

Fundamentals
You feel it in your bones, a quiet dimming of the lights. The energy that once propelled you through demanding days has been replaced by a persistent, draining fatigue. Your mental sharpness feels blunted, the clarity you once took for granted now elusive.
You might notice a subtle shift in your physique, a loss of muscle tone or a stubborn accumulation of body fat that resists your best efforts. These are not mere signs of aging to be passively accepted. They are signals from your body, a complex and intelligent system, indicating a disruption in its internal communication network.
Your lived experience of these symptoms is the most important data point we have. It is the starting point of a journey toward understanding the intricate biological symphony that governs your vitality.
At the heart of this symphony is your endocrine system, a sophisticated network of glands that produces and secretes hormones. Think of hormones as precise chemical messengers, traveling through your bloodstream to deliver specific instructions to every cell, tissue, and organ in your body.
They regulate everything from your metabolism and mood to your sleep cycles and sexual function. When this system is in perfect calibration, you feel it as a state of effortless well-being. When the signals become faint, distorted, or imbalanced, the consequences manifest as the very symptoms you are experiencing. The fatigue, the brain fog, the changes in body composition ∞ these are the direct results of a communication breakdown within your own biology.
Clinical therapies like Testosterone Replacement Therapy (TRT) or specific peptide treatments are powerful tools designed to address these communication breakdowns directly. TRT, for instance, replenishes levels of a key messenger, testosterone, restoring its vital signals throughout the body.
Peptide therapies, composed of short chains of amino acids, can act as highly specific keys, unlocking particular cellular functions like tissue repair or the release of your own growth hormone. These interventions are analogous to repairing a critical line of communication in a vast network. They are precise, effective, and grounded in decades of clinical science. Their purpose is to restore a specific, measurable deficiency in the system, bringing a vital messenger back online.
A participatory wellness approach transforms the body from a passive recipient of treatment into an active, thriving environment where clinical therapies can achieve their maximum potential.
A participatory wellness approach represents a profound shift in perspective. It recognizes that for these clinical interventions to be truly successful, the entire system must be optimized to receive and act upon their signals. It is about cultivating an internal environment where these hormonal messengers can perform their duties without interference.
Imagine sending a critical message through a network filled with static and noise. The message may be sent, but its reception will be poor, and its impact diminished. A participatory approach is the systematic process of clearing that static.
It involves a conscious and sustained effort to manage the foundational pillars of health that govern your body’s overall receptivity to hormonal signaling. These pillars are not abstract concepts; they are the tangible, daily inputs that dictate your biological reality ∞ the nutrients you consume, the quality of your sleep, the way you manage stress, and the physical demands you place on your body.
This is where your active participation becomes the most critical component of your therapeutic success. Your daily choices directly influence the cellular environment in which hormones operate. For example, chronic inflammation, often driven by dietary choices, can blunt the sensitivity of hormone receptors, making them less responsive to the signals from TRT or peptides.
Poor sleep can disrupt the natural rhythms of hormone release, creating a chaotic internal environment that works against the stability you are trying to achieve. Chronic stress elevates cortisol, a hormone that can directly interfere with testosterone production and function. By actively managing these factors, you are doing more than just living a “healthy lifestyle.” You are engaging in a sophisticated form of biological optimization. You are preparing the soil so the seeds of clinical therapy can flourish.
This integrated model is about building a robust biological foundation that supports and amplifies the effects of your clinical treatment. It is a partnership between targeted medical science and your own informed, daily actions. The goal is a state of health that is resilient, vibrant, and sustainable.
It is about reclaiming your vitality and function, not as a temporary fix, but as a new, elevated baseline of well-being that you have helped to create. This journey begins with understanding that your symptoms are real, they have a biological basis, and you possess a remarkable capacity to influence that biology.

The Language of Hormones
To fully appreciate the synergy between clinical therapies and participatory wellness, one must first understand the language of hormones. This language is not spoken in words, but in molecules, feedback loops, and receptor interactions. Hormones are the body’s primary regulators, the conductors of an orchestra playing the music of your physiology.
Each hormone has a specific role, a unique instrument to play. Testosterone, for example, is a powerful conductor of anabolic processes, directing the building of muscle and bone, influencing libido, and maintaining cognitive function. Growth hormone is the master of cellular regeneration and repair. Insulin governs the flow of energy into cells. The coordinated action of these and hundreds of other hormones creates the seamless experience of health.
These messengers operate within a system of exquisite balance, maintained by a process called homeostasis. The body is constantly monitoring its internal state and making adjustments to keep key parameters within a narrow, optimal range. This is achieved through feedback loops, primarily negative feedback loops. Think of the thermostat in your home.
When the temperature rises above the set point, the air conditioning turns on. When it cools down, the system shuts off. The endocrine system works in a similar fashion. For example, the Hypothalamic-Pituitary-Gonadal (HPG) axis governs testosterone production. When testosterone levels are low, the hypothalamus releases Gonadotropin-Releasing Hormone (GnRH).
This signals the pituitary gland to release Luteinizing Hormone (LH), which in turn signals the testes to produce more testosterone. As testosterone levels rise, they send a signal back to the hypothalamus and pituitary to slow down the production of GnRH and LH. This elegant loop ensures that testosterone levels are kept in balance.
When we introduce an external therapy like TRT, we are intervening in this feedback loop. By providing an external source of testosterone, we are ensuring that the body’s tissues receive the necessary signal. However, this intervention can also cause the natural production system to down-regulate.
This is why a comprehensive TRT protocol often includes medications like Gonadorelin or Enclomiphene, which are designed to stimulate the body’s own signaling pathways and maintain the health of the HPG axis. This illustrates a core principle ∞ effective hormonal therapy is about intelligently integrating with the body’s existing systems, not just overriding them.

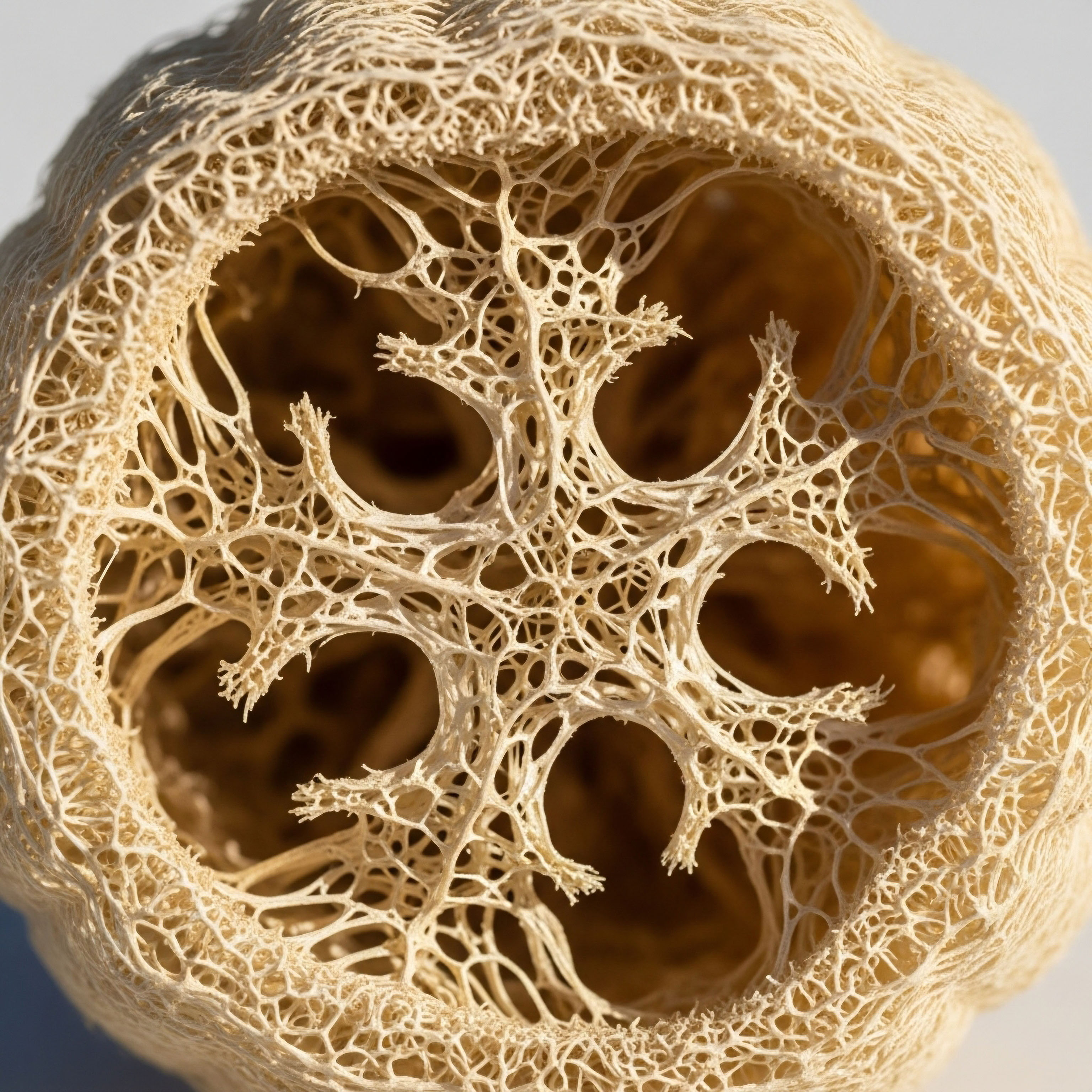
Hormone Receptors the Locks to the Cellular Kingdom
The action of a hormone is ultimately determined by its ability to bind to a specific receptor on or inside a cell. A hormone is like a key, and a receptor is the lock. When the key fits the lock, it opens a door, initiating a specific action within the cell.
A cell can have thousands of receptors for a particular hormone. The number and sensitivity of these receptors are not static. They can be up-regulated (increased) or down-regulated (decreased) based on a variety of factors. This is a critical concept for understanding the power of a participatory wellness approach.
Your lifestyle choices have a profound impact on receptor sensitivity. For instance, chronic high insulin levels, often a result of a diet high in refined carbohydrates and sugars, can lead to insulin resistance. This is a state where the insulin receptors on your cells become less sensitive to the effects of insulin.
The pancreas has to produce more and more insulin to get the same job done, eventually leading to metabolic dysfunction. A similar principle applies to other hormonal systems. Chronic inflammation, oxidative stress, and nutrient deficiencies can all impair the function of hormone receptors, making your body less responsive to the hormones it produces naturally, as well as those provided through therapy.
Conversely, a participatory wellness approach can enhance receptor sensitivity. Regular exercise has been shown to increase the sensitivity of insulin receptors. A diet rich in anti-inflammatory foods and essential nutrients provides the building blocks for healthy receptors and reduces the inflammatory “noise” that can interfere with their function.
Adequate sleep and stress management help to regulate cortisol levels, which can positively influence the sensitivity of receptors for other hormones like testosterone. By optimizing your lifestyle, you are essentially polishing the locks, ensuring that the hormonal keys provided by your clinical therapy can work as efficiently and effectively as possible. You are creating a biological environment that is primed for success.


Intermediate
Advancing beyond the foundational understanding of hormonal communication, we arrive at the practical application of a participatory wellness strategy. This is where we translate knowledge into action, building a synergistic framework where clinical interventions like TRT and peptide therapies are not merely supported, but actively potentiated by your daily choices.
The success of these advanced clinical protocols is contingent upon the physiological environment in which they operate. A body burdened by inflammation, insulin resistance, or chronic stress is a body that will mount a suboptimal response to even the most precisely calibrated therapeutic regimen. Therefore, a participatory approach is the active cultivation of a high-performance biological terrain.
This cultivation is a multi-faceted process, addressing the core pillars of metabolic health, physical conditioning, recovery, and stress modulation. Each of these pillars represents a powerful lever that you can pull to amplify the benefits of your clinical therapy, mitigate potential side effects, and achieve a more profound and sustainable level of well-being.
We will now explore the specific mechanisms through which these participatory strategies interface with TRT and peptide treatments, moving from the theoretical to the tangible. This is the blueprint for building a body that is not just treated, but truly optimized.

Nutritional Architecture for Hormonal Efficacy
Nutrition is the cornerstone of your participatory wellness protocol. The food you consume provides the raw materials for hormone production, the cofactors for enzymatic reactions, and the signaling molecules that modulate inflammation and cellular health.
When you are on a therapy like TRT, your nutritional strategy should be designed to maximize the anabolic potential of testosterone while simultaneously managing its potential metabolic consequences, such as changes in lipid profiles or estrogen levels. For those utilizing peptide therapies, nutrition plays a vital role in providing the amino acid building blocks for tissue repair and supporting the metabolic shifts initiated by these powerful signaling molecules.
A primary objective of your nutritional architecture is the management of insulin sensitivity. Insulin and testosterone have a complex, bidirectional relationship. High levels of circulating insulin, a condition often preceding or accompanying insulin resistance, can suppress the production of Sex Hormone-Binding Globulin (SHBG). SHBG is a protein that binds to testosterone in the bloodstream.
When SHBG is low, more testosterone is “free” or bioavailable, which might seem beneficial. However, this state is often associated with the broader metabolic dysfunction of insulin resistance, which can increase inflammation and aromatization (the conversion of testosterone to estrogen).
A diet centered around whole, unprocessed foods, with a controlled intake of refined carbohydrates and an emphasis on high-quality protein, healthy fats, and abundant fiber from vegetables, is fundamental to maintaining insulin sensitivity. This dietary pattern helps to stabilize blood sugar levels, reduce the demand for insulin, and create a metabolic environment conducive to optimal testosterone action.
Strategic nutrition provides the essential building blocks and metabolic stability required for hormone therapies to function optimally.
Furthermore, specific micronutrients are critical for hormonal health. Zinc is an essential mineral for testosterone production. Magnesium is involved in hundreds of enzymatic reactions, including those related to sleep and stress management, which indirectly influence hormonal balance. Vitamin D, technically a pro-hormone, plays a crucial role in both testosterone production and immune function.
A diet rich in a variety of colorful plants, lean proteins, and healthy fats will provide a broad spectrum of these vital nutrients. In some cases, targeted supplementation, guided by blood work and clinical assessment, may be necessary to correct deficiencies and further optimize the system. The goal is to create a state of nutrient sufficiency, providing your body with all the tools it needs to execute the instructions delivered by your clinical therapy.

The Role of Macronutrients in a Therapeutic Context
When undergoing hormonal optimization, the strategic allocation of macronutrients ∞ protein, carbohydrates, and fats ∞ becomes a powerful tool for directing therapeutic outcomes. Each macronutrient has a distinct impact on the endocrine system.
- Protein ∞ Adequate protein intake is paramount, especially when on TRT or muscle-building peptide protocols. Testosterone is an anabolic hormone; it signals your body to synthesize new proteins and build muscle tissue. To execute this command, your body needs a sufficient supply of amino acids, the building blocks of protein. Consuming a consistent intake of high-quality protein from sources like lean meats, fish, eggs, and legumes provides the necessary substrate for muscle protein synthesis, allowing you to fully capitalize on the anabolic signals of your therapy. A general guideline for active individuals seeking to build muscle is 1.6-2.2 grams of protein per kilogram of body weight.
- Fats ∞ Dietary fats, particularly saturated and monounsaturated fats, are the direct precursors to steroid hormones, including testosterone. Cholesterol is the foundational molecule from which all steroid hormones are synthesized. A diet that is overly restrictive in fat can compromise the body’s natural ability to produce these vital messengers. Healthy fat sources like avocados, olive oil, nuts, and seeds also play a crucial role in managing inflammation and supporting cell membrane health, which is essential for proper receptor function. Omega-3 fatty acids, found in fatty fish like salmon, are particularly important for their potent anti-inflammatory properties.
- Carbohydrates ∞ The role of carbohydrates is more nuanced and should be personalized based on your activity level and metabolic health. For highly active individuals, carbohydrates are a vital source of fuel for high-intensity exercise and help to replenish glycogen stores, which is important for recovery and performance. They also have a protein-sparing effect, ensuring that dietary protein is used for tissue repair rather than being converted to glucose for energy. However, for individuals with underlying insulin resistance, a more measured approach to carbohydrate intake is warranted. Focusing on complex, high-fiber carbohydrate sources like root vegetables, legumes, and whole grains, and timing their consumption around workouts, can help to manage the insulin response and support metabolic flexibility.

Exercise as a Synergistic Intervention
Physical activity is a potent modulator of the endocrine system. It is one of the most effective participatory strategies for enhancing the outcomes of TRT and peptide therapies. The right type of exercise can improve body composition, enhance insulin sensitivity, boost mood, and even amplify the specific effects of your clinical protocol. The relationship between exercise and hormonal therapy is synergistic; each makes the other more effective.
Resistance training, in particular, is a powerful partner to TRT. Testosterone promotes muscle protein synthesis, but this process is significantly amplified when it is combined with the mechanical stimulus of lifting weights. The micro-trauma induced by resistance exercise signals a cascade of cellular repair and growth processes.
Testosterone acts as a powerful accelerant for this process, leading to greater gains in muscle mass and strength than would be achieved with either intervention alone. These gains in lean muscle mass are not just for aesthetics; muscle is a highly metabolically active tissue.
The more muscle you have, the more glucose you can dispose of, which improves insulin sensitivity and overall metabolic health. A well-structured resistance training program, focusing on compound movements that engage multiple muscle groups, is a non-negotiable component of a successful TRT protocol.
For those using growth hormone-releasing peptides like Sermorelin or Ipamorelin/CJC-1295, exercise provides a complementary stimulus for growth hormone (GH) release. High-intensity interval training (HIIT) and resistance training have both been shown to be potent natural stimulators of GH secretion.
By timing the administration of your peptide therapy in conjunction with your workout schedule (for example, taking it before bed on a training day), you can create a more robust and prolonged elevation of GH and its downstream effector, Insulin-Like Growth Factor 1 (IGF-1). This can lead to enhanced recovery, improved body composition, and greater benefits from the peptide therapy.
The table below outlines how different types of exercise can be strategically paired with specific therapeutic goals.
| Exercise Modality | Primary Physiological Effect | Synergy with Clinical Therapies |
|---|---|---|
| Resistance Training (Strength) |
Increases muscle protein synthesis, improves neuromuscular efficiency, enhances bone density. |
Maximizes the anabolic effects of TRT for muscle and strength gains. Increases metabolic rate, supporting fat loss goals with peptides like Tesamorelin. |
| High-Intensity Interval Training (HIIT) |
Potent stimulus for natural growth hormone release, improves cardiovascular fitness, enhances insulin sensitivity. |
Amplifies the effects of growth hormone secretagogues (Sermorelin, Ipamorelin). Improves metabolic flexibility, complementing the effects of TRT on body composition. |
| Zone 2 Cardio (Endurance) |
Improves mitochondrial function and density, enhances fat oxidation, lowers resting heart rate. |
Builds a robust aerobic base, improving recovery capacity between intense workouts. Supports cardiovascular health, an important consideration for long-term TRT. |
| Mobility and Flexibility Work |
Improves joint range of motion, reduces risk of injury, aids in recovery. |
Supports the ability to perform resistance training safely and effectively. Complements the healing and regenerative effects of peptides like BPC-157. |

The Critical Role of Sleep and Circadian Rhythm
Sleep is a foundational biological process during which the body undergoes intense periods of repair, consolidation, and hormonal regulation. It is a non-negotiable pillar of any participatory wellness program, and its importance is magnified when undergoing hormonal therapy.
The majority of our key anabolic hormones, including testosterone and growth hormone, are released in a pulsatile manner during the deep stages of sleep. Disruptions to sleep quality or quantity can severely blunt these crucial hormonal surges, effectively working against the goals of your therapy.
The master clock that governs our sleep-wake cycle is the circadian rhythm, a roughly 24-hour internal cycle that is synchronized primarily by light exposure. Maintaining a regular sleep schedule, even on weekends, helps to anchor this rhythm.
Exposure to bright light, preferably sunlight, in the morning helps to reinforce a strong wakefulness signal and properly time the release of melatonin later in the evening. Conversely, minimizing exposure to bright, blue-spectrum light from screens in the hours before bed is critical for allowing melatonin to rise and facilitate the transition to sleep. These practices, often referred to as sleep hygiene, are not trivial; they are a form of direct circadian entrainment.
For an individual on TRT, optimizing sleep can enhance feelings of well-being and energy that the therapy provides. For someone using growth hormone-releasing peptides, deep sleep is the window of opportunity during which these peptides can exert their maximum effect on the pituitary gland.
A participatory approach to sleep involves creating a sanctuary for rest. This includes a cool, dark, and quiet bedroom, a relaxing pre-bed routine, and a commitment to obtaining 7-9 hours of quality sleep per night. It is an active investment in the restorative processes that allow your body to rebuild and respond to therapeutic inputs.


Academic
A sophisticated analysis of the synergy between participatory wellness and clinical hormonal therapies requires a departure from simplistic, linear models of cause and effect. We must adopt a systems-biology perspective, recognizing the human body as a complex, interconnected network of systems.
The efficacy of an exogenous therapeutic agent, be it testosterone or a synthetic peptide, is not determined in a vacuum. Its ultimate physiological impact is a product of its interaction with the entirety of the host’s biological milieu.
This section will delve into the intricate crosstalk between the Hypothalamic-Pituitary-Gonadal (HPG) axis, the primary target of TRT, and the Hypothalamic-Pituitary-Adrenal (HPA) axis, the central governor of the stress response. It is within the nexus of this interaction that the profound influence of participatory wellness protocols can be most clearly elucidated.
The HPG and HPA axes are two of the most fundamental neuroendocrine systems in the body. They are deeply intertwined, sharing anatomical proximity in the hypothalamus and pituitary, and exhibiting complex reciprocal regulation. The HPA axis, when activated by a perceived stressor (be it psychological, physical, or inflammatory), initiates a cascade culminating in the release of cortisol from the adrenal glands.
Cortisol is a glucocorticoid hormone essential for life, playing critical roles in metabolism and immune function. However, chronic activation of the HPA axis and the resultant sustained elevation of cortisol can exert a potent inhibitory influence on the HPG axis at multiple levels. This inhibitory crosstalk is a key mechanism through which a poorly managed lifestyle can undermine the intended benefits of hormonal therapies and, in some cases, contribute to the very condition being treated.

The Neuroendocrine Mechanisms of HPA-HPG Crosstalk
The inhibitory effect of HPA axis hyperactivity on the HPG axis is mediated by several distinct mechanisms. Understanding these pathways is crucial for appreciating why stress modulation is a clinical necessity, not a lifestyle luxury, in the context of hormonal optimization.
- Suppression of GnRH Release ∞ Corticotropin-Releasing Hormone (CRH), the principal initiator of the HPA axis cascade released from the hypothalamus, has been shown to directly inhibit the release of Gonadotropin-Releasing Hormone (GnRH). GnRH is the apex hormone of the HPG axis, providing the primary stimulus for the pituitary to release LH and FSH. By suppressing GnRH, chronic stress effectively turns down the master signal for endogenous testosterone production. While an individual on a TRT protocol is receiving exogenous testosterone, this suppression of the upstream signaling pathway can still contribute to testicular desensitization and a more challenging clinical picture, particularly if future restoration of endogenous function is a goal.
- Pituitary Inhibition ∞ Glucocorticoids, like cortisol, can act directly on the pituitary gland to reduce its sensitivity to GnRH. This means that even if GnRH is released, the pituitary’s response in terms of LH and FSH secretion is blunted. This further dampens the endogenous steroidogenic drive.
- Direct Testicular Inhibition ∞ There is evidence to suggest that elevated cortisol levels can have a direct inhibitory effect on the Leydig cells within the testes, impairing their ability to produce testosterone in response to LH stimulation. This represents a third level of HPG axis suppression.
- Alterations in SHBG and Bioavailability ∞ Chronic stress and elevated cortisol can influence liver function, potentially altering the production of Sex Hormone-Binding Globulin (SHBG). While the effects can be complex, changes in SHBG levels directly impact the amount of free, bioavailable testosterone.
This multi-level suppression of the HPG axis by a chronically activated HPA axis provides a compelling biological rationale for the integration of stress-modulating practices into any hormonal optimization protocol. Participatory wellness strategies such as mindfulness meditation, breathwork, and adequate sleep are not merely “stress relievers”; they are targeted interventions designed to down-regulate HPA axis hyperactivity and thereby reduce the inhibitory tone on the HPG axis. They create a neuroendocrine environment that is permissive for optimal androgen signaling.
The chronic activation of the body’s stress response system can directly suppress the very hormonal pathways that clinical therapies aim to support.

Inflammation as a Mediator of Hormonal Resistance
Another critical area where participatory wellness exerts a profound influence is in the modulation of systemic inflammation. Chronic, low-grade inflammation is a pervasive feature of modern lifestyles, driven by factors such as a diet high in processed foods, sedentary behavior, poor sleep, and chronic stress.
This inflammatory state can be conceptualized as a form of biological “noise” that interferes with the clear transmission of hormonal signals. The mechanisms through which inflammation disrupts hormonal function are multifaceted and highly relevant to both TRT and peptide therapies.
Inflammation can induce a state of “hormone resistance,” analogous to the well-understood phenomenon of insulin resistance. Pro-inflammatory cytokines, such as Tumor Necrosis Factor-alpha (TNF-α) and Interleukin-6 (IL-6), can interfere with the downstream signaling pathways activated by hormone-receptor binding.
For example, they can phosphorylate key intracellular signaling molecules in a way that inhibits the normal cellular response to testosterone or IGF-1. This means that even with adequate levels of the hormone in the bloodstream (whether endogenous or exogenous), the target tissues are unable to respond appropriately. The clinical manifestation is a blunted therapeutic effect, where a patient’s lab values may look optimal, but their subjective experience of symptoms does not improve as expected.
Furthermore, inflammation can directly impact hormone metabolism. The enzyme aromatase, which converts testosterone to estradiol, is known to be up-regulated by inflammatory cytokines, particularly in adipose tissue. An individual with high levels of systemic inflammation and excess adiposity may experience a higher rate of aromatization while on TRT, leading to an unfavorable testosterone-to-estrogen ratio and potential side effects like gynecomastia and water retention.
A participatory wellness program focused on an anti-inflammatory diet (rich in omega-3 fatty acids, polyphenols, and fiber), regular exercise (which has potent anti-inflammatory effects), and stress reduction directly targets the root cause of this inflammatory milieu. By reducing the systemic inflammatory load, these strategies can enhance hormone receptor sensitivity and promote a more favorable metabolic fate for the hormones being administered.
The table below summarizes the impact of key inflammatory markers on hormonal pathways, highlighting the importance of an anti-inflammatory lifestyle.
| Cytokine | Source/Stimulus | Impact on HPG/HPA Axis and Hormone Action |
|---|---|---|
| TNF-α (Tumor Necrosis Factor-alpha) |
Adipose tissue, macrophages. Stimulated by endotoxin, infection, metabolic dysfunction. |
Can suppress GnRH release. Induces insulin resistance. May impair Leydig cell function. Interferes with intracellular signaling pathways for androgens and IGF-1. |
| IL-6 (Interleukin-6) |
Immune cells, adipose tissue, muscle (during exercise). Chronically elevated in obesity and inflammatory states. |
Stimulates HPA axis and CRH release, leading to elevated cortisol. Can up-regulate aromatase activity in fat cells. Has complex, context-dependent effects on hormonal systems. |
| CRP (C-Reactive Protein) |
Produced by the liver in response to IL-6. A key clinical marker of systemic inflammation. |
While not directly acting on hormonal pathways, elevated CRP is a strong indicator of an inflammatory state that is associated with lower testosterone levels and blunted response to therapies. |

How Do Peptides Interact with This Complex System?
The interaction of therapeutic peptides with this integrated neuroendocrine-immune system is a frontier of clinical science. Many peptides have pleiotropic effects, meaning they influence multiple biological pathways simultaneously. For example, BPC-157, a peptide known for its remarkable tissue-healing properties, has also been shown in preclinical models to have a modulating effect on the HPA axis and to protect against stress-induced gastric lesions.
This suggests that its therapeutic benefits may extend beyond simple structural repair to include a more systemic, homeostatic-restoring function.
Growth hormone secretagogues like Ipamorelin and CJC-1295 stimulate the release of GH, which in turn stimulates the production of IGF-1. IGF-1 is a powerful anabolic and neuroprotective molecule. However, the biological activity of IGF-1 is itself modulated by the inflammatory state of the body.
In a highly inflammatory environment, the binding proteins that regulate IGF-1 bioavailability can be altered, and the sensitivity of the IGF-1 receptor can be impaired. Therefore, the full regenerative potential of these peptides can only be realized in a biological environment that has been optimized through participatory wellness strategies. An anti-inflammatory lifestyle creates a permissive canvas upon which these peptides can paint their restorative masterpiece.
Ultimately, a participatory wellness approach is a form of applied systems biology. It is the recognition that the human body is a complex adaptive system, and that any intervention, clinical or otherwise, will have effects that ripple throughout the entire network.
By optimizing the foundational pillars of nutrition, exercise, sleep, and stress, we are not merely supporting our clinical therapies. We are fundamentally changing the operating parameters of the system, creating a state of resilience, receptivity, and enhanced therapeutic potential. It is the most sophisticated and personalized form of medicine imaginable.
References
- Vingren, J. L. et al. “Testosterone physiology in resistance exercise and training.” Sports Medicine, vol. 40, no. 12, 2010, pp. 1037-53.
- Carro, E. et al. “The role of insulin-like growth factor I in the molecular cascade of neuroprotection.” Growth Hormone & IGF Research, vol. 12, no. 4, 2002, pp. 193-8.
- Kyrou, I. and C. Tsigos. “Stress hormones ∞ physiological stress and regulation of metabolism.” Current Opinion in Pharmacology, vol. 9, no. 6, 2009, pp. 787-93.
- Grossmann, M. and B. B. M. Kumar. “The role of testosterone in the age-related metabolic syndrome.” Current Opinion in Endocrinology, Diabetes and Obesity, vol. 17, no. 3, 2010, pp. 247-54.
- Sinner, J. M. et al. “The role of inflammation in the pathogenesis of hypogonadism in the aging male.” The Journal of Steroid Biochemistry and Molecular Biology, vol. 127, no. 1-2, 2011, pp. 59-65.
- Raharjo, B. and P. J. Fuller. “Glucocorticoid and mineralocorticoid receptor signaling ∞ a story of complexity.” Journal of Endocrinology, vol. 241, no. 2, 2019, pp. T1-T13.
- Traish, A. M. et al. “The dark side of testosterone deficiency ∞ I. Metabolic syndrome and erectile dysfunction.” Journal of Andrology, vol. 30, no. 1, 2009, pp. 10-22.
- Sigalos, J. T. and A. W. Pastuszak. “The safety and efficacy of growth hormone secretagogues.” Sexual Medicine Reviews, vol. 6, no. 1, 2018, pp. 45-53.
- Walker, R. F. “Sermorelin ∞ a better approach to management of adult-onset growth hormone insufficiency?” Clinical Interventions in Aging, vol. 1, no. 4, 2006, pp. 307-8.
- Tilg, H. and A. R. Moschen. “Adipocytokines ∞ mediators linking adipose tissue, inflammation and immunity.” Nature Reviews Immunology, vol. 6, no. 10, 2006, pp. 772-83.

Reflection
You have now traveled through the intricate biological landscapes that govern your vitality. You have seen how the precise signals of clinical therapies can be amplified and clarified by your own conscious actions. This knowledge is a powerful instrument. It shifts the dynamic from one of passive treatment to one of active, informed partnership with your own physiology.
The path forward is one of continuous discovery, a personal exploration of the inputs that allow your unique biology to function at its highest potential. What you have learned here is the map; the journey itself is yours to navigate. The ultimate goal is a state of health that feels authentic and sustainable, a vitality that is not just restored, but truly reclaimed.

What Is the Next Step on Your Personal Health Journey?
The information presented here provides a framework for understanding the profound connection between your daily habits and the effectiveness of advanced medical treatments. The next step involves translating this understanding into a personalized protocol. This requires a deep and honest assessment of your own life. Where are the areas of greatest friction?
Is it nutrition, sleep, stress, or movement? Acknowledging these challenges is the first step toward addressing them. This process is one of self-experimentation and observation, guided by data from both lab work and your own subjective experience. It is a commitment to becoming the foremost expert on your own body.

Building Your Personal Therapeutic Alliance
This journey is best undertaken with a trusted clinical partner who understands and values this integrated approach. A therapeutic alliance is a collaborative effort between you, your physician, and your own biology. It is a dynamic process of setting goals, implementing strategies, measuring outcomes, and refining the approach based on the feedback your body provides.
The science provides the principles, but you provide the context. Your lived experience, your goals, and your commitment to the process are the catalysts that transform a clinical protocol into a truly personalized path to wellness. The power to influence your health is, and always has been, within you. The knowledge you have gained is simply the key to unlocking it.



