Fundamentals
You may have noticed a subtle shift within your body’s internal landscape. The energy that once felt abundant now seems to wane more quickly. Maintaining a healthy body composition requires more effort than it used to, and recovery from physical exertion feels prolonged.
This lived experience is a valid and common starting point for a deeper inquiry into your own biology. These changes often originate from the intricate and interconnected world of your endocrine system, the body’s sophisticated communication network. At the heart of this network lies a molecule of profound importance to vitality and metabolic function ∞ human growth hormone (GH).
Its role extends far beyond childhood growth, continuing throughout adulthood to regulate metabolism, repair tissues, and maintain the structural integrity of your body.
As we age, the body’s natural production of growth hormone begins a gradual, persistent decline. This is a universal biological process. The clear, strong signals from the brain’s command center, the hypothalamus and pituitary gland, become quieter and less frequent.
The result is a diminished hormonal chorus, which can manifest as the very symptoms you may be feeling ∞ a slower metabolism, a gradual accumulation of fat, particularly around the midsection, and a loss of lean muscle mass. Understanding this connection is the first step toward reclaiming control over your metabolic destiny. It allows you to reframe your experience from one of passive acceptance to one of active, informed investigation.
The body’s metabolic rhythm is deeply tied to the precise signaling of hormones like human growth hormone.
Growth hormone peptides represent a specific and intelligent approach to addressing this decline. These are not synthetic hormones that flood the body with an external supply. They are small chains of amino acids, biological messengers designed to work with your body’s own machinery.
Think of them as precise keys that fit into specific locks within the pituitary gland, gently prompting it to produce and release your own natural growth hormone in a manner that mimics your body’s youthful, rhythmic pulses.
This strategy honors the body’s innate feedback loops, the internal checks and balances that ensure the endocrine system remains in a state of dynamic equilibrium. By supporting the body’s own production, these peptides help restore a more optimized hormonal environment, which is the foundation of robust metabolic health.

What Is Metabolic Health?
Metabolic health is a comprehensive state of well-being that defines how efficiently your body manages energy. It encompasses several key physiological processes that work in concert to maintain vitality. A healthy metabolism is characterized by the body’s ability to regulate blood sugar levels effectively, maintain a balanced profile of blood lipids like cholesterol and triglycerides, and manage inflammation.
It also involves maintaining a favorable body composition, with a healthy ratio of lean muscle mass to adipose tissue, especially visceral fat. When these systems are functioning optimally, you experience stable energy levels, mental clarity, and physical resilience. Disruptions in these areas are what lead to the metabolic challenges many adults face.

The Central Role of the GH Axis
The regulation of growth hormone is governed by the growth hormone axis, a complex feedback system involving the hypothalamus and the pituitary gland. The hypothalamus releases Growth Hormone-Releasing Hormone (GHRH), which signals the pituitary to secrete GH. This release is not constant; it occurs in pulses, primarily during deep sleep and after intense exercise.
Once in circulation, GH travels to the liver and other tissues, where it stimulates the production of Insulin-like Growth Factor 1 (IGF-1). It is IGF-1 that mediates many of GH’s anabolic, or tissue-building, effects. The entire system is self-regulating; high levels of IGF-1 signal the hypothalamus to slow down GHRH release, maintaining balance. Peptides work by interacting with this axis at different points to amplify the natural signaling process.
- Sermorelin ∞ This peptide is a GHRH analog. It directly mimics the body’s own GHRH, binding to its receptors on the pituitary gland to stimulate a natural pulse of growth hormone. Its action is consistent with the body’s inherent physiological processes.
- Ipamorelin ∞ This peptide works through a different but complementary pathway. It is a ghrelin mimetic, meaning it activates the ghrelin receptor in the pituitary. This action also stimulates GH release, but it does so with high specificity, avoiding the significant release of other hormones like cortisol.
- Tesamorelin ∞ Another potent GHRH analog, Tesamorelin has been extensively studied for its powerful effect on reducing visceral adipose tissue (VAT), the metabolically active fat stored deep within the abdominal cavity. Its primary strength lies in its ability to target this specific driver of metabolic disease.


Intermediate
Advancing from a foundational awareness of growth hormone peptides to an intermediate understanding requires a closer look at their precise mechanisms and clinical applications. The therapeutic goal of these protocols is to achieve a meaningful shift in metabolic outcomes by recalibrating the body’s endocrine signaling.
This involves more than just elevating growth hormone levels; it is about restoring the physiological rhythm and amplitude of GH release. The synergy between different classes of peptides is a key element of this sophisticated approach, allowing for a tailored and more potent stimulation of the body’s natural pathways. This nuanced strategy is what allows for significant improvements in body composition, lipid metabolism, and overall energy management.

The Mechanism of Action a Deeper Look
The effectiveness of growth hormone peptide therapy lies in its ability to leverage the body’s existing biological pathways. The pituitary gland has multiple receptors that can trigger the release of GH. By targeting these receptors with specific peptides, it is possible to amplify the body’s own production in a controlled manner. This is fundamentally different from administering synthetic HGH, which introduces a large, non-pulsatile amount of the hormone, potentially disrupting the delicate feedback loops of the endocrine system.
A common and highly effective strategy involves combining a GHRH analog with a Growth Hormone Releasing Peptide (GHRP). – GHRH Analogs (e.g. Sermorelin, CJC-1295, Tesamorelin) ∞ These peptides bind to the GHRH receptor on the pituitary. Their function is to increase the number of somatotrophs (the cells that produce GH) that release the hormone and the amount of GH each cell releases.
They effectively increase the strength of the natural GH pulse. – GHRPs / Ghrelin Mimetics (e.g. Ipamorelin, Hexarelin) ∞ These peptides bind to a different receptor, the growth hormone secretagogue receptor (GHS-R). Activating this receptor also initiates a pulse of GH release. When used together, these two classes of peptides create a powerful synergistic effect.
The GHRH analog loads the pituitary for a robust release, while the GHRP acts as the trigger. This dual-action approach can lead to a 3-5 fold increase in growth hormone release compared to using either peptide alone, all while preserving the natural, pulsatile rhythm of secretion that the body recognizes.
Peptide protocols work by restoring the natural, pulsatile release of growth hormone, which is critical for optimal metabolic function.

Visceral Fat the Metabolic Epicenter
One of the most significant long-term benefits of optimizing growth hormone levels is the targeted reduction of visceral adipose tissue (VAT). VAT is the fat stored deep within the abdominal cavity, surrounding vital organs.
It is metabolically active and acts like an endocrine organ itself, secreting inflammatory molecules (cytokines) and hormones that directly contribute to systemic inflammation, insulin resistance, and an increased risk of cardiovascular disease. Subcutaneous fat, the fat you can pinch under the skin, has a much lower metabolic impact.
Growth hormone has a potent lipolytic effect, meaning it promotes the breakdown of stored fats (triglycerides) into free fatty acids that can be used for energy. GH appears to preferentially target visceral adipocytes. Peptides like Tesamorelin have demonstrated a remarkable ability to reduce VAT.
Clinical studies, initially in HIV-positive patients with lipodystrophy, showed that Tesamorelin could significantly decrease VAT without majorly affecting subcutaneous fat. This targeted action is profoundly important for long-term metabolic health, as reducing VAT can lower inflammation, improve lipid profiles, and enhance insulin sensitivity. The reduction of this metabolically harmful fat is a primary mechanism through which GH peptides can produce lasting health improvements.
The table below compares the primary attributes of several key growth hormone peptides used in metabolic health protocols.
| Peptide | Class | Primary Mechanism | Primary Metabolic Target |
|---|---|---|---|
| Sermorelin | GHRH Analog | Stimulates natural, pulsatile GH release from the pituitary. | Overall restoration of GH levels, improving lean mass and fat metabolism. |
| CJC-1295 / Ipamorelin | GHRH Analog + GHRP | Synergistic action on two different pituitary receptors for a potent GH pulse. | Enhanced body composition, muscle growth, and fat loss. |
| Tesamorelin | GHRH Analog | Potent stimulation of GH release with high efficacy. | Targeted reduction of visceral adipose tissue (VAT). |
| MK-677 (Ibutamoren) | Oral GH Secretagogue | Mimics ghrelin to stimulate GH release; taken orally. | Sustained elevation of GH and IGF-1 for muscle mass and recovery. |

How Does Peptide Therapy Impact Insulin Sensitivity?
The relationship between growth hormone and insulin is complex. On one hand, GH can have a diabetogenic effect; it can antagonize insulin’s action in peripheral tissues, leading to a temporary increase in blood glucose levels. This occurs because the increase in free fatty acids resulting from GH-induced lipolysis can interfere with insulin signaling pathways. This is a critical consideration and is why protocols must be managed by a knowledgeable clinician who monitors metabolic markers.
On the other hand, the long-term metabolic benefits derived from peptide therapy often lead to a net improvement in insulin sensitivity. By significantly reducing visceral fat, the primary source of inflammatory signals that cause insulin resistance, the body’s cells become more responsive to insulin over time.
Furthermore, the increase in lean muscle mass, another effect of optimized GH levels, creates more tissue to take up glucose from the blood, further aiding glycemic control. The initial, transient effects on glucose are often outweighed by the substantial, lasting improvements in body composition and reduced inflammation.


Academic
An academic exploration of growth hormone peptides and their long-term metabolic impact requires a granular analysis of the underlying molecular biology and a critical appraisal of clinical trial data. The central question transitions from whether these peptides can improve metabolic health to how they achieve these effects on a cellular level and whether these effects are sustainable and safe over extended periods.
The dominant therapeutic pathway appears to be the targeted remodeling of adipose tissue, specifically the reduction of visceral adiposity. This process initiates a cascade of downstream benefits, including the modulation of systemic inflammation and a recalibration of insulin signaling, which collectively contribute to improved metabolic outcomes. A thorough examination must also confront the inherent complexities of the GH/IGF-1 axis, particularly its biphasic relationship with insulin sensitivity.

Growth Hormone Signalling and Adipose Tissue Remodeling
At the molecular level, growth hormone’s lipolytic action is mediated through its binding to the GH receptor on adipocytes. This event triggers a signaling cascade involving Janus kinase 2 (JAK2) and Signal Transducer and Activator of Transcription (STAT) proteins.
This pathway ultimately leads to the phosphorylation and activation of hormone-sensitive lipase (HSL), the rate-limiting enzyme in the hydrolysis of stored triglycerides into glycerol and free fatty acids (FFAs). The released FFAs are then transported to the liver and skeletal muscle to be used for energy through beta-oxidation.
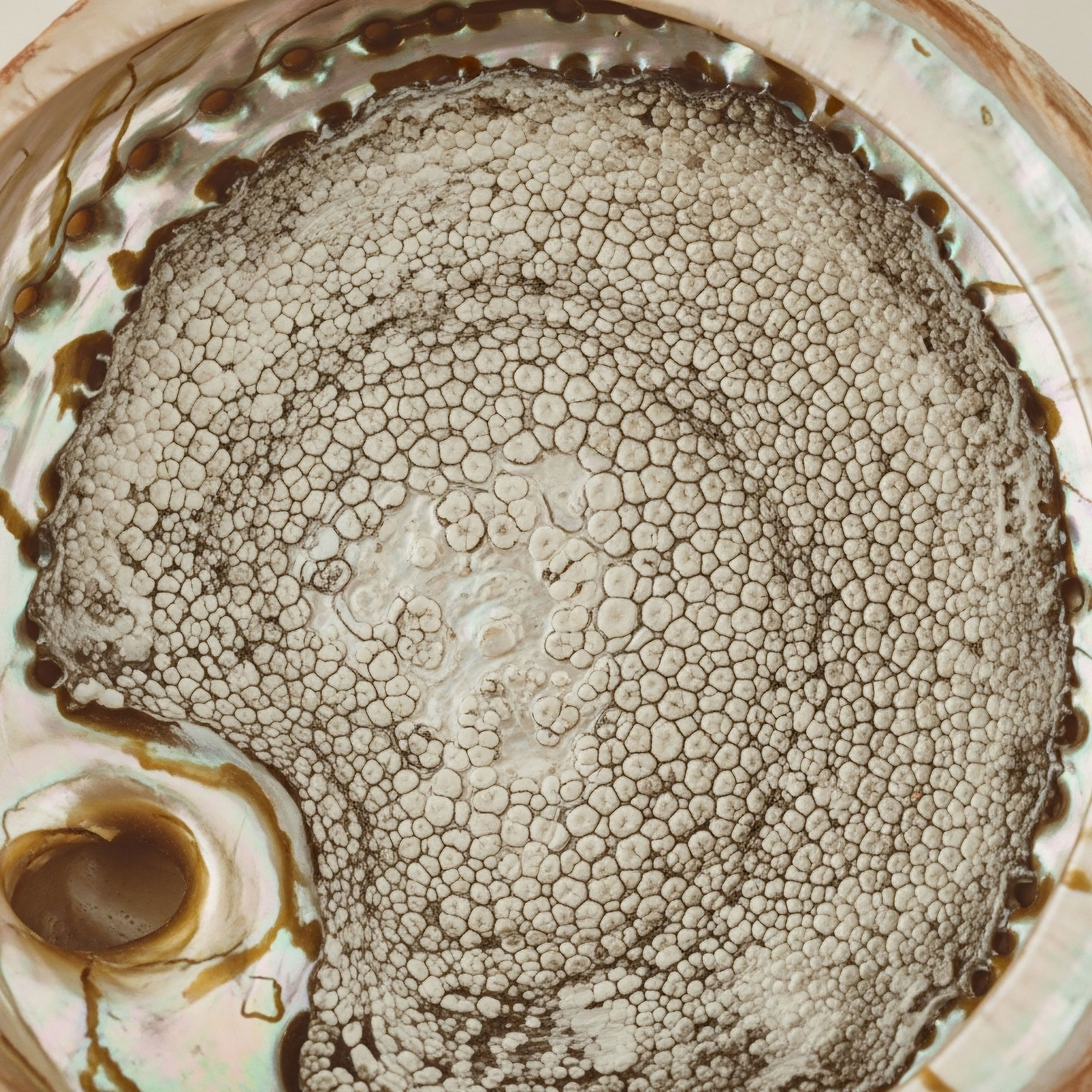
Research into peptides like Tesamorelin has revealed an even more sophisticated mechanism than simple fat reduction. Studies using CT scans to assess fat quality have shown that Tesamorelin not only reduces the quantity (area) of VAT but also increases its density. Higher fat density is associated with smaller, healthier adipocytes.
This suggests that the therapy promotes a remodeling of the adipose tissue itself, shifting it away from a hypertrophic, inflammatory state toward a healthier phenotype. This improvement in fat quality, independent of changes in fat quantity, is a significant finding and may be a key contributor to the observed metabolic benefits.

The Critical Role of Visceral Adipose Tissue in Metabolic Disease
Visceral adipose tissue is a primary driver of the pathophysiology of metabolic syndrome. Unlike subcutaneous fat, VAT is highly infiltrated with immune cells, such as macrophages, which in an obese state, adopt a pro-inflammatory profile.
These cells, along with the adipocytes themselves, secrete a host of adipokines and cytokines, including TNF-α, IL-6, and resistin, while reducing the secretion of the protective adipokine, adiponectin. This chronic, low-grade inflammatory state is a major contributor to the development of systemic insulin resistance, endothelial dysfunction, and non-alcoholic fatty liver disease (NAFLD).
Therapeutic interventions that selectively reduce VAT, therefore, strike at the root of metabolic dysregulation. Clinical trials involving Tesamorelin have provided robust evidence for this principle. A landmark study published in JAMA demonstrated that daily injections of Tesamorelin in HIV-infected patients with abdominal lipohypertrophy significantly reduced liver fat, a common comorbidity.
Subsequent research confirmed that this reduction in visceral and hepatic fat was associated with a favorable shift in metabolic syndrome classification, driven primarily by a decrease in waist circumference and triglyceride levels. More recent data has even shown that Tesamorelin can reduce the progression of liver fibrosis in patients with NAFLD, further underscoring the profound, long-term benefits of targeting VAT.
Clinical data shows that specific growth hormone peptides can reduce visceral fat quantity and improve its quality, directly mitigating a core driver of metabolic disease.
The following table summarizes key findings from select clinical trials, illustrating the quantitative impact of Tesamorelin on metabolic markers.
| Study Focus / Population | Key Finding | Metric | Source |
|---|---|---|---|
| HIV-associated Lipodystrophy | Tesamorelin significantly reduced visceral adipose tissue (VAT). | ~18% reduction in VAT over 26-52 weeks. | Stanley et al. The Journal of Clinical Endocrinology & Metabolism |
| HIV and Nonalcoholic Fatty Liver Disease (NAFLD) | Tesamorelin reduced liver fat content. | 35% of treated patients no longer classified as having NAFLD vs. 4% in placebo. | Stanley et al. The Lancet HIV |
| HIV and Metabolic Syndrome | Tesamorelin treatment was associated with a reversal of metabolic syndrome classification. | Prevalence of metabolic syndrome decreased significantly in responders. | Bedimo et al. Conference on Retroviruses and Opportunistic Infections |
| Fat Quality in People with HIV | Tesamorelin increased the density of both subcutaneous and visceral fat. | Significant increase in mean VAT density (HU), indicating improved fat quality. | Srinivasa et al. The Journal of Clinical Endocrinology & Metabolism |

Does Optimizing Growth Hormone Pose Long Term Risks?
A rigorous academic discussion must address the potential long-term risks associated with elevating GH and IGF-1 levels. The primary concern revolves around the mitogenic properties of IGF-1. As a potent growth factor, IGF-1 promotes cellular proliferation and inhibits apoptosis (programmed cell death).
Epidemiological studies have suggested a correlation between high-normal levels of IGF-1 and an increased risk of certain cancers, including prostate and breast cancer. It is important to contextualize this risk. Peptide therapies that work within the body’s physiological feedback loops, like Sermorelin, tend to keep IGF-1 levels within a healthy, youthful range, rather than pushing them to supraphysiological levels seen with high-dose synthetic HGH abuse.
Nonetheless, this remains an area of active research and is why these therapies are contraindicated in individuals with a history of active malignancy.
The second major consideration is the impact on glucose homeostasis. As established, GH can induce a state of insulin resistance. While the long-term net effect is often positive due to VAT reduction, it necessitates careful monitoring, especially in individuals with pre-existing glucose intolerance or type 2 diabetes.
The use of oral secretagogues like MK-677, which can cause a more sustained elevation of GH/IGF-1, may carry a higher risk of impacting insulin sensitivity over time compared to injectable peptides that produce more physiological pulses.
- Monitoring IGF-1 Levels ∞ It is standard clinical practice to monitor IGF-1 levels during peptide therapy to ensure they remain within an optimal, safe range, mitigating the theoretical risk associated with cellular proliferation.
- Assessing Glycemic Control ∞ Regular monitoring of fasting glucose, HbA1c, and insulin levels is crucial to manage any potential short-term diabetogenic effects of the therapy and to confirm long-term improvements in insulin sensitivity.
- Cardiovascular Health ∞ While the reduction of VAT and improvement in lipid profiles suggest a long-term cardiovascular benefit, ongoing monitoring of blood pressure and a comprehensive lipid panel is a cornerstone of responsible protocol management.
- Need for Further Research ∞ While the data for Tesamorelin in specific populations is robust, more long-term, large-scale studies are needed to fully characterize the effects of various peptide combinations on metabolic health outcomes in the general aging population.

References
- Grinspoon, S. K. et al. “Effects of Tesamorelin on Nonalcoholic Fatty Liver Disease in HIV-Infected Patients ∞ A Randomized, Double-Blind, Multicenter Trial.” JAMA, vol. 312, no. 4, 2014, pp. 380-389.
- Rathi, Kumar. “Ipamorelin + CJC 1295 Stack ∞ The Dynamic Duo.” Muscle and Brawn, 17 Jan. 2025.
- Bedimo, R. et al. “Tesamorelin Reverses Metabolic Syndrome and Improves Body Composition in HIV-infected Patients with Abdominal Fat Accumulation.” 30th Conference on Retroviruses and Opportunistic Infections (CROI), 2023.
- Srinivasa, S. et al. “Tesamorelin Improves Fat Quality Independent of Changes in Fat Quantity.” The Journal of Clinical Endocrinology & Metabolism, vol. 102, no. 11, 2017, pp. 4025-4034.
- Stanley, T. L. et al. “Tesamorelin for Nonalcoholic Fatty Liver Disease in HIV ∞ A Randomized, Double-Blind, Placebo-Controlled Trial.” The Lancet HIV, vol. 6, no. 12, 2019, pp. e823-e832.
- Møller, N. and J. O. L. Jørgensen. “Effects of Growth Hormone on Glucose, Lipid, and Protein Metabolism in Human Subjects.” Endocrine Reviews, vol. 30, no. 2, 2009, pp. 152-177.
- Vijayakumar, A. et al. “Effect of Growth Hormone on Insulin Signaling.” Journal of Molecular Endocrinology, vol. 61, no. 1, 2018, pp. R1-R13.
- Sigalos, J. T. and A. W. Pastuszak. “The Safety and Efficacy of Growth Hormone Secretagogues.” Sexual Medicine Reviews, vol. 6, no. 1, 2018, pp. 45-53.

Reflection
The information presented here offers a detailed map of the biological terrain connecting growth hormone peptides to metabolic health. It translates the silent, cellular conversations of your body into a language of mechanism and potential. This knowledge is a powerful tool, shifting your perspective from being a passenger in your own health journey to becoming an informed pilot.
The purpose of this deep exploration is to equip you with a new lens through which to view your body’s signals and a more sophisticated vocabulary to articulate your personal health narrative.
Consider the systems within you not as static components, but as a dynamic, interconnected network constantly adapting. The path to sustained vitality is paved with an understanding of these systems. This clinical science is the first step. The next is to ask how this information applies to your unique biological blueprint.
A truly personalized wellness protocol begins with this kind of informed introspection, followed by a collaborative dialogue with a trusted clinical guide. You possess the capacity to actively shape your long-term health, and that journey begins with understanding the profound intelligence already at work within you.

Glossary

body composition

endocrine system

growth hormone

pituitary gland

lean muscle mass

growth hormone peptides

metabolic health

adipose tissue

visceral fat

ghrh analog

sermorelin

ipamorelin

visceral adipose tissue

tesamorelin

peptide therapy

cjc-1295

insulin resistance

free fatty acids

insulin sensitivity

lipolysis

muscle mass

fat quality

metabolic syndrome

non-alcoholic fatty liver disease

hiv-infected patients with abdominal