

Fundamentals
You sense a subtle yet persistent dissonance within your body. Despite disciplined efforts with nutrition and exercise, a feeling of fatigue lingers, the numbers on the scale remain static, and a general sense of vitality feels just out of reach. This experience points toward a deeper conversation happening within your endocrine system, a dialogue between your thyroid hormones and your estrogen receptors. The question of how to support this internal communication network is central to reclaiming your body’s intended function.
The body’s hormonal landscape operates as an intricate, interconnected system. Your thyroid gland, located at the base of your neck, produces hormones that set the metabolic rate for every cell in your body. Concurrently, estrogen interacts with its own specific receptors to regulate a vast array of processes, from reproductive health to cognitive function and bone density. These two systems are in constant communication, influencing each other’s effectiveness in profound ways.
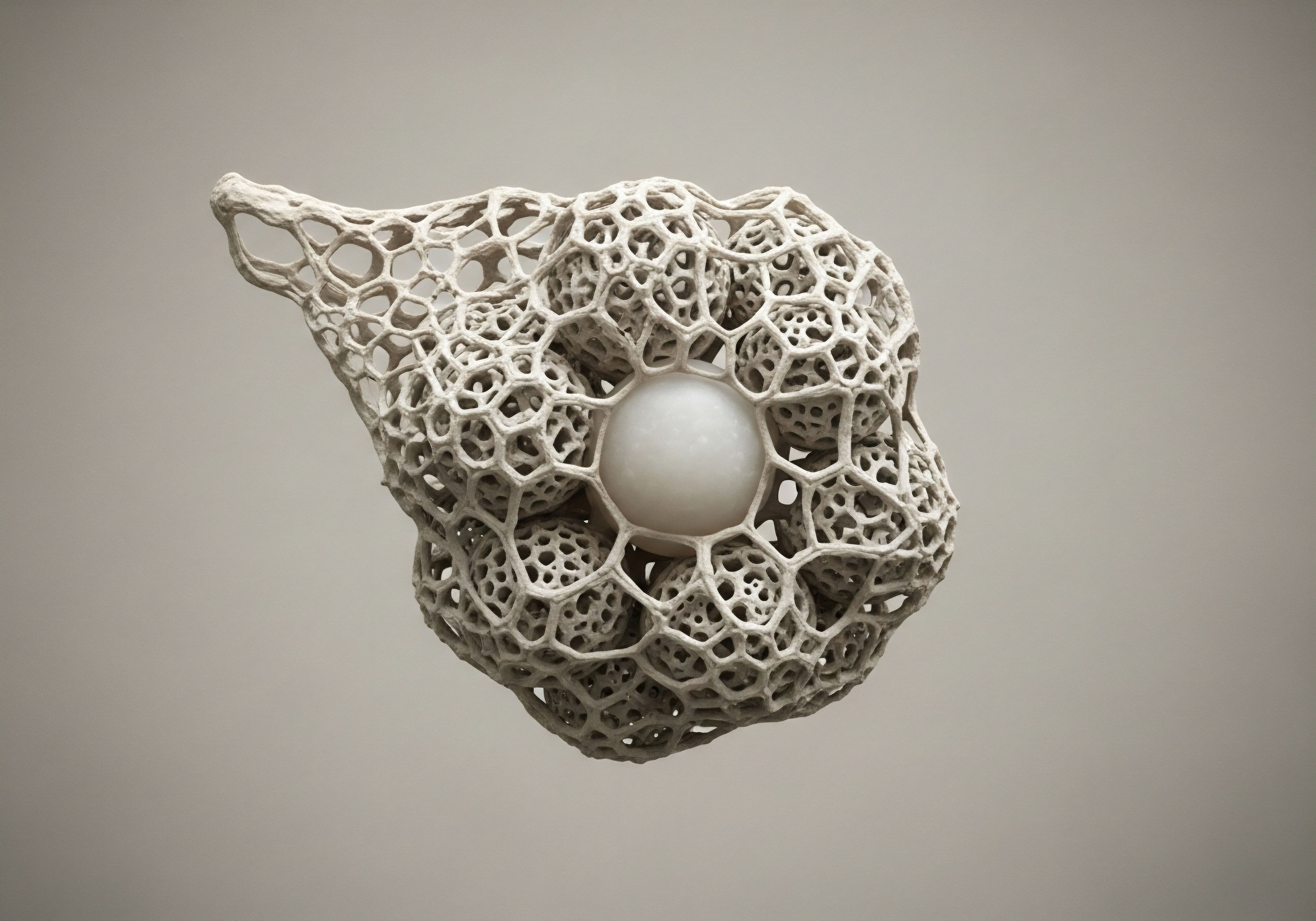
The sensitivity of a cell’s receptors determines its ability to respond to hormonal signals, much like a key fitting a lock.
Understanding this relationship begins with the concept of receptor sensitivity. A hormone, such as estrogen or the active thyroid hormone T3, is a messenger molecule. Its message can only be received if it binds successfully to a receptor on the surface of or inside a target cell.
When receptors are sensitive and abundant, a small amount of hormone can produce a significant effect. When sensitivity is low, the hormonal message is effectively unheard, even if hormone levels in the bloodstream appear normal. Lifestyle interventions are the tools we use to modulate the sensitivity of these receptors, ensuring the messages sent by your hormones are properly received.

The Estrogen and Thyroid Connection
Estrogen has a direct effect on thyroid function. It can increase the body’s production of thyroxine-binding globulin (TBG), a protein that carries thyroid hormones through the bloodstream. When thyroid hormones are bound to TBG, they are inactive. An elevation in TBG can therefore reduce the amount of free, usable thyroid hormone available to your cells.
This dynamic illustrates why a comprehensive approach to wellness must consider both systems simultaneously. Addressing thyroid health without considering the estrogen environment, or vice versa, provides an incomplete picture of the body’s true functional state.

What Influences Receptor Health?
The health and responsiveness of your cellular receptors are not static. They are dynamically influenced by a host of daily inputs. Chronic stress, for instance, elevates cortisol, a hormone that can suppress the conversion of inactive thyroid hormone (T4) to its active form (T3) and interfere with estrogen signaling.
Similarly, exposure to endocrine-disrupting chemicals (EDCs) found in many personal care products and plastics can bind to hormone receptors, blocking the action of your body’s natural hormones. These factors highlight a critical principle of metabolic health ∞ our daily choices directly impact our body’s ability to hear and respond to its own internal cues.


Intermediate
To meaningfully support both estrogen receptor sensitivity and thyroid function, we must move beyond general wellness advice and into specific, targeted lifestyle protocols. These interventions are designed to directly influence the biological pathways that govern hormonal communication. The objective is to create an internal environment that optimizes receptor density, enhances binding affinity, and ensures the efficient downstream signaling that translates hormonal messages into physiological action.
This process involves a multi-pronged strategy that addresses nutritional biochemistry, physical stressors, and the management of systemic inflammation. Each element provides a distinct set of inputs that can either enhance or inhibit the delicate balance of the endocrine system. By consciously managing these inputs, we can encourage our bodies to restore a more responsive and efficient hormonal state.

Nutritional Protocols for Hormonal Recalibration
Nutrition provides the raw materials for hormone production and the cofactors necessary for their metabolic pathways. A targeted nutritional strategy can profoundly influence both estrogen metabolism and thyroid efficiency. The focus is on incorporating specific food groups and micronutrients that support these systems while minimizing exposure to compounds that disrupt them.
Cruciferous vegetables, such as broccoli, cauliflower, and Brussels sprouts, contain a compound called indole-3-carbinol, which is converted to diindolylmethane (DIM) in the gut. DIM helps promote a healthier metabolism of estrogen, favoring the production of less potent estrogen metabolites.
Phytoestrogens, found in foods like flax seeds and organic soy, are plant-based compounds that can bind to estrogen receptors. Their mild estrogenic effect can help modulate the body’s response in states of either high or low estrogen, acting as balancing agents within the system.
| Nutrient/Compound | Primary Source | Mechanism of Action |
|---|---|---|
| Iodine | Seaweed, seafood, iodized salt | A fundamental building block of thyroid hormones (T4 and T3). |
| Selenium | Brazil nuts, fish, poultry | Essential cofactor for the deiodinase enzymes that convert inactive T4 to active T3. |
| Zinc | Oysters, beef, pumpkin seeds | Plays a role in the synthesis of thyroid-releasing hormone (TRH) in the hypothalamus. |
| DIM (from Indole-3-Carbinol) | Broccoli, kale, cabbage | Supports the healthy metabolism and detoxification of estrogen in the liver. |
| Fiber | Vegetables, fruits, legumes | Binds to excess estrogen in the digestive tract, facilitating its excretion from the body. |

How Does Exercise Modulate Receptor Sensitivity?
Physical activity is a powerful modulator of hormonal health, with different forms of exercise exerting distinct effects. The goal is to create a balanced regimen that improves insulin sensitivity, manages cortisol, and directly impacts hormone receptor expression.
High-intensity interval training (HIIT) has been shown to be particularly effective at improving insulin sensitivity. Since insulin resistance can contribute to hormonal imbalances like Polycystic Ovary Syndrome (PCOS), which is characterized by elevated estrogen, managing blood sugar is a critical component of endocrine health.
Resistance training, on the other hand, helps build lean muscle mass. Muscle tissue is more metabolically active than fat tissue and can improve the body’s overall hormonal environment. Furthermore, reducing excess adipose tissue is important because fat cells can produce and store estrogen, contributing to a state of estrogen dominance.
Strategic exercise acts as a signaling event, telling cells to become more receptive to hormonal messages.

The Role of Stress and Circadian Rhythm
The body’s stress response system, governed by the hypothalamic-pituitary-adrenal (HPA) axis, is deeply intertwined with both thyroid and reproductive hormones. Chronic activation of this system, leading to elevated cortisol, creates a cascade of disruptive effects. Cortisol can inhibit the conversion of T4 to T3, effectively slowing down metabolism. It can also alter the sensitivity of estrogen receptors, contributing to symptoms of hormonal imbalance.
Aligning with the body’s natural circadian rhythm is a foundational practice for HPA axis regulation. This involves consistent sleep and wake times, exposure to natural light in the morning, and minimizing blue light exposure in the evening. These practices help anchor the body’s internal clock, leading to more regulated cortisol patterns and, consequently, a more stable and responsive endocrine system.


Academic
A deeper exploration into the molecular cross-talk between thyroid hormone signaling and estrogen receptor function reveals a complex web of interactions mediated by nuclear receptors, genomic and non-genomic pathways, and, critically, the gut microbiome.
The functional status of the gastrointestinal system, particularly the composition and metabolic activity of its resident microbes, represents a significant and often underappreciated control point in systemic endocrine regulation. This section will examine the role of the “estrobolome” and the gut-thyroid axis as a central mechanism through which lifestyle interventions can exert their effects.

The Estrobolome and Estrogen Recirculation
The estrobolome is defined as the aggregate of enteric bacterial genes whose products are capable of metabolizing estrogens. After estrogens are produced in the gonads and other tissues, they travel to the liver for conjugation, a process that marks them for excretion. These conjugated estrogens are then transported into the bile and subsequently into the intestinal lumen.
Here, certain gut bacteria produce an enzyme called β-glucuronidase. This enzyme deconjugates the estrogens, allowing them to be reabsorbed back into circulation through the enterohepatic pathway.
A state of gut dysbiosis, characterized by an imbalance in microbial populations, can lead to either an under-activity or over-activity of β-glucuronidase. Elevated activity can result in an increased reabsorption of estrogens, contributing to a state of estrogen dominance.
This has direct implications for thyroid health, as higher circulating levels of estrogen increase thyroxine-binding globulin (TBG), thereby reducing the bioavailability of free thyroid hormones. Lifestyle interventions, particularly those focused on diet, directly shape the composition of the estrobolome.
- Prebiotic Fibers ∞ Sourced from foods like Jerusalem artichokes, garlic, and onions, these fibers nourish beneficial bacterial species, such as Lactobacilli and Bifidobacteria, which tend to promote a balanced β-glucuronidase activity.
- Polyphenols ∞ Compounds found in berries, green tea, and dark chocolate act as antioxidants and can modulate the gut microbial environment, favoring the growth of beneficial bacteria and supporting a healthy gut lining.
- Probiotic-Rich Foods ∞ Fermented foods like kimchi, sauerkraut, and kefir introduce beneficial microbes into the gut, helping to restore a more balanced and diverse microbial community.

What Is the Gut Thyroid Axis?
The connection between the gut and the thyroid extends beyond estrogen metabolism. The gut microbiome plays a crucial role in the conversion of inactive T4 to active T3. Approximately 20% of this vital conversion occurs in the gastrointestinal tract, dependent on the presence of the intestinal sulfatase enzyme, which is produced by healthy gut bacteria. Gut dysbiosis can impair this conversion process, leading to a functional hypothyroidism even when the thyroid gland itself is producing adequate T4.
The gut microbiome functions as a central endocrine organ, actively participating in the regulation of systemic hormonal balance.
Furthermore, intestinal permeability, or “leaky gut,” is a primary trigger for autoimmune conditions, including Hashimoto’s thyroiditis, the most common cause of hypothyroidism in the developed world. When the gut lining is compromised, undigested food particles and bacterial components can enter the bloodstream, triggering an immune response.
Due to a phenomenon called molecular mimicry, the antibodies produced to target these foreign invaders can sometimes cross-react with proteins in the thyroid gland, leading to autoimmune destruction of thyroid tissue. Dietary interventions that remove inflammatory triggers and support the integrity of the gut lining are therefore paramount in managing autoimmune thyroid disease.
| Factor | Gut-Mediated Mechanism | Impact on Estrogen | Impact on Thyroid |
|---|---|---|---|
| Gut Dysbiosis | Altered β-glucuronidase activity. | Increased estrogen recirculation, leading to potential estrogen dominance. | Increased TBG, reducing free thyroid hormone availability. |
| Impaired T4-T3 Conversion | Reduced intestinal sulfatase from microbial imbalance. | Indirectly affects metabolic rate, which influences hormone clearance. | Reduced availability of active T3, leading to hypothyroid symptoms. |
| Intestinal Permeability | Passage of lipopolysaccharides (LPS) into circulation. | Systemic inflammation can disrupt HPG axis signaling. | Potential trigger for autoimmune thyroiditis (Hashimoto’s) via molecular mimicry. |
| Micronutrient Absorption | Healthy gut villi are required for absorption. | Absorption of B vitamins needed for estrogen detoxification. | Absorption of selenium, zinc, and iron needed for hormone synthesis and conversion. |
In conclusion, the gut serves as a critical interface between our external environment (diet and lifestyle) and our internal endocrine milieu. Supporting estrogen receptor sensitivity and thyroid function requires a clinical focus on restoring gut health. This systems-biology perspective demonstrates that targeted lifestyle interventions are not merely supportive but are in fact potent modulators of fundamental hormonal physiology.

References
- Patil, Neha, et al. “The Crosstalk between Gut Microbiota and Thyroid Gland ∞ A Narrative Review.” Journal of the Endocrine Society, vol. 7, no. 10, 2023, bvad113.
- Kresser, Chris. “Thyroid-Gut-Axis ∞ How to Heal Your Gut for Better Thyroid Function.” Kresser Institute, 2021.
- Pellatt, Amy J. et al. “Thyroid Hormone and Estrogen Receptor Interaction in Breast Cancer.” Journal of the Endocrine Society, vol. 3, no. 8, 2019, pp. 1541-1554.
- Bredella, Miriam A. “The Role of Exercise in the Treatment of Polycystic Ovary Syndrome.” Current Opinion in Endocrinology, Diabetes and Obesity, vol. 24, no. 6, 2017, pp. 385-390.
- Gierach, Gretchen L. et al. “Physical Activity, Recreational and Occupational, and Postmenopausal Breast Cancer Risk.” Journal of the National Cancer Institute, vol. 102, no. 9, 2010, pp. 631-640.
- Allgeier, Christine, and Mary R. Andriollo. “Estrogen and Thyroid Hormone Receptor Interactions ∞ Physiological and Clinical Implications.” Endocrine Reviews, vol. 18, no. 4, 1997, pp. 495-519.
- Baker, Kristina R. and R. Michael Tuttle. “Thyroid Disease and the Gut Microbiome.” The Journal of Clinical Endocrinology & Metabolism, vol. 103, no. 11, 2018, pp. 4026-4034.

Reflection
The information presented here provides a map of the intricate biological terrain connecting your lifestyle choices to your hormonal vitality. It illuminates the pathways through which nutrition, movement, and stress modulation become potent tools for physiological change. This knowledge shifts the perspective from one of managing symptoms to one of cultivating a responsive internal environment.
Consider your own daily rhythms and patterns. Where are the opportunities to send a clearer, more supportive signal to your body? The journey to reclaiming your vitality begins with understanding this profound dialogue between your actions and your cells, recognizing that you are an active participant in the conversation.

Glossary

endocrine system

thyroid hormones
thyroid gland

receptor sensitivity

thyroid hormone

lifestyle interventions

thyroid function

estrogen receptor sensitivity

indole-3-carbinol

hormone receptor

insulin resistance

hpa axis regulation

estrogen receptor

nuclear receptors

gut-thyroid axis

estrobolome

the estrobolome

gut microbiome




