity of key enzymes like eNOS, restoring critical vascular functions.

Beyond Nitric Oxide Angiogenesis and Cytoprotection
The cardiovascular benefits of peptides extend beyond the endothelium. The body-protective compound BPC-157 provides a fascinating example of a peptide with pleiotropic, cytoprotective effects. Its molecular origins are in a protein found in gastric juice, and it appears to be a natural regulator of healing and tissue maintenance. In the context of cardiovascular health, its most salient properties are its potent pro-angiogenic and anti-inflammatory effects.
BPC-157 has been observed in preclinical models to accelerate the formation of new blood vessels, a process vital for recovery from ischemic injury, such as a myocardial infarction. It appears to achieve this by upregulating the expression of Vascular Endothelial Growth Factor (VEGF) receptors. Concurrently, it exerts a powerful dampening effect on pro-inflammatory cytokines like TNF-α and IL-6, which are known drivers of atherosclerotic plaque progression. The table below outlines the molecular targets of select peptides.
| Peptide | Primary Molecular Target/Pathway | Resulting Physiological Effect |
|---|---|---|
| CJC-1295/Ipamorelin | GHRH-R / Ghrelin Receptor -> PI3K/Akt Pathway | Phosphorylation and activation of eNOS |
| BPC-157 | VEGF Receptor Upregulation / Modulation of FAK-paxillin pathway | Enhanced angiogenesis and cell survival |
| Apolipoprotein A-I Mimetics | ABCA1 Transporter | Promotion of reverse cholesterol transport. |
| SOCS1 Mimetics | JAK2 Kinase | Inhibition of inflammatory STAT signaling. |

Could Peptides Mitigate Cardiac Fibrosis?
Cardiac fibrosis, the excessive deposition of extracellular matrix in the heart muscle, is a final common pathway in many forms of heart disease, leading to stiffness and diastolic dysfunction. Growth hormone has demonstrated anti-fibrotic properties in cardiac tissue.
It appears to work by counteracting the pro-fibrotic signaling of transforming growth factor-beta (TGF-β1), a key cytokine involved in the fibrotic process. By restoring a more youthful GH/IGF-1 signaling environment, GHS peptides may help mitigate the progression of cardiac fibrosis, preserving the heart’s compliance and function over time. This represents a proactive strategy aimed at preventing the structural changes that lead to heart failure.
- Signaling Restoration ∞ Peptides like Sermorelin or CJC-1295 restore GH signaling patterns.
- TGF-β1 Antagonism ∞ Optimized IGF-1 levels interfere with the TGF-β1 pathway, reducing the activation of cardiac fibroblasts.
- Matrix Modulation ∞ This process leads to a more balanced deposition and degradation of collagen, preserving the heart’s structural integrity.

References
- Rysz, Jakub, et al. “The Role of BPC 157 in the Treatment of Cardiovascular Diseases.” International Journal of Molecular Sciences, vol. 24, no. 13, 2023, p. 11234.
- De Spiegeleer, Bart, et al. “The Future of Peptide Drug Development.” Therapeutic Innovation & Regulatory Science, vol. 52, no. 1, 2018, pp. 11-13.
- King, M. K. & Kaplan, J. D. “Use of Tesamorelin in a Patient with HIV and Nonalcoholic Steatohepatitis.” The Annals of Pharmacotherapy, vol. 47, no. 10, 2013, pp. e42.
- Vassalle, C. “Peptides in the diagnosis, prognosis and therapy of cardiovascular diseases.” Current Medicinal Chemistry, vol. 15, no. 8, 2008, pp. 787-798.
- Pell, V. R. et al. “Growth hormone axis and cardiac function ∞ experimental and clinical evidence.” Journal of Molecular Endocrinology, vol. 62, no. 3, 2019, pp. R151-R160.
- Gentilini, D. et al. “Growth hormone and heart failure ∞ an update on a debated topic.” Growth Hormone & IGF Research, vol. 25, no. 4, 2015, pp. 165-171.
- Catapano, A. L. et al. “Apolipoprotein A-I mimetic peptides ∞ a new approach for the treatment of atherosclerosis.” Current Opinion in Investigational Drugs, vol. 5, no. 6, 2004, pp. 636-641.
- Madonna, R. et al. “Suppressor of cytokine signalling 1 mimetic peptide limits vascular inflammation and atherosclerosis in mice.” Cardiovascular Research, vol. 97, no. 1, 2013, pp. 167-176.

Reflection
The information presented here serves as a map of the intricate biological landscape that governs your cardiovascular vitality. It illuminates the pathways and communication networks that determine how well your system functions. This knowledge is the foundational tool for building a truly personalized health strategy.
Your own journey begins with the questions that arise from this new understanding. How does my own metabolic health influence my vascular system? What signals might my body be sending, and how can I learn to interpret them with greater clarity? This inquiry, guided by clinical expertise, is the path toward reclaiming and sustaining your highest level of function.



