

Fundamentals
Have you found yourself feeling a persistent lack of vitality, a subtle yet pervasive shift in your energy levels, or perhaps a change in your body composition that seems resistant to your usual efforts?
Many women experience these sensations, often dismissing them as simply “getting older” or “stress.” This lived experience, however, frequently points to deeper physiological currents, particularly within the intricate realm of hormonal balance and metabolic function. Understanding these internal systems is the first step toward reclaiming your sense of well-being and optimizing your health trajectory.
Your body operates as a complex, interconnected network, where hormones serve as essential messengers, orchestrating nearly every biological process. From regulating your mood and sleep cycles to governing your energy expenditure and body weight, these biochemical signals play a central role. When these signals become dysregulated, even subtly, the ripple effects can be felt across multiple systems, manifesting as the very symptoms you might be experiencing.
Metabolic syndrome represents a cluster of conditions that collectively elevate the risk for cardiovascular disease and type 2 diabetes. These conditions include elevated blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol or triglyceride levels. While often discussed in terms of lifestyle factors, the profound influence of the endocrine system on metabolic health is increasingly recognized. Hormonal optimization protocols offer a pathway to address these underlying imbalances, moving beyond symptomatic management to target systemic recalibration.
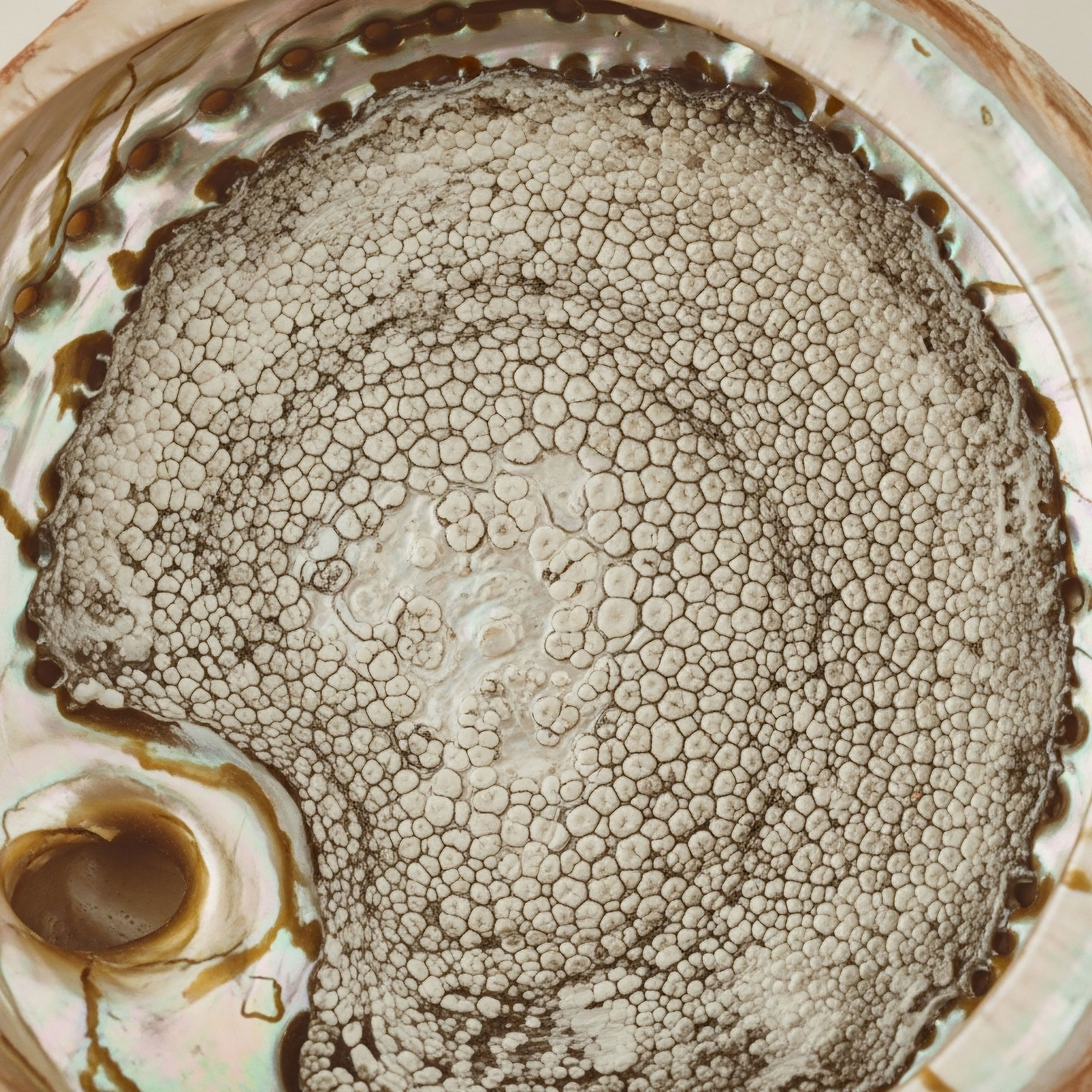
Hormonal balance is a foundational element for metabolic health, influencing energy regulation and systemic well-being.
The endocrine system, a collection of glands that produce and secrete hormones, acts as the body’s master regulator. Consider the hypothalamic-pituitary-gonadal (HPG) axis, a sophisticated feedback loop involving the brain and reproductive glands. This axis does not operate in isolation; it constantly communicates with other endocrine glands, such as the thyroid and adrenal glands, and significantly impacts metabolic pathways. For instance, sex hormones like estrogen and testosterone influence insulin sensitivity, fat distribution, and energy metabolism.
When hormonal levels deviate from their optimal ranges, particularly during life stages such as perimenopause and post-menopause, the body’s metabolic equilibrium can be disrupted. This disruption can contribute to the development or worsening of metabolic syndrome components. Addressing these hormonal shifts with precision can therefore be a powerful strategy in mitigating metabolic risk and restoring systemic harmony.

Understanding Hormonal Communication
Hormones function much like a sophisticated internal messaging service, transmitting instructions from one part of the body to another. These chemical messengers travel through the bloodstream, binding to specific receptors on target cells to elicit a particular response. The precision of this communication is paramount for maintaining physiological balance. When the production of these messengers falters, or when cellular receptors become less responsive, the entire system can experience a cascade of downstream effects.
For women, the fluctuations of estrogen and progesterone throughout the menstrual cycle, and especially during the menopausal transition, directly influence metabolic parameters. Estrogen, for example, plays a protective role in cardiovascular health and helps maintain insulin sensitivity. As estrogen levels decline, women may experience increased visceral fat accumulation, alterations in lipid profiles, and a greater propensity for insulin resistance, all contributing factors to metabolic syndrome.
The Endocrine System’s Metabolic Influence
The endocrine system’s influence extends deeply into metabolic regulation. Key hormones involved include ∞
- Insulin ∞ Produced by the pancreas, it regulates blood glucose levels by facilitating glucose uptake into cells. Hormonal imbalances can impair insulin sensitivity.
- Thyroid Hormones ∞ Triiodothyronine (T3) and Thyroxine (T4) regulate basal metabolic rate, influencing energy expenditure and weight management.
- Cortisol ∞ A stress hormone from the adrenal glands, chronic elevation can lead to increased blood sugar, central adiposity, and insulin resistance.
- Estrogen and Progesterone ∞ These sex hormones impact fat distribution, glucose metabolism, and cardiovascular health.
- Testosterone ∞ While often associated with men, testosterone in women plays a role in muscle mass, bone density, and metabolic function.
Recognizing the interconnectedness of these hormonal signals provides a more comprehensive understanding of metabolic health. It moves beyond viewing metabolic syndrome as merely a consequence of diet and exercise, instead considering the intricate biochemical landscape that shapes an individual’s susceptibility and resilience. This holistic perspective is foundational to developing personalized wellness protocols that truly address the root causes of imbalance.


Intermediate
For women navigating the complexities of hormonal shifts, particularly during perimenopause and post-menopause, specific clinical protocols offer targeted support. These interventions aim to restore physiological balance, thereby influencing metabolic health and overall vitality. Understanding the precise mechanisms and applications of these therapies is essential for making informed decisions about personal wellness.
The concept of hormonal optimization extends beyond simply replacing deficient hormones; it involves a careful recalibration of the body’s internal systems to function at their best. This approach recognizes that symptoms like irregular cycles, mood changes, hot flashes, and diminished libido are not isolated occurrences but rather manifestations of systemic imbalances that can impact metabolic pathways.

Testosterone Replacement Therapy for Women
While often associated with male health, testosterone plays a significant role in female physiology, influencing energy, mood, muscle mass, bone density, and sexual function. As women age, particularly during the menopausal transition, natural testosterone levels decline. This reduction can contribute to symptoms that overlap with metabolic dysfunction, such as increased body fat, reduced lean muscle mass, and fatigue.
Protocols for women typically involve very low doses compared to those used for men, reflecting the physiological differences in hormonal requirements. A common approach utilizes Testosterone Cypionate, administered weekly via subcutaneous injection. Dosages often range from 10 ∞ 20 units (0.1 ∞ 0.2ml), carefully titrated based on individual response and laboratory monitoring. This method allows for consistent delivery and avoids the peaks and troughs associated with less frequent administration.
Precise testosterone dosing for women can improve body composition and metabolic markers.
The inclusion of Progesterone is a critical component of female hormonal optimization, particularly for women who still have a uterus or are post-menopausal. Progesterone balances estrogen’s effects on the uterine lining and contributes to mood stability, sleep quality, and bone health. Its prescription is tailored to the woman’s menopausal status, often administered orally or transdermally.
Another delivery method for testosterone is Pellet Therapy, where small, custom-compounded pellets are inserted subcutaneously, providing a steady release of testosterone over several months. This can be a convenient option for some individuals, eliminating the need for weekly injections.
When appropriate, Anastrozole may be included in certain protocols, particularly if there is a concern about excessive testosterone conversion to estrogen, which can occur in some individuals and potentially lead to undesirable effects. This medication acts as an aromatase inhibitor, reducing estrogen synthesis.

Growth Hormone Peptide Therapy
Growth hormone (GH) and its stimulating peptides represent another frontier in metabolic and anti-aging protocols. These peptides do not directly replace GH but rather stimulate the body’s own pituitary gland to produce and release more GH, mimicking natural physiological rhythms. This approach can be beneficial for active adults and athletes seeking improvements in body composition, recovery, and overall vitality.
Key peptides in this category include ∞
- Sermorelin ∞ A growth hormone-releasing hormone (GHRH) analog that stimulates the pituitary to release GH. It promotes fat loss, muscle gain, and improved sleep quality.
- Ipamorelin / CJC-1295 ∞ This combination acts synergistically. Ipamorelin is a selective GH secretagogue, while CJC-1295 (without DAC) is a GHRH analog.
Together, they promote a sustained, pulsatile release of GH, supporting muscle development, fat reduction, and enhanced recovery.
- Tesamorelin ∞ A GHRH analog specifically approved for reducing visceral adipose tissue in certain populations. It directly targets central fat accumulation, a significant component of metabolic syndrome.
- Hexarelin ∞ Another GH secretagogue that also exhibits cardioprotective effects and can support muscle growth.
- MK-677 (Ibutamoren) ∞ An oral GH secretagogue that increases GH and IGF-1 levels, promoting muscle mass, bone density, and sleep quality.
The influence of these peptides on metabolic syndrome risk is indirect but significant. By promoting lean muscle mass, reducing adipose tissue, and improving insulin sensitivity, they contribute to a healthier metabolic profile. The enhanced recovery and sleep quality also play a role in reducing systemic stress, which can otherwise negatively impact metabolic function.

Other Targeted Peptides
Beyond growth hormone secretagogues, other peptides offer specific therapeutic benefits that can indirectly support metabolic health by addressing related concerns.
PT-141 (Bremelanotide) is a melanocortin receptor agonist primarily used for sexual health, addressing conditions like hypoactive sexual desire disorder in women. While its direct impact on metabolic syndrome is not primary, improved sexual function can contribute to overall well-being and quality of life, which are important aspects of a holistic health approach.
Pentadeca Arginate (PDA) is a peptide being explored for its roles in tissue repair, healing, and inflammation modulation. Chronic inflammation is a known contributor to insulin resistance and the progression of metabolic syndrome. By potentially mitigating inflammatory processes, PDA could offer supportive benefits in maintaining metabolic equilibrium.

Comparing Hormonal Optimization Protocols
The selection of a specific protocol depends on individual needs, symptoms, and laboratory findings. A comprehensive assessment is always necessary to tailor the most effective and safest approach.
| Protocol Type | Primary Target | Key Benefits for Women | Potential Metabolic Influence |
|---|---|---|---|
| Testosterone Optimization | Low testosterone symptoms | Improved libido, energy, mood, muscle mass, bone density | Reduced visceral fat, improved insulin sensitivity, enhanced lean mass |
| Progesterone Supplementation | Hormonal balance, uterine health | Mood stability, better sleep, bone protection | Indirectly supports metabolic balance by reducing stress and improving sleep |
| Growth Hormone Peptides | GH deficiency symptoms, anti-aging | Increased muscle mass, fat loss, improved skin elasticity, better sleep | Direct reduction of adipose tissue, improved glucose metabolism, enhanced energy expenditure |
| Targeted Peptides (e.g. PDA) | Specific physiological concerns | Tissue repair, inflammation reduction, sexual health | Modulation of inflammatory pathways, indirect metabolic support |
Each protocol is a tool in a broader strategy to restore systemic balance. The aim is to create an internal environment where the body can naturally regulate its metabolic processes more effectively, moving away from a state of dysfunction toward optimal function. This requires careful monitoring and adjustment, ensuring that the body’s responses are aligned with the desired physiological outcomes.


Academic
The relationship between hormonal optimization protocols and metabolic syndrome risk in women extends into the deep complexities of endocrinology and systems biology. This section explores the intricate interplay of biological axes, metabolic pathways, and cellular signaling that underpins this connection, providing a more granular understanding of how targeted interventions can influence systemic health.
Metabolic syndrome is not a singular disease but a constellation of interconnected metabolic dysregulations. Its development is significantly influenced by the endocrine system, which acts as the central command for energy homeostasis. When the delicate balance of hormones is disturbed, particularly sex steroids, the body’s ability to manage glucose, lipids, and energy expenditure is compromised, paving the way for metabolic dysfunction.

Endocrine Axes and Metabolic Interplay
The hypothalamic-pituitary-gonadal (HPG) axis, responsible for regulating reproductive function, is inextricably linked with metabolic health. Estrogen, particularly estradiol, plays a protective role in metabolic function. It influences insulin sensitivity, lipid metabolism, and fat distribution.
As women transition through perimenopause and into post-menopause, the decline in ovarian estrogen production leads to a shift in fat accumulation from subcutaneous to visceral depots. Visceral fat is metabolically active, secreting pro-inflammatory adipokines and cytokines that contribute to systemic inflammation and insulin resistance.
Testosterone, while present in lower concentrations in women, also holds metabolic significance. Optimal testosterone levels in women are associated with healthier body composition, including greater lean muscle mass and reduced adiposity. Low testosterone in women has been correlated with increased insulin resistance and higher prevalence of metabolic syndrome components. The precise mechanisms involve testosterone’s influence on glucose transporter proteins and its role in muscle glucose uptake.
Hormonal shifts during menopause directly impact fat distribution and insulin sensitivity.
Beyond the HPG axis, the hypothalamic-pituitary-adrenal (HPA) axis, governing the stress response, also profoundly impacts metabolism. Chronic activation of the HPA axis leads to sustained elevation of cortisol. High cortisol levels promote gluconeogenesis, increase insulin resistance, and encourage central fat deposition, all of which are direct contributors to metabolic syndrome. The interplay here is bidirectional ∞ hormonal imbalances can heighten stress responses, and chronic stress can further disrupt hormonal equilibrium.

Cellular Mechanisms of Hormonal Influence
At the cellular level, hormones exert their effects by binding to specific receptors, initiating a cascade of intracellular signaling events that ultimately alter gene expression and cellular function. For instance, estrogen receptors (ERα and ERβ) are widely distributed in metabolic tissues, including adipose tissue, liver, and skeletal muscle. Activation of these receptors by estradiol influences mitochondrial function, glucose utilization, and lipid synthesis. A decline in estrogen signaling can therefore lead to mitochondrial dysfunction and impaired metabolic flexibility.
Insulin resistance, a hallmark of metabolic syndrome, involves a reduced responsiveness of cells to insulin’s action, leading to elevated blood glucose. Hormonal imbalances can exacerbate this. For example, reduced estrogen can impair the insulin signaling pathway, specifically affecting the phosphatidylinositol 3-kinase (PI3K)/Akt pathway, which is critical for glucose uptake.
Similarly, chronic inflammation, often fueled by excess visceral fat and hormonal dysregulation, can induce insulin resistance through activation of inflammatory kinases like JNK and IKKβ, which interfere with insulin receptor signaling.

Targeted Protocols and Metabolic Outcomes
Hormonal optimization protocols aim to restore physiological hormone levels, thereby influencing these cellular and systemic mechanisms.
Testosterone Replacement Therapy (TRT) in women, when administered at appropriate physiological doses, can improve insulin sensitivity and body composition. Studies indicate that optimizing testosterone levels can lead to a reduction in visceral fat and an increase in lean muscle mass, both of which are protective against metabolic syndrome. The enhanced muscle mass improves glucose disposal, while reduced visceral fat lessens the secretion of pro-inflammatory adipokines.
Growth Hormone Peptide Therapy, by stimulating endogenous GH production, indirectly influences metabolic pathways. GH promotes lipolysis (fat breakdown) and reduces adiposity, particularly visceral fat. It also influences glucose metabolism, though its effects can be complex, sometimes leading to transient insulin resistance at supraphysiological levels.
However, when used to restore more physiological GH pulsatility, the overall metabolic impact is often beneficial, contributing to improved body composition and energy expenditure. Peptides like Tesamorelin have demonstrated efficacy in reducing visceral fat in clinical trials, directly addressing a core component of metabolic syndrome.

The Role of Adipokines and Cytokines
Adipose tissue, particularly visceral fat, is not merely an energy storage depot; it is an active endocrine organ that secretes a variety of hormones and signaling molecules known as adipokines. These include leptin, adiponectin, resistin, and inflammatory cytokines like TNF-α and IL-6.
| Adipokine/Cytokine | Source | Metabolic Role | Influence of Hormonal Imbalance |
|---|---|---|---|
| Leptin | Adipose tissue | Regulates appetite and energy balance; high levels indicate leptin resistance in obesity | Increased in obesity, often exacerbated by hormonal dysregulation (e.g.
low estrogen) |
| Adiponectin | Adipose tissue | Enhances insulin sensitivity, anti-inflammatory, cardioprotective | Decreased in obesity and metabolic syndrome; potentially improved with hormonal optimization |
| Resistin | Adipose tissue, immune cells | Promotes insulin resistance and inflammation | Elevated in metabolic syndrome; potentially influenced by sex hormone levels |
| TNF-α (Tumor Necrosis Factor-alpha) | Adipose tissue, immune cells | Pro-inflammatory cytokine, induces insulin resistance | Increased with visceral adiposity and chronic inflammation, often linked to hormonal shifts |
| IL-6 (Interleukin-6) | Adipose tissue, immune cells | Pro-inflammatory cytokine, influences glucose and lipid metabolism | Elevated in metabolic syndrome; hormonal balance can modulate its production |
Hormonal imbalances, such as estrogen deficiency, can alter the secretion profile of these adipokines, favoring a pro-inflammatory and insulin-resistant state. By restoring hormonal balance, optimization protocols can positively influence the adipokine milieu, thereby mitigating systemic inflammation and improving insulin sensitivity. This systemic recalibration underscores the profound impact of hormonal health on the very core of metabolic function.

Can Hormonal Optimization Protocols Influence Metabolic Syndrome Progression?
The evidence suggests that targeted hormonal optimization can indeed influence the progression of metabolic syndrome in women. By addressing underlying hormonal deficiencies and imbalances, these protocols work to ∞
- Improve Insulin Sensitivity ∞ Restoring optimal estrogen and testosterone levels can enhance cellular responsiveness to insulin, leading to better glucose regulation.
- Modulate Adiposity ∞ Shifting fat distribution away from metabolically active visceral fat and promoting lean muscle mass.
- Reduce Systemic Inflammation ∞ By influencing adipokine secretion and reducing pro-inflammatory cytokines.
- Support Lipid Metabolism ∞ Positively impacting cholesterol and triglyceride profiles.
- Regulate Blood Pressure ∞ Indirectly through improved metabolic health and reduced inflammation.
The integration of these protocols within a comprehensive wellness strategy, including nutritional guidance and appropriate physical activity, offers a powerful synergistic effect. It is a testament to the body’s remarkable capacity for self-regulation when provided with the precise biochemical support it requires. The aim is not merely to alleviate symptoms but to fundamentally re-establish a state of metabolic resilience and long-term health.

References
- Davis, S. R. & Wahlin-Jacobsen, S. (2015). Testosterone in women ∞ the clinical significance. The Lancet Diabetes & Endocrinology, 3(12), 980-992.
- Wild, R. A. (2012). Obesity, insulin resistance, androgens, and the polycystic ovary syndrome. Clinical Endocrinology, 77(4), 505-510.
- Chrousos, G. P. (2009). Stress and disorders of the stress system. Nature Reviews Endocrinology, 5(7), 374-381.
- Hotamisligil, G. S. (2006). Inflammation and metabolic disorders. Nature, 444(7121), 860-867.
- Traish, A. M. et al. (2014). The dark side of testosterone deficiency ∞ II. Type 2 diabetes and metabolic syndrome. Journal of Andrology, 35(6), 1115-1124.
- Stanley, T. L. et al. (2012). Effects of tesamorelin on visceral adipose tissue and metabolic parameters in HIV-infected patients with abdominal adiposity. Clinical Infectious Diseases, 54(12), 1790-1798.
- Mauvais-Jarvis, F. et al. (2013). Estrogen regulation of metabolism and body weight. Annual Review of Physiology, 75, 23-38.
- Pasquali, R. et al. (2011). The impact of obesity on the hypothalamic-pituitary-gonadal axis in men and women. Journal of Endocrinological Investigation, 34(10), 793-801.

Reflection
As you consider the intricate connections between your hormonal landscape and metabolic well-being, remember that this knowledge is a powerful tool. It is not about chasing an idealized state, but rather about understanding your unique biological blueprint and providing it with the precise support it needs to function optimally. Your personal health journey is a continuous process of discovery, where each symptom and sensation offers a clue to the underlying systems at play.
The insights shared here are designed to equip you with a deeper appreciation for your body’s remarkable intelligence. They invite you to move beyond generalized health advice and instead seek a personalized path, one that respects your individual physiology. True vitality is not a destination; it is a state of being that arises from aligning your internal environment with your innate capacity for health. Consider this exploration a foundational step in your ongoing pursuit of enduring well-being.



