Fundamentals
The experience of noticing a change in your cognitive sharpness, a subtle shift in memory recall, or a general feeling of mental fog often coincides with significant periods of hormonal transition. This is a deeply personal and frequently unsettling experience.
It is a direct communication from your body’s intricate internal systems, signaling a change in the biochemical environment that has long supported your brain’s structure and function. The question of whether lifestyle choices can influence these changes is a profound one, and the answer begins with understanding the biological dialogue between your hormones and your brain.
Your brain is a profoundly active and adaptable organ, and its physical integrity is intimately linked to the chemical messengers that circulate throughout your body. Hormones such as estradiol in women and testosterone in men are powerful stewards of neurological health, acting directly on brain cells to support their vitality, their connections, and their ability to communicate effectively.
When the production of these key hormones begins to decline, as it does during perimenopause, menopause, and andropause, the brain undergoes tangible structural shifts. Areas critical for memory and higher-order thinking, particularly the hippocampus and regions of the cerebral cortex, can experience a reduction in volume. This is a physiological reality.
The communication pathways, or synapses, that allow for rapid thought and memory formation can become less efficient. The brain’s ability to draw upon energy resources can also be altered. These are not failures of intellect or character; they are the predictable biological consequences of a changing internal hormonal landscape. Recognizing this connection is the first step in moving from a position of concern to one of proactive engagement with your own health.

The Architecture of Brain Health
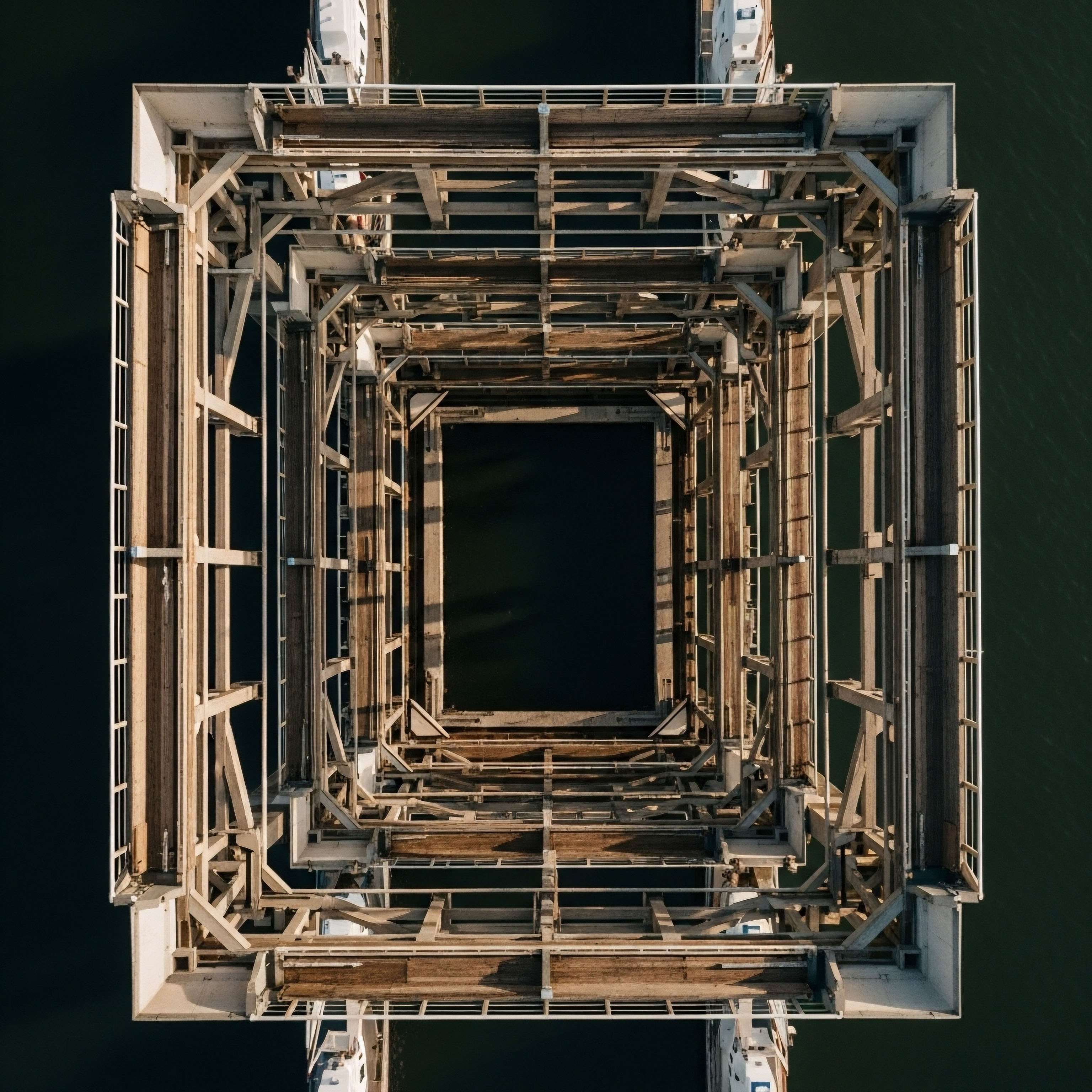
Thinking of your brain as a complex and dynamic city provides a useful framework. The neurons are the buildings and residences, and the synapses are the roads and communication lines connecting everything. Hormones like estradiol and testosterone function as the city’s master architects and maintenance crews.
They oversee the construction of new connections, ensure the roads are clear for traffic, and manage the city’s power supply. When the levels of these hormones decrease, it is as if the maintenance budget has been reduced. Some roads may become less reliable, and the power grid might fluctuate. The structural integrity of the city itself is challenged.
This is where lifestyle interventions become so powerful. They do not simply patch over the issues; they provide the raw materials and the stimulus for the city to begin reinforcing its own infrastructure. Diet and exercise act as independent, potent biological signals that can directly counter some of the structural changes initiated by hormonal decline.
They provide an alternative set of instructions to the brain, encouraging it to maintain its plasticity, preserve its volume, and optimize its function, even as the primary hormonal support system is changing. This is a process of building resilience from within, using tangible, daily actions as the tools.
Lifestyle interventions provide the biological resources and stimuli for the brain to fortify its own structure against hormonal shifts.

Diet as a Neuro-Supportive Tool
The food you consume is far more than simple fuel; it is a source of complex information that your body and brain use to regulate function. A diet centered on whole, unprocessed foods provides the essential building blocks for neurotransmitters, the chemicals that facilitate communication between brain cells.
It also supplies the vitamins and minerals that act as cofactors in countless enzymatic reactions essential for brain energy metabolism. Adopting a dietary pattern like the Mediterranean diet, which is rich in colorful vegetables, fruits, healthy fats from olive oil and nuts, and lean proteins, provides a constant stream of antioxidants and anti-inflammatory compounds.
These molecules actively protect brain cells from the oxidative stress and low-grade inflammation that are known to accelerate the aging process and are often exacerbated by hormonal changes. By consciously choosing foods that support neurological health, you are directly investing in the physical material of your brain.

Exercise as a Catalyst for Brain Remodeling
Physical activity is one of the most effective methods for initiating positive structural changes in the brain. When you engage in exercise, particularly aerobic activities that elevate your heart rate, you increase blood flow to the brain. This enhanced circulation delivers a greater supply of oxygen and essential nutrients, which supports the health of all brain tissue.
More than that, exercise acts as a direct molecular signal to stimulate the production of growth factors. These proteins, most notably Brain-Derived Neurotrophic Factor (BDNF), function like a potent fertilizer for neurons. They encourage the growth of new brain cells, a process called neurogenesis, especially within the hippocampus.
They also strengthen the connections between existing neurons, enhancing the brain’s capacity for learning and adaptation, a quality known as synaptic plasticity. This process of physical reinforcement through movement provides a powerful counterbalance to the structural declines associated with hormonal shifts.


Intermediate
To appreciate how profoundly lifestyle choices can mitigate the brain’s structural response to hormonal decline, we must examine the specific biological mechanisms at play. The process is an elegant interplay of molecular signaling, cellular regeneration, and systemic regulation. Exercise and diet are not passive influences; they actively initiate cascades of events that preserve neuronal architecture and enhance cognitive resilience.
The conversation moves from the general concept of “brain health” to a more precise understanding of how targeted inputs can generate specific, measurable outputs in the brain’s physical structure and functional capacity.
The decline in hormones like estrogen and testosterone creates a permissive environment for atrophy and inflammation within the central nervous system. Lifestyle interventions serve as a powerful counter-regulatory force. They work by activating alternative pathways that promote growth, repair, and metabolic efficiency. This is a form of biological recalibration, where you are using external stimuli to tune your internal environment, compensating for the diminished hormonal signals and fostering a new state of equilibrium that is conducive to neurological vitality.

The Molecular Language of Exercise
When the body engages in sustained physical activity, it communicates with the brain through a sophisticated chemical language. This dialogue is mediated by a host of molecules that cross the blood-brain barrier and initiate profound changes at the cellular level. Understanding this language reveals how exercise directly builds a more robust and adaptable brain.

The Central Role of Neurotrophic Factors
Neurotrophic factors are a class of proteins that support the growth, survival, and differentiation of developing and mature neurons. They are the primary agents through which exercise exerts its neuroprotective and regenerative effects. Three of the most critical players in this process are:
- Brain-Derived Neurotrophic Factor (BDNF) ∞ Often described as “Miracle-Gro for the brain,” BDNF is a cornerstone of neuroplasticity. Exercise, particularly aerobic exercise, is a potent stimulator of BDNF production. Once released, BDNF binds to its receptor, TrkB, on neurons, triggering a signaling cascade that enhances synaptic transmission, promotes the growth of new dendrites (the branching extensions of a neuron that receive signals from other neurons), and is essential for Long-Term Potentiation (LTP), the cellular mechanism underlying learning and memory. Increased BDNF levels directly combat the synaptic pruning and loss of connectivity seen with hormonal decline.
- Vascular Endothelial Growth Factor (VEGF) ∞ This protein is critical for angiogenesis, the formation of new blood vessels. Exercise upregulates VEGF, leading to a denser capillary network within the brain. This enhanced vasculature improves the delivery of oxygen and glucose, the brain’s primary fuels, and facilitates the removal of metabolic waste products. This process ensures the brain’s metabolic needs are met, which is particularly important as hormonal changes can sometimes impair cerebral glucose metabolism.
- Insulin-like Growth Factor 1 (IGF-1) ∞ Produced by the liver in response to exercise and growth hormone signaling, IGF-1 travels to the brain where it plays a multifaceted role. It stimulates the proliferation of neural stem cells, contributing to adult hippocampal neurogenesis. It also works in concert with BDNF to promote synaptic plasticity and neuronal survival. Furthermore, IGF-1 is crucial for regulating brain insulin sensitivity, helping to maintain proper energy balance within neurons.
| Exercise Type | Primary Neurological Mechanism | Key Structural and Functional Outcomes |
|---|---|---|
| Aerobic Exercise (e.g. Running, Swimming, Cycling) |
Potent upregulation of Brain-Derived Neurotrophic Factor (BDNF) and Vascular Endothelial Growth Factor (VEGF). Enhanced cerebral blood flow. |
Promotes adult hippocampal neurogenesis, increases synaptic density, improves memory and executive function, enhances vascular health of the brain. |
| Strength Training (e.g. Weightlifting, Bodyweight exercises) |
Increases circulating levels of Insulin-like Growth Factor 1 (IGF-1). Improves systemic insulin sensitivity, which is reflected in the brain. |
Supports neuronal growth and survival, protects against age-related muscle loss (sarcopenia) which is linked to cognitive decline, improves white matter integrity. |

How Does Diet Reshape the Brain’s Environment?
A strategic dietary approach, such as the Mediterranean diet, works by fundamentally altering the biochemical environment in which the brain operates. It shifts the balance away from inflammation and oxidative stress towards a state of protection and repair. This is accomplished through several interconnected pathways that directly address the vulnerabilities created by hormonal decline.
A nutrient-dense diet systematically reduces inflammation and oxidative stress, creating a protective biochemical environment for the brain.

Taming Neuroinflammation and Oxidative Stress
Hormonal decline, particularly the loss of estrogen, is associated with a rise in pro-inflammatory markers in the brain. The Mediterranean diet is rich in compounds that directly counter this trend.
- Polyphenols ∞ Found in berries, dark chocolate, green tea, and olive oil, these plant-based compounds are powerful antioxidants and anti-inflammatory agents. They can cross the blood-brain barrier and directly inhibit inflammatory signaling pathways within the brain, such as the NF-kB pathway. They also activate the body’s own antioxidant defense systems.
- Omega-3 Fatty Acids ∞ Abundant in fatty fish like salmon and walnuts, these essential fats are incorporated into the membranes of neurons, influencing their fluidity and function. Their metabolic byproducts, known as resolvins and protectins, are potent anti-inflammatory molecules that actively help to resolve inflammation, protecting neurons from collateral damage.

The Gut-Brain Axis a New Frontier
The connection between the gut and the brain is a critical component of neurological health. The gut microbiome, the community of trillions of bacteria residing in your digestive tract, communicates with the brain via neural, endocrine, and immune pathways. A diet high in fiber from vegetables, fruits, and whole grains nourishes a diverse and healthy microbiome.
These beneficial microbes produce short-chain fatty acids (SCFAs), such as butyrate, which can travel to the brain and exert neuroprotective effects, including supporting BDNF production and reducing inflammation. Conversely, a diet high in processed foods can lead to gut dysbiosis, which promotes systemic inflammation that can negatively impact the brain. Supporting gut health is a direct way to support brain health.


Academic
A sophisticated analysis of how lifestyle interventions can counteract the structural brain changes of hormonal decline requires a systems-biology perspective. The central thesis is that the withdrawal of gonadal steroids, particularly estradiol, precipitates a state of chronic, low-grade neuroinflammation, which acts as a primary driver of neuronal atrophy and synaptic dysfunction.
This process is mediated by the brain’s resident immune cells, the microglia. Lifestyle interventions, specifically targeted dietary patterns and consistent physical exercise, function as powerful immunomodulatory agents, capable of shifting microglial phenotype and disrupting the inflammatory cascade at a molecular level.

The Centrality of Microglial Activation in Hormonal Senescence
Microglia are the primary immune effectors of the central nervous system (CNS). In a healthy, homeostatic state, they exist in a resting or “surveying” state, extending and retracting their processes to monitor the parenchymal environment. They can be polarized into different functional phenotypes.
The M2 phenotype is associated with anti-inflammatory and neurotrophic functions, promoting debris clearance, tissue repair, and the release of growth factors like IGF-1. The M1 phenotype, conversely, is pro-inflammatory, characterized by the release of cytotoxic molecules including reactive oxygen species (ROS), nitric oxide (NO), and pro-inflammatory cytokines like Tumor Necrosis Factor-alpha (TNF-α) and Interleukin-1 beta (IL-1β).
Estradiol is a potent modulator of microglial function. It promotes the M2 phenotype and suppresses the M1 phenotype, thereby maintaining an anti-inflammatory tone within the CNS. The profound drop in estradiol levels during the menopausal transition removes this crucial braking mechanism.
In the absence of sufficient estrogenic signaling, microglia become more prone to M1 polarization in response to stimuli like cellular debris or misfolded proteins. This creates a self-perpetuating cycle of neuroinflammation. The cytokines released by M1 microglia can directly impair synaptic plasticity, inhibit neurogenesis, and induce neuronal apoptosis, contributing directly to the hippocampal and cortical volume loss observed in postmenopausal women.
This shift establishes a brain environment that is not only less supportive of cognitive function but also more vulnerable to the development of age-related neurodegenerative diseases.

How Does Exercise Directly Modulate Neuroinflammation?
Physical exercise introduces a suite of systemic and local signals that actively counter the pro-inflammatory state induced by hormonal decline. Its mechanisms are multifaceted, involving both direct effects on the brain and indirect effects mediated by peripheral tissues.
- Myokine Signaling ∞ Skeletal muscle, when contracting during exercise, functions as an endocrine organ, releasing signaling proteins called myokines. One such myokine, irisin, has been shown to cross the blood-brain barrier and reduce neuroinflammation. Another, IL-6 released from muscle, has paradoxical effects; while systemically pro-inflammatory in chronic disease states, its transient release during exercise has anti-inflammatory consequences, promoting the production of anti-inflammatory cytokines like IL-10.
- Modulation of Microglial Phenotype ∞ Exercise has been demonstrated in preclinical models to directly influence microglial polarization. It promotes a shift from the M1 to the M2 phenotype, thereby increasing the production of anti-inflammatory cytokines and neurotrophic factors within the brain microenvironment. This shift helps to restore homeostasis and creates conditions favorable for synaptic repair and growth.
- Regulation of the Tryptophan-Kynurenine Pathway ∞ Chronic inflammation can shunt the metabolism of the amino acid tryptophan away from serotonin production and towards the kynurenine pathway. A downstream metabolite of this pathway, quinolinic acid, is a potent neurotoxin. Exercise induces the expression of kynurenine aminotransferase in skeletal muscle, which converts kynurenine into kynurenic acid, a compound that cannot cross the blood-brain barrier. This peripheral shunting effectively reduces the brain’s exposure to neurotoxic kynurenine metabolites.
Exercise initiates a cascade of anti-inflammatory signals that can shift microglial cells from a destructive to a reparative state.

The Molecular Impact of Diet on Inflammatory Pathways
Dietary components can exert precise pharmacological-like effects on the molecular machinery of inflammation within the brain. The anti-inflammatory properties of a Mediterranean-style diet are not merely circumstantial; they are the result of specific molecules interacting with key signaling nodes.
| Dietary Component | Molecular Target/Pathway | Neuroprotective Effect |
|---|---|---|
| Omega-3 Fatty Acids (EPA/DHA) |
Inhibition of cyclooxygenase (COX) and lipoxygenase (LOX) enzymes. Precursors to specialized pro-resolving mediators (SPMs) like resolvins and protectins. |
Reduces production of pro-inflammatory prostaglandins and leukotrienes. Actively resolves inflammation and promotes tissue healing, shifting microglia to an M2 phenotype. |
| Polyphenols (e.g. Curcumin, Resveratrol) |
Inhibition of the transcription factor Nuclear Factor-kappa B (NF-κB). Activation of the Nrf2 antioxidant response element. |
Downregulates the genetic expression of numerous pro-inflammatory cytokines (TNF-α, IL-1β, IL-6). Upregulates the expression of endogenous antioxidant enzymes. |
| Dietary Fiber |
Gut microbiota metabolism into Short-Chain Fatty Acids (SCFAs), particularly butyrate. |
Butyrate functions as a histone deacetylase (HDAC) inhibitor in the brain, leading to epigenetic modifications that increase BDNF expression. It also strengthens the gut-blood and blood-brain barriers, reducing inflammatory influx. |
The convergence of these dietary mechanisms provides a powerful, multi-pronged strategy to lower the baseline neuroinflammatory state. By inhibiting pro-inflammatory signaling, providing the building blocks for anti-inflammatory molecules, and supporting a healthy gut-brain axis, these dietary patterns directly counteract the inflammatory permissiveness created by the decline of gonadal hormones.
This comprehensive approach demonstrates that strategic lifestyle interventions are not simply supportive measures; they are potent biological response modifiers capable of mitigating the fundamental drivers of structural brain change associated with hormonal aging.

References
- Villa, Roberta F. et al. “The effects of hormones and physical exercise on hippocampal structural plasticity.” Neuroscience & Biobehavioral Reviews, vol. 69, 2016, pp. 56-81.
- Gu, Yian, et al. “Mediterranean diet and brain structure in a multiethnic elderly cohort.” Neurology, vol. 85, no. 20, 2015, pp. 1744-51.
- Vegeto, Elisabetta, et al. “Estrogen anti-inflammatory activity in brain ∞ a therapeutic opportunity for menopause and neurodegenerative diseases.” Frontiers in Neuroendocrinology, vol. 29, no. 4, 2008, pp. 507-19.
- Erickson, Kirk I. et al. “Exercise training increases size of hippocampus and improves memory.” Proceedings of the National Academy of Sciences, vol. 108, no. 7, 2011, pp. 3017-22.
- Voss, Michelle W. et al. “Plasticity of brain networks in a randomized intervention trial of exercise in older adults.” Frontiers in Aging Neuroscience, vol. 2, 2010, p. 32.
- Lista, Isabella, and Harald Hampel. “The role of exercise in the prevention of Alzheimer’s disease.” British Medical Journal, vol. 358, 2017.
- Mosconi, Lisa, et al. “Perimenopause and emergence of an Alzheimer’s bioenergetic phenotype in brain and periphery.” PLoS ONE, vol. 16, no. 10, 2021, e0255653.
- Brinton, Roberta D. “The healthy cell bias of estrogen action ∞ mitochondrial bioenergetics and neurological protection.” Trends in Endocrinology & Metabolism, vol. 19, no. 3, 2008, pp. 79-87.
- Mishra, S. P. and R. D. Brinton. “Dynamic neuroimmune profile during mid-life aging in the female brain and implications for Alzheimer risk.” Neurobiology of Aging, vol. 96, 2020, pp. 13-26.
- Spencer, S. J. et al. “The gut microbiome ∞ a key regulator of energy metabolism and the peripheral and central stress systems.” Molecular Psychiatry, vol. 22, no. 1, 2017, pp. 24-33.

Reflection

Translating Knowledge into Personal Practice
The information presented here provides a biological roadmap, a detailed chart showing the connections between your internal chemistry, your brain’s physical structure, and the daily choices you make. This knowledge moves the conversation about midlife cognitive changes from one of passive observation to one of active participation.
The feelings of brain fog or lapses in memory are real signals from a system in transition. The critical insight is that you possess the tools to send powerful signals back to that system.
Consider your next meal or your next opportunity for physical movement. View these actions not as tasks to be completed, but as opportunities to communicate with your own physiology. What message do you wish to send? Is it a message of nourishment and anti-inflammatory support through a plate of colorful vegetables and healthy fats?
Is it a message of regeneration and growth, sent by elevating your heart rate and moving your body? Each choice is a data point, an input into the complex equation of your long-term health. The path forward involves becoming a conscious architect of these inputs, learning to listen to your body’s feedback, and cultivating a sense of partnership with your own biology. This journey of self-regulation and proactive wellness is the ultimate expression of personalized medicine.

Glossary

testosterone

estradiol

lifestyle interventions

hormonal decline

mediterranean diet

oxidative stress

brain-derived neurotrophic factor

synaptic plasticity

brain health

blood-brain barrier

vascular endothelial growth factor

adult hippocampal neurogenesis

insulin sensitivity

growth factor

polyphenols

fatty acids

neuroinflammation

myokines