
Fundamentals
Have you found yourself grappling with a persistent sense of fatigue, a diminished drive, or perhaps a subtle shift in your physical and mental resilience? Many individuals experience these sensations, often attributing them to the natural progression of years or the relentless pace of modern existence.
Yet, beneath these common experiences often lies a more intricate biological narrative, one involving the delicate balance of the body’s internal messengers ∞ hormones. Understanding these biochemical signals, particularly testosterone, offers a pathway to regaining a sense of vigor and functional capacity.
Testosterone, a steroid hormone, plays a central role in both male and female physiology, extending far beyond its commonly recognized association with male characteristics. In men, it is primarily synthesized in the testes, while in women, the ovaries and adrenal glands produce smaller, yet physiologically significant, quantities.
This biochemical agent acts as a master regulator, influencing a wide array of bodily systems. Its presence is critical for maintaining muscle mass, supporting bone density, regulating mood, sustaining cognitive clarity, and influencing metabolic function. When its levels deviate from optimal ranges, the body’s intricate machinery can begin to falter, leading to the very symptoms many individuals report.
The body’s endocrine system operates as a sophisticated communication network, with hormones serving as the messages dispatched throughout the system. Consider the hypothalamic-pituitary-gonadal (HPG) axis as the central command center for testosterone regulation. The hypothalamus, a region in the brain, initiates the process by releasing gonadotropin-releasing hormone (GnRH).
This signal prompts the pituitary gland, situated at the base of the brain, to secrete two additional hormones ∞ luteinizing hormone (LH) and follicle-stimulating hormone (FSH). LH then travels to the gonads ∞ the testes in men, ovaries in women ∞ stimulating them to produce testosterone. This elegant feedback loop ensures that testosterone levels are tightly controlled, adjusting production based on the body’s current needs.
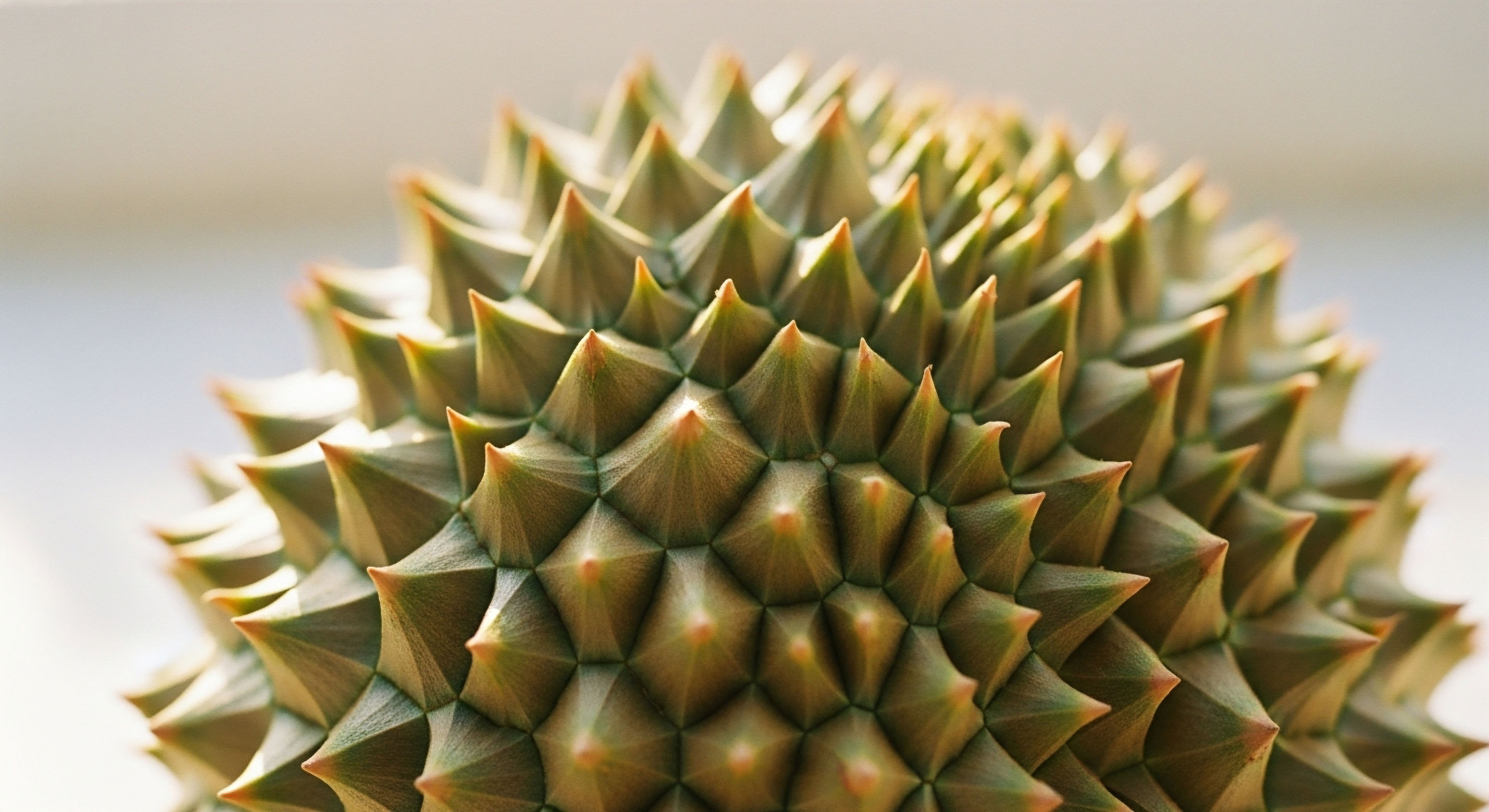
The body’s hormonal system acts as a complex internal communication network, with testosterone serving as a vital messenger influencing multiple physiological processes.
When this finely tuned system experiences disruptions, the consequences can manifest in a variety of ways. For men, declining testosterone levels, often termed andropause or late-onset hypogonadism, can present as reduced energy, decreased libido, changes in body composition (such as increased abdominal adiposity and reduced lean muscle), and even shifts in emotional well-being.
Women, too, can experience symptoms related to suboptimal testosterone, particularly during peri-menopause and post-menopause, which may include diminished libido, persistent fatigue, and a reduced sense of vitality. Recognizing these signals as potential indicators of hormonal imbalance is the initial step toward addressing them.
Lifestyle adjustments offer a foundational strategy for supporting hormonal equilibrium. These are not merely superficial changes; they represent a deep recalibration of daily habits that directly influence the body’s biochemical environment. The human body possesses an inherent capacity for self-regulation, and by providing it with the appropriate inputs, we can often optimize its natural processes.
This involves a comprehensive approach that considers nutrition, physical activity, sleep quality, and stress management. Each of these elements interacts with the endocrine system, either supporting or hindering its optimal function.

The Interconnectedness of Biological Systems
The endocrine system does not operate in isolation. It is inextricably linked with metabolic pathways, the immune system, and even neurological function. For instance, chronic stress, mediated by the hormone cortisol, can directly suppress testosterone production by interfering with the HPG axis.
Similarly, suboptimal metabolic health, characterized by insulin resistance or excess adiposity, can alter the conversion and clearance of hormones, leading to imbalances. Addressing these broader systemic influences becomes a fundamental aspect of any strategy aimed at optimizing testosterone levels and enhancing overall well-being.
Consider the impact of nutrition. The building blocks for hormone synthesis, including cholesterol, are derived from dietary intake. A diet lacking in essential micronutrients or healthy fats can impede the body’s ability to produce hormones effectively. Conversely, a diet rich in whole, unprocessed foods provides the necessary substrates and cofactors for robust endocrine function. Similarly, regular physical activity, particularly resistance training, has been shown to stimulate testosterone production and improve insulin sensitivity, thereby creating a more favorable hormonal environment.

Why Does Lifestyle Matter for Hormonal Balance?
The body’s internal environment is constantly responding to external cues. The food we consume, the movement we engage in, the quality of our rest, and the way we manage psychological pressures all send signals that either promote or disrupt hormonal harmony. These daily inputs collectively shape the body’s biochemical landscape.
When these inputs are consistently aligned with physiological needs, the body’s innate capacity for balance is reinforced. Conversely, a sustained pattern of unsupportive lifestyle choices can gradually erode hormonal resilience, leading to the symptoms of imbalance.
Understanding this dynamic relationship between daily habits and hormonal health empowers individuals to take an active role in their own physiological recalibration. It shifts the perspective from passively experiencing symptoms to proactively influencing the underlying biological mechanisms. This journey begins with a clear recognition of the body’s signals and a commitment to providing the foundational support it requires to function optimally.


Intermediate
Once foundational lifestyle adjustments are in place, a deeper exploration into specific clinical protocols can be considered for individuals seeking to optimize their hormonal landscape. These interventions are designed to address more significant imbalances or to support specific physiological goals, always within a framework of personalized care. The application of these protocols requires a precise understanding of their mechanisms and a careful consideration of individual biochemical profiles.
Testosterone Replacement Therapy (TRT) represents a primary intervention for men experiencing clinically low testosterone levels, a condition known as hypogonadism. The objective of TRT is to restore testosterone to physiological ranges, thereby alleviating symptoms and improving quality of life. A common protocol involves weekly intramuscular injections of Testosterone Cypionate, typically at a concentration of 200mg/ml. This method provides a stable release of the hormone, mimicking the body’s natural pulsatile secretion to some extent.

Male Hormone Optimization Protocols
Beyond direct testosterone administration, a comprehensive male hormone optimization protocol often includes additional agents to manage potential side effects and preserve endogenous function.
- Gonadorelin ∞ This synthetic peptide, administered via subcutaneous injections twice weekly, stimulates the pituitary gland to release LH and FSH. Its inclusion helps maintain the testes’ natural production of testosterone and supports fertility, which can be suppressed by exogenous testosterone administration.
- Anastrozole ∞ As an aromatase inhibitor, Anastrozole is typically prescribed as an oral tablet twice weekly. Its role is to mitigate the conversion of testosterone into estrogen, preventing potential estrogen-related side effects such as gynecomastia or fluid retention.
- Enclomiphene ∞ This selective estrogen receptor modulator (SERM) may be incorporated to directly support LH and FSH levels, particularly for men who wish to maintain or restore their natural testosterone production and fertility without direct testosterone administration.
The precise dosage and combination of these agents are tailored to each individual, guided by regular laboratory assessments of testosterone, estrogen, and other relevant biomarkers. This individualized approach ensures that the therapy is both effective and well-tolerated.
Personalized hormone optimization protocols extend beyond simple replacement, often incorporating agents to preserve natural function and manage biochemical conversions.

Female Hormone Balance and Testosterone
Testosterone also plays a vital, though often overlooked, role in female health. Women experiencing symptoms such as irregular cycles, mood fluctuations, hot flashes, or diminished libido, particularly during peri-menopause and post-menopause, may benefit from targeted testosterone support.
Protocols for women typically involve much lower doses than those for men, reflecting physiological differences. Testosterone Cypionate can be administered weekly via subcutaneous injection, often in very small quantities, such as 10 ∞ 20 units (0.1 ∞ 0.2ml). This micro-dosing approach aims to restore testosterone to optimal female physiological ranges, not male ranges.
Progesterone is another critical component of female hormone balance, prescribed based on menopausal status. For pre-menopausal and peri-menopausal women, it can help regulate menstrual cycles and alleviate symptoms like mood changes and sleep disturbances. In post-menopausal women, progesterone is often used in conjunction with estrogen therapy to protect the uterine lining.
Another delivery method for testosterone in women is pellet therapy. Long-acting testosterone pellets are inserted subcutaneously, providing a consistent release of the hormone over several months. Anastrozole may be used with pellet therapy when appropriate, particularly if there is a concern about excessive estrogen conversion.

Growth Hormone Peptide Therapy
Beyond steroid hormones, peptide therapies offer another avenue for physiological optimization, particularly for active adults and athletes seeking improvements in body composition, recovery, and overall vitality. These peptides work by stimulating the body’s natural production of growth hormone, rather than directly administering it.
Key peptides in this category include:
- Sermorelin ∞ A growth hormone-releasing hormone (GHRH) analog that stimulates the pituitary gland to release growth hormone. It is often used for anti-aging benefits, improved sleep, and enhanced recovery.
- Ipamorelin / CJC-1295 ∞ This combination acts synergistically to increase growth hormone secretion. Ipamorelin is a growth hormone secretagogue, while CJC-1295 is a GHRH analog. Together, they promote muscle gain, fat loss, and improved sleep architecture.
- Tesamorelin ∞ A GHRH analog specifically approved for reducing visceral adipose tissue in certain conditions, but also used off-label for its body composition benefits.
- Hexarelin ∞ Another growth hormone secretagogue, often used for its potent effects on growth hormone release and potential for muscle growth.
- MK-677 ∞ An oral growth hormone secretagogue that stimulates growth hormone release by mimicking the action of ghrelin. It is often used for its effects on sleep, body composition, and appetite.
These peptides are typically administered via subcutaneous injection, with specific dosing protocols tailored to individual goals and responses.

Other Targeted Peptides for Specific Needs
The therapeutic landscape of peptides extends to addressing specific physiological needs beyond growth hormone optimization.
- PT-141 (Bremelanotide) ∞ This peptide targets melanocortin receptors in the brain, influencing sexual function. It is used to address sexual health concerns, particularly low libido, in both men and women, by acting on central nervous system pathways.
- Pentadeca Arginate (PDA) ∞ This peptide is recognized for its potential in tissue repair, healing processes, and modulating inflammatory responses. It supports the body’s regenerative capacities, making it relevant for recovery from injury or chronic inflammatory states.
The application of these peptides represents a sophisticated approach to supporting specific biological functions, moving beyond broad hormonal adjustments to target precise physiological pathways.

Comparing Hormone Optimization Protocols
The selection of a specific protocol depends on the individual’s unique physiological presentation, symptoms, and desired outcomes. A detailed assessment of laboratory values, clinical history, and lifestyle factors guides the choice of therapeutic agents and their administration.
| Protocol Category | Primary Target Audience | Key Agents | Primary Benefits |
|---|---|---|---|
| Male TRT | Men with low testosterone symptoms | Testosterone Cypionate, Gonadorelin, Anastrozole, Enclomiphene | Improved energy, libido, muscle mass, mood, cognitive function |
| Female Hormone Balance | Women with hormonal symptoms (peri/post-menopause) | Testosterone Cypionate (low dose), Progesterone, Anastrozole (pellets) | Enhanced libido, mood stability, reduced hot flashes, vitality |
| Growth Hormone Peptides | Active adults, athletes seeking anti-aging, recovery | Sermorelin, Ipamorelin/CJC-1295, Tesamorelin, Hexarelin, MK-677 | Improved body composition, sleep quality, recovery, anti-aging effects |
| Targeted Peptides | Individuals with specific sexual health or tissue repair needs | PT-141, Pentadeca Arginate | Enhanced sexual function, accelerated tissue healing, inflammation modulation |
Each protocol is a component of a broader strategy aimed at restoring physiological balance and enhancing well-being. The integration of these clinical interventions with ongoing lifestyle adjustments creates a powerful synergy, supporting the body’s capacity for optimal function and vitality.


Academic
A deep understanding of how lifestyle adjustments can influence testosterone levels and overall well-being necessitates an academic exploration of the intricate endocrinological and metabolic pathways involved. The human body operates as a complex adaptive system, where seemingly disparate inputs converge to shape hormonal output and systemic health. This section will delve into the molecular and physiological underpinnings, drawing connections between cellular mechanisms and macroscopic well-being.
The regulation of testosterone production is a prime example of a sophisticated biological feedback loop. The HPG axis, as previously mentioned, is central to this regulation. The pulsatile release of GnRH from the hypothalamus stimulates the anterior pituitary to secrete LH and FSH.
LH then acts on Leydig cells in the testes (in men) or theca cells in the ovaries (in women) to stimulate androgen synthesis. FSH, in men, primarily supports spermatogenesis by acting on Sertoli cells, while in women, it promotes follicular development.
The resulting testosterone and estrogen then exert negative feedback on both the hypothalamus and the pituitary, modulating GnRH, LH, and FSH release to maintain homeostasis. Disruptions at any point in this axis, whether due to chronic stress, nutritional deficiencies, or inflammatory states, can alter the delicate balance of hormonal signaling.

Metabolic Interplay and Androgen Homeostasis
The relationship between metabolic health and androgen homeostasis is bidirectional and highly significant. Conditions such as insulin resistance and obesity are strongly correlated with lower testosterone levels in men. Adipose tissue, particularly visceral fat, is metabolically active and contains the enzyme aromatase, which converts androgens (like testosterone) into estrogens.
An increase in aromatase activity due to excess adiposity leads to higher estrogen levels, which in turn exert stronger negative feedback on the HPG axis, suppressing endogenous testosterone production. This creates a vicious cycle where low testosterone can exacerbate fat accumulation, and excess fat can further suppress testosterone.
Furthermore, insulin resistance can directly impair Leydig cell function, reducing their capacity to synthesize testosterone. Chronic inflammation, often associated with obesity and metabolic dysfunction, also plays a role. Inflammatory cytokines can interfere with hypothalamic and pituitary signaling, further contributing to hypogonadism. This highlights why lifestyle interventions targeting metabolic health ∞ such as dietary modifications to improve insulin sensitivity and regular physical activity to reduce adiposity ∞ are not merely adjuncts but fundamental components of testosterone optimization strategies.

The Role of Neurotransmitters and Stress Response
The brain’s neurochemical environment profoundly influences hormonal regulation. Neurotransmitters like dopamine and norepinephrine are involved in the pulsatile release of GnRH. Chronic psychological stress activates the hypothalamic-pituitary-adrenal (HPA) axis, leading to sustained elevation of cortisol. Cortisol, a glucocorticoid, can directly inhibit GnRH release from the hypothalamus and reduce the sensitivity of Leydig cells to LH, thereby suppressing testosterone synthesis. This phenomenon, often termed “stress-induced hypogonadism,” illustrates the deep interconnectedness between mental well-being and endocrine function.
Sleep deprivation also impacts this delicate balance. Growth hormone and testosterone are predominantly secreted during deep sleep phases. Chronic insufficient sleep can disrupt these natural secretory patterns, leading to suboptimal levels of both hormones. This reinforces the clinical importance of prioritizing sleep hygiene as a non-pharmacological intervention for hormonal support.
The intricate dance between metabolic function, neurotransmitter activity, and the HPG axis dictates the body’s capacity for optimal testosterone production.

Pharmacological Mechanisms of Hormone Optimization
When lifestyle adjustments alone are insufficient, targeted pharmacological interventions can precisely recalibrate the endocrine system.
Testosterone Cypionate, an esterified form of testosterone, provides a sustained release due to its oil-based vehicle and ester linkage, allowing for less frequent administration compared to unesterified testosterone. Once injected, the ester bond is cleaved by esterases in the bloodstream, releasing free testosterone. This free testosterone then binds to androgen receptors within target cells, initiating gene transcription and protein synthesis, leading to its diverse physiological effects.
Gonadorelin, a synthetic GnRH analog, acts directly on GnRH receptors in the anterior pituitary, stimulating the release of endogenous LH and FSH. This mechanism helps to preserve testicular function and spermatogenesis in men undergoing exogenous testosterone therapy, which would otherwise suppress the HPG axis through negative feedback.
Anastrozole, an aromatase inhibitor, works by reversibly binding to the aromatase enzyme, preventing the conversion of androgens to estrogens. This is particularly relevant in men on TRT to manage supraphysiological estrogen levels that can arise from increased substrate (testosterone) for aromatization.
Sermorelin and Ipamorelin/CJC-1295 operate by different mechanisms to stimulate growth hormone release. Sermorelin is a GHRH mimetic, binding to GHRH receptors on somatotrophs in the pituitary, leading to a pulsatile release of growth hormone. Ipamorelin, a ghrelin mimetic, binds to the growth hormone secretagogue receptor (GHSR), also stimulating growth hormone release, while CJC-1295 is a long-acting GHRH analog. Their combined action can significantly amplify endogenous growth hormone secretion, influencing protein synthesis, lipolysis, and tissue repair.

The Future of Personalized Endocrine Support
The trajectory of endocrine support is moving toward increasingly personalized and data-driven protocols. Advanced diagnostics, including comprehensive hormone panels, genetic predispositions, and metabolic markers, allow for a more precise understanding of an individual’s unique biochemical needs. This granular data informs the selection of specific agents, dosages, and administration routes, moving beyond a one-size-fits-all approach.
The integration of lifestyle interventions with targeted pharmacological or peptide therapies represents a sophisticated strategy for optimizing hormonal health. This approach acknowledges the body’s inherent complexity and its capacity for self-regulation when provided with the correct internal and external signals. The goal remains to restore physiological balance, thereby enhancing vitality, functional capacity, and overall well-being.
| Hormone/Peptide | Primary Source | Key Interacting System(s) | Physiological Impact |
|---|---|---|---|
| Testosterone | Testes, Ovaries, Adrenals | HPG Axis, Metabolic System, Musculoskeletal System, Nervous System | Muscle mass, bone density, libido, mood, cognitive function, fat metabolism |
| Estrogen | Ovaries, Adipose Tissue (via aromatase) | HPG Axis, Cardiovascular System, Bone Health | Reproductive function, bone density, cardiovascular health, mood regulation |
| Cortisol | Adrenal Glands | HPA Axis, Immune System, Metabolic System | Stress response, glucose regulation, inflammation modulation, immune suppression |
| Growth Hormone | Pituitary Gland | Metabolic System, Musculoskeletal System, Immune System | Protein synthesis, fat metabolism, tissue repair, immune function, bone growth |
| Insulin | Pancreas | Metabolic System, Adipose Tissue, Musculoskeletal System | Glucose uptake, energy storage, protein synthesis, fat storage |
This systems-biology perspective underscores that optimizing testosterone levels is not an isolated endeavor. It is a component of a broader strategy to recalibrate the entire physiological network, allowing individuals to reclaim their inherent capacity for health and high performance.

References
- Mooradian, A. D. Morley, J. E. & Korenman, S. G. (1987). Biological actions of androgens. Endocrine Reviews, 8(1), 1-28.
- Bhasin, S. et al. (2010). Testosterone therapy in men with androgen deficiency syndromes ∞ An Endocrine Society clinical practice guideline. Journal of Clinical Endocrinology & Metabolism, 95(6), 2536-2559.
- Traish, A. M. et al. (2009). The dark side of testosterone deficiency ∞ II. Type 2 diabetes and insulin resistance. Journal of Andrology, 30(1), 23-32.
- Veldhuis, J. D. et al. (2001). Sleep-wake cycle and the neuroendocrine axis. Journal of Clinical Endocrinology & Metabolism, 86(9), 4029-4036.
- Jones, T. H. & Saad, F. (2019). Testosterone Deficiency and Its Management. Springer.
- Miller, K. K. et al. (2013). Tesamorelin in HIV-infected patients with excess abdominal fat ∞ a randomized controlled trial. Journal of Clinical Endocrinology & Metabolism, 98(12), 4627-4636.
- Bassil, N. et al. (2009). The benefits and risks of testosterone replacement therapy ∞ a review. Therapeutics and Clinical Risk Management, 5(3), 427-448.
- Davis, S. R. et al. (2015). Global Consensus Position Statement on the Use of Testosterone Therapy for Women. Journal of Clinical Endocrinology & Metabolism, 100(10), 3487-3502.

Reflection
The journey toward optimizing hormonal health is deeply personal, reflecting the unique biochemical tapestry of each individual. Understanding the intricate connections between lifestyle choices, metabolic function, and the endocrine system provides a powerful framework for reclaiming vitality. This knowledge serves as a compass, guiding individuals to make informed decisions about their well-being.
Consider this exploration not as a destination, but as the initial steps on a path of continuous discovery. Your body communicates its needs through symptoms and sensations; learning to interpret these signals is a fundamental aspect of self-care. True well-being arises from a proactive engagement with your biological systems, supported by evidence-based strategies and personalized guidance.
The capacity to influence your own physiological state is a profound realization. By aligning your daily habits with your body’s inherent design, and by considering targeted clinical support when appropriate, you can unlock a renewed sense of energy, clarity, and functional capacity. This ongoing process of understanding and recalibration is the essence of a truly personalized health journey.



